Normal Physical Exam Template
Explore a comprehensive guide to a normal physical exam. Learn about key components, procedures, and documentation tips to enhance patient care and assessment.


What is a physical examination?
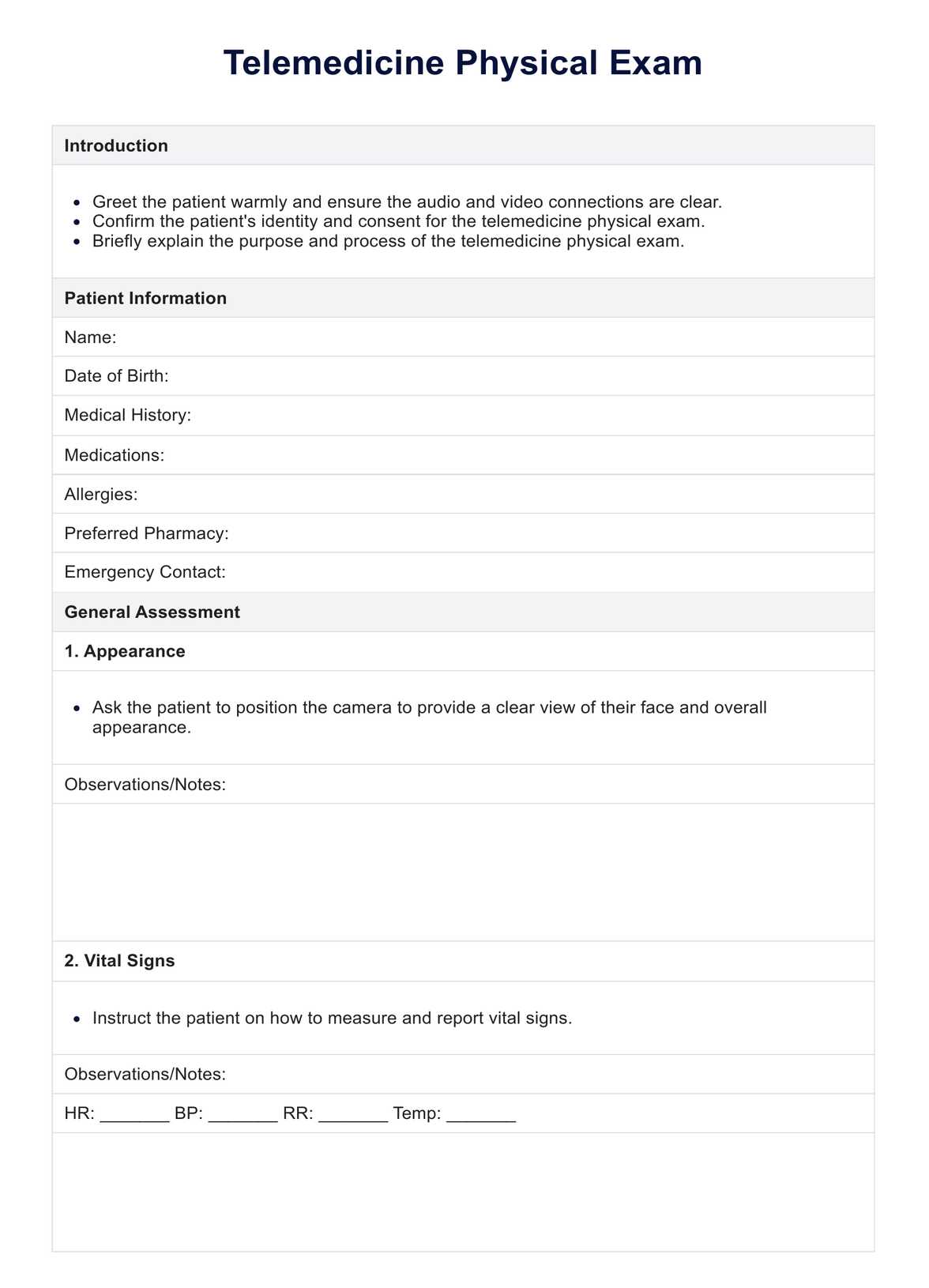
A physical examination is a crucial component of patient assessment and medical care. It involves a healthcare provider systematically evaluating a patient's body systems to gather objective data about their health status and the patient's health status. A physical exam aims to identify any signs of disease, injury, or abnormality that may require further investigation or treatment (Garibaldi & Elder, 2021).
The healthcare provider uses various techniques to assess the patient's overall health and specific body systems during a physical examination. This information also helps inform the patient's treatment plan.
Different parts of a physical exam
A physical exam is a comprehensive assessment of a patient's health. Here's a breakdown of the critical components:
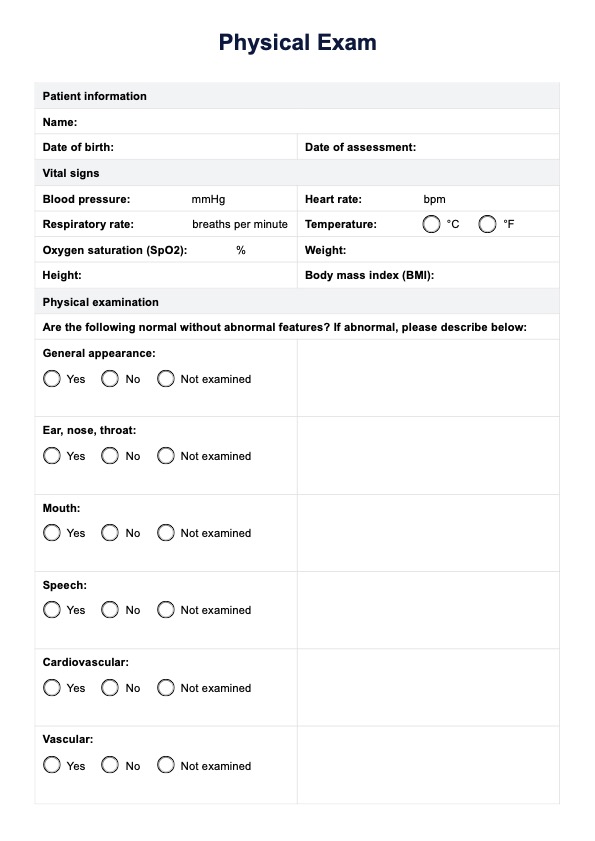
- Vital signs: Blood pressure, heart rate, respiratory rate, and temperature provide a baseline health assessment.
- Physical appearance and mental status: This includes observing mood, affect, and communication ability.
- Skin, hair, and nails: Examined for color, texture, moisture, and abnormalities like rashes or lesions.
- Head, eyes, ears, nose, and throat (HEENT): Checks head for trauma, visual acuity, ears, nose, throat, and oral health.
- Neck and lymph nodes: Palpated for tenderness, stiffness, or enlarged lymph nodes. The thyroid gland is also assessed.
- Chest and lungs: The chest wall is inspected for symmetry and signs of deformity. Lungs are auscultated for breath sounds.
- Cardiovascular system: Pulses are checked for rate, rhythm, and quality, and the heart is listened to for abnormal sounds.
- Abdomen: Inspected for contour, symmetry, and masses. Bowel sounds are auscultated, and the abdomen is palpated for tenderness or masses. The liver and spleen are assessed.
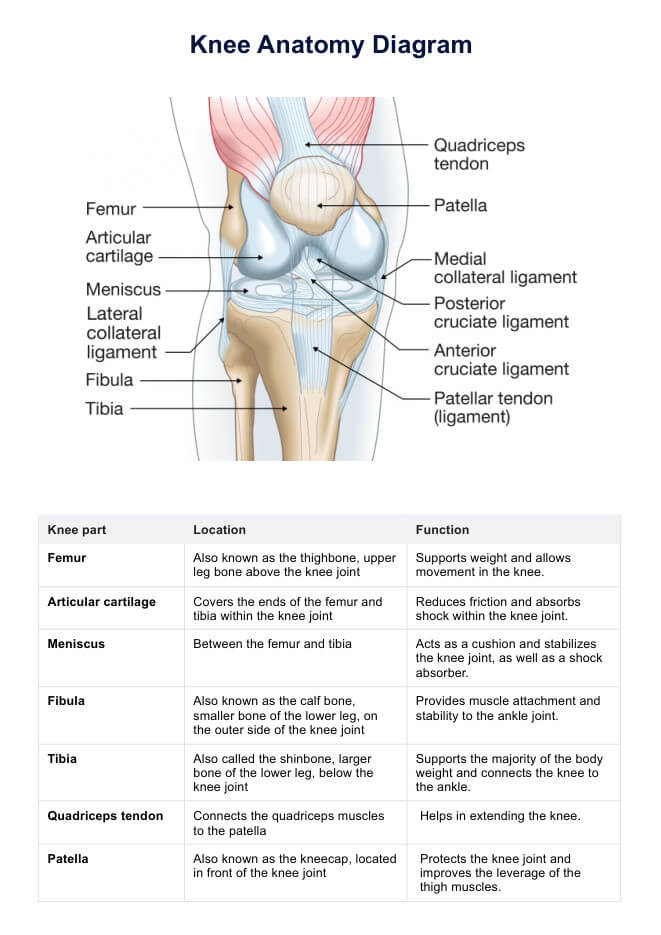
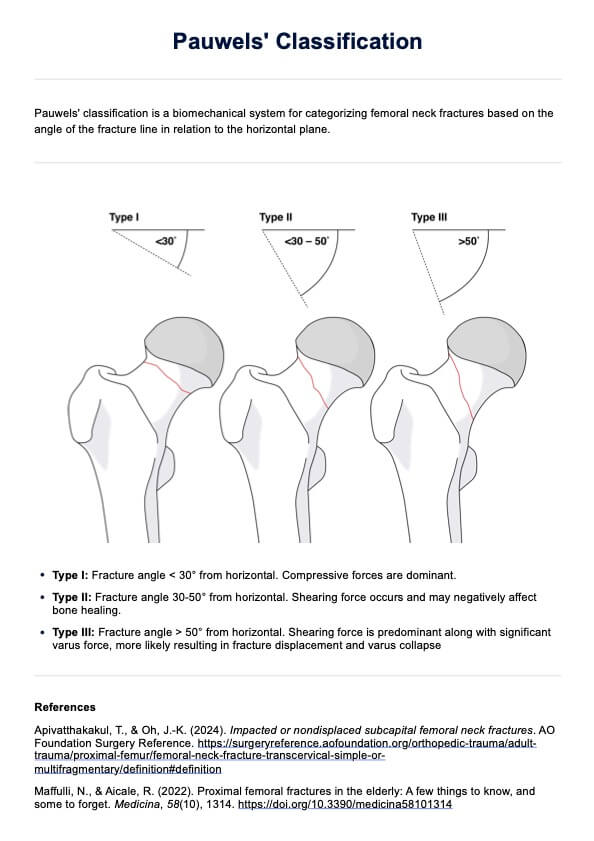
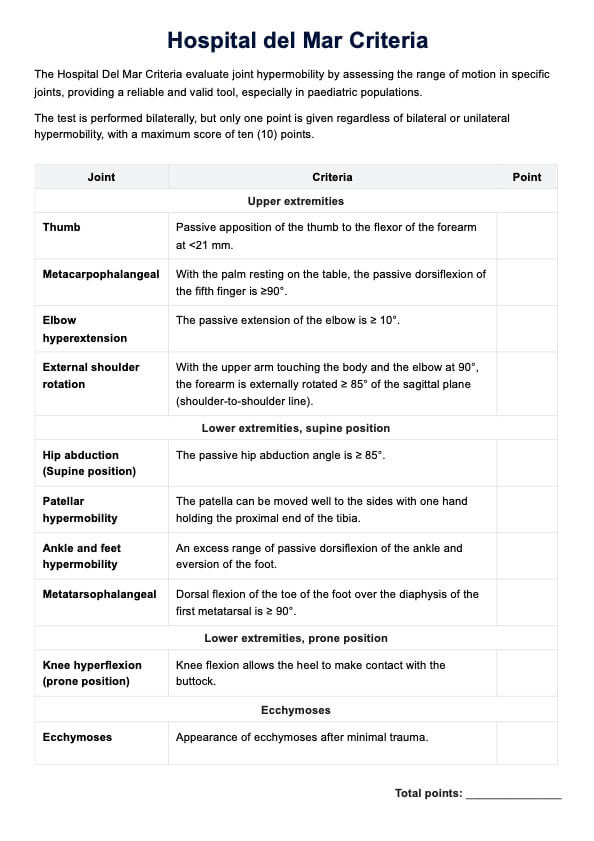
- Musculoskeletal system: The upper and lower extremities' muscle strength, normal gait, tone, and symmetry are evaluated. The range of motion of major joints is assessed for limitations, pain, or crepitus. The spine is inspected for abnormalities. Gait and ability to perform daily activities are observed.
- Neurological exam: Cranial nerves, motor function, sensory function, and reflexes are tested. Coordination, balance, and fine motor skills are assessed for abnormalities.
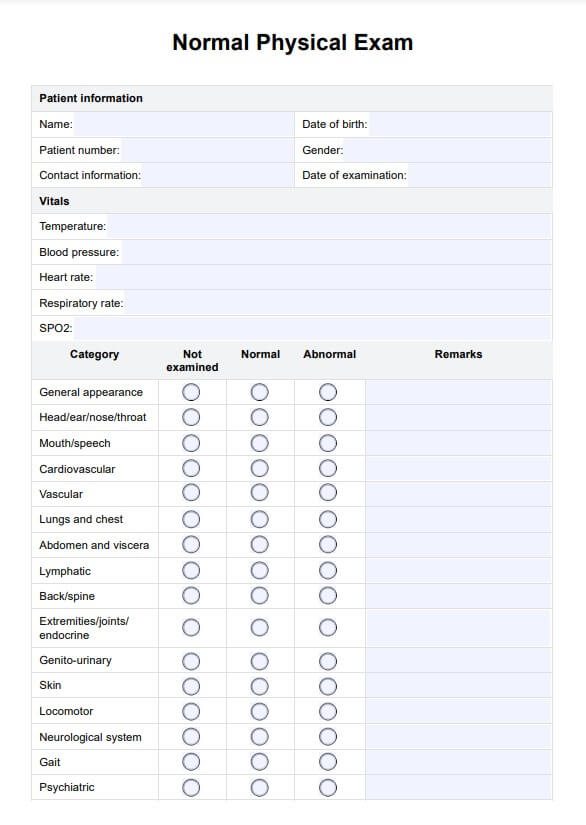
Normal Physical Exam Template
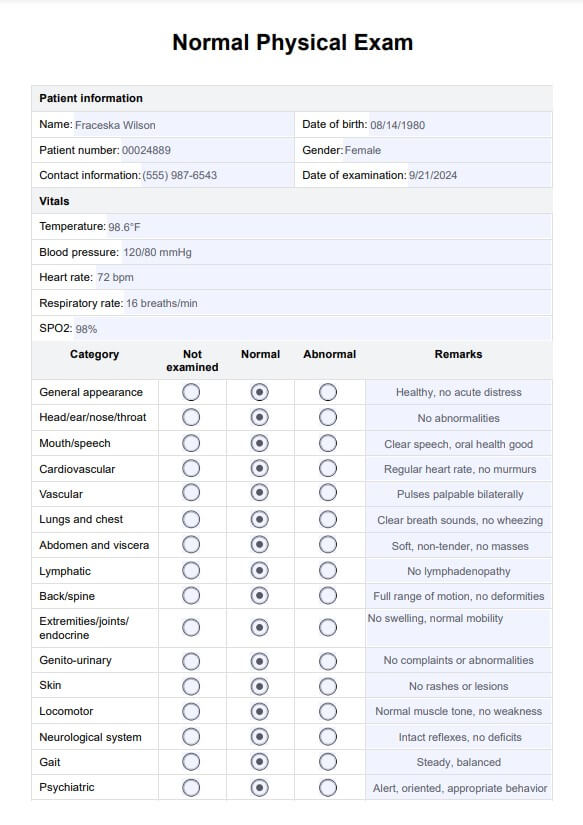
Normal Physical Exam Template Example
How to use this template?
Our Normal Physical Exam Template is functional and intuitive. Follow the steps below to get yourself started with this template:
Step 1: Download the template
You can download the free PDF template onto your devices or access it from the Carepatron template library, allowing more flexibility in the template design and content.
Step 2: Patient information & vitals
Document the necessary patient information for identification purposes. Then, record all the vitals on the template to quickly assess the patient's health status.
Step 3: Review the systems
We have listed many systems for you. This certainly doesn't mean you need to assess every body system, only those relevant to the patient's specific presentation. Select and comment on all the reviewed systems, and mark those not examined as ‘not examined.'
Step 4: Additional notes
You can practically write down anything in this section, from essential documentation of patients' presenting complaints to highly specialized areas of examination that are not included in the worksheet. Essentially, you are adding anything that brings a holistic picture of the patient to anyone who will view this examination result in the future, aiding in creating the patient's treatment plan.
Step 5: Documentation
Once everything is recorded appropriately, you should store this document organized and securely. Due to the confidentiality of the patient and the importance of the information within this document, please treat it with care and professionalism.
When to conduct a physical examination
Performing physical exams is essential for healthcare providers to ensure timely and appropriate patient care. Here are key situations where physical examinations are necessary:
- Annual check-ups or wellness visits: Routine physical exams assess overall health, screen for potential health issues, and promote preventive care for patients of all ages.
- Evaluation of new symptoms or risk factors: When a patient presents with new symptoms, such as chest pain or difficulty breathing, a focused physical exam helps identify underlying causes and guide further diagnostic testing or treatment.
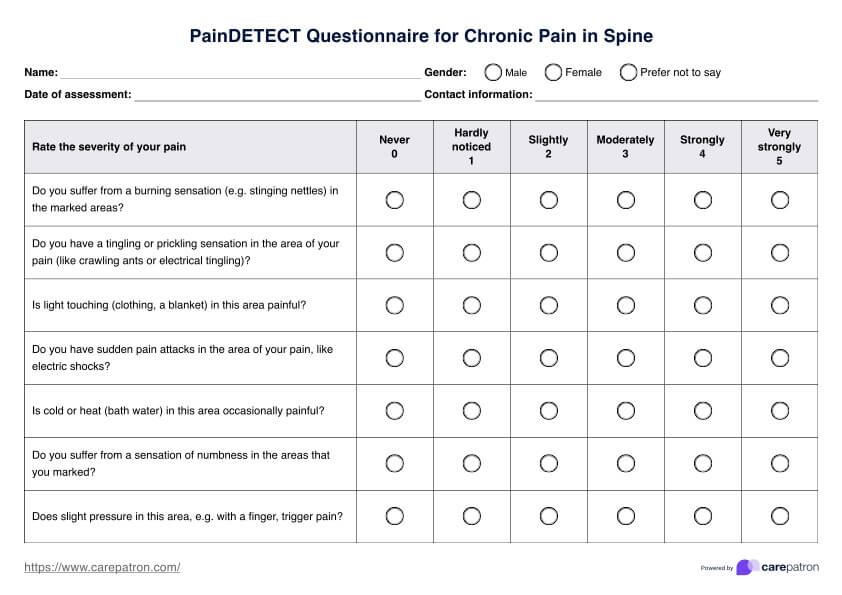
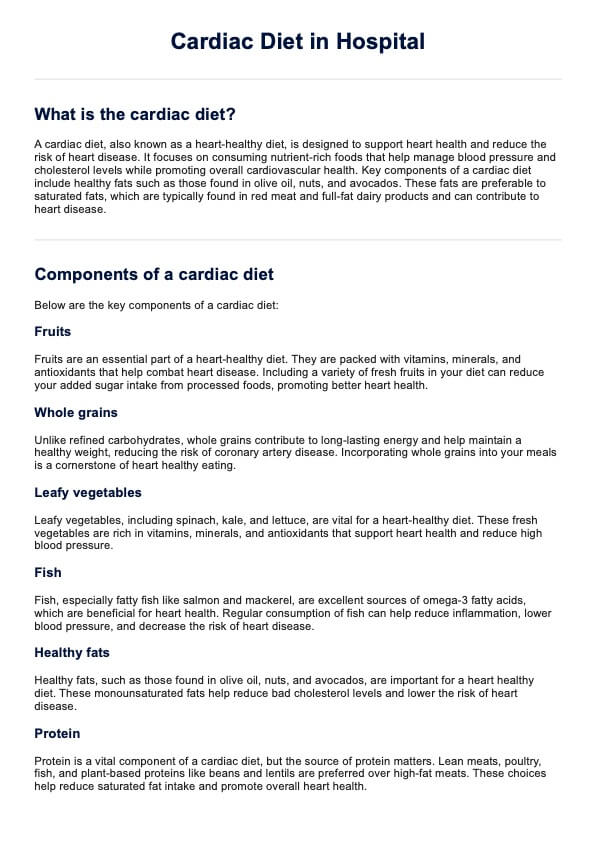
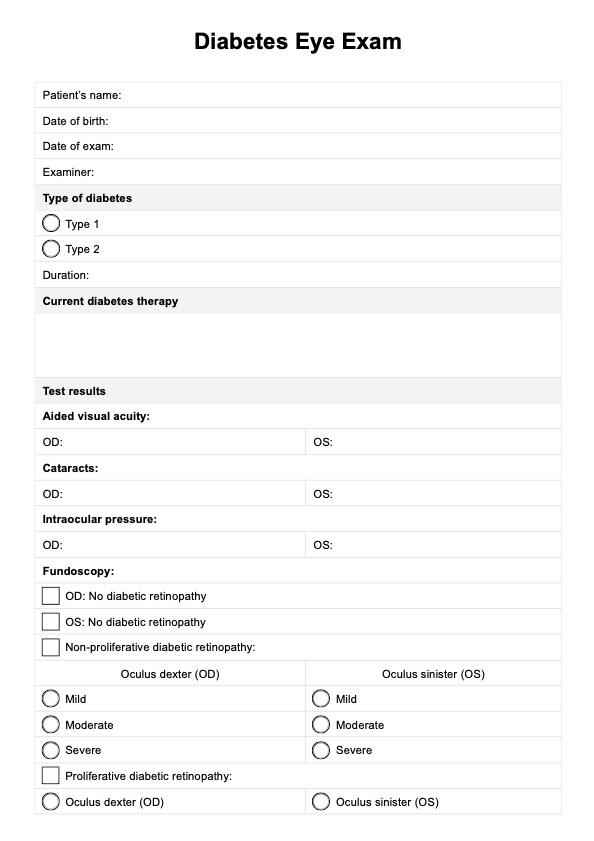
- Monitoring chronic conditions: Regular physical exams for patients with chronic conditions like diabetes or hypertension are crucial for monitoring disease progression, assessing treatment effectiveness, and identifying complications.
- Pre-operative assessment: Before surgery, a physical exam evaluates a patient's fitness for the procedure and identifies potential risks or complications.
- Occupational health assessments: Periodic physical exams in certain occupations ensure employee safety and fitness for duty, especially in jobs involving hazardous materials or physically demanding tasks.
Regular physical exams are fundamental to maintaining health, diagnosing new issues, and managing ongoing conditions. They are a critical component of preventive healthcare and effective medical treatment.
Documenting physical exam results
A systematic approach ensures all relevant information is captured accurately and efficiently during physical exam documentation. Here are key considerations for noting physical exam findings:
Use clear and objective language
Using clear, concise, and objective language is crucial when describing physical exam findings. Avoid ambiguous or subjective terms and use specific, descriptive language to convey the findings accurately. For example, instead of stating, "The patient appears tired," document specific observations like "The patient has dark circles under their eyes and yawns frequently during the exam."
Include both normal and abnormal findings
Comprehensive physical exam documentation should encompass both normal and abnormal findings. Documenting normal findings establishes a baseline for future reference and demonstrates a thorough examination. When describing abnormal findings, provide specific details such as the location, size, shape, color, and texture of any lesions, masses, or abnormalities.
Organize findings by body system
Organizing physical exam findings by body system ensures thorough assessment and documentation of all relevant areas. This systematic approach maintains consistency and completeness in the documentation process. Examples include organizing by HEENT, cardiovascular, respiratory, gastrointestinal, musculoskeletal, and neurological systems.
References
Asif, T., Mohiuddin, A., Hasan, B., & Pauly, R. R. (2017). Importance of thorough physical examination: A lost art. Cureus, 9(5), e1212. https://doi.org/10.7759/cureus.1212
Garibaldi, B. T., & Elder, A. (2021). Seven reasons why the physical examination remains important. Journal of the Royal College of Physicians of Edinburgh, 51(3), 211–214. https://doi.org/10.4997/jrcpe.2021.301
Commonly asked questions
A full physical exam typically includes evaluating the patient's overall health, checking vital signs such as blood pressure, pulse, and temperature, and a head-to-toe examination. This comprehensive exam covers the head, neck, thorax, abdomen, extremities, and musculoskeletal system. A neurological assessment, including an evaluation of cranial nerves, reflexes, and motor and sensory functions, is performed.
To document a normal physical exam, clearly and concisely describe the patient's appearance and note any findings. Include normal results for vital signs, such as heart rate and blood pressure, and document normal physical examination findings for each assessed body system. Ensure all observations are specific and objective to maintain accuracy.
In a musculoskeletal assessment, you can describe the patient's posture, gait, and movement abnormalities or limitations. Note muscle strength, tone, signs of atrophy, joint range of motion, tenderness, or swelling. Document any abnormal reflexes, muscle tone, and signs of weakness or paralysis.