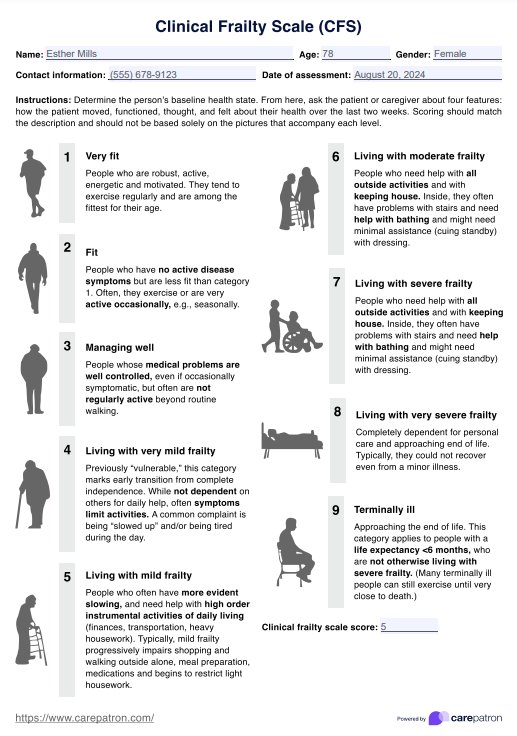
Clinical Frailty Scale (CFS)
Use the Clinical Frailty Scale as a tool to assess frailty in elderly people.


What does it mean for elderly people to be frail?
Frailty in elderly people is a complex health state characterized by increased vulnerability to stressors and decreased physiological reserves. It's not simply a matter of aging but rather a distinct clinical syndrome that can significantly impact an individual's health outcomes and quality of life.
It's important to note that frailty is not inevitable in aging. Many older adults remain robust and active well into their later years. However, when severe frailty does occur, it's associated with an increased risk of adverse health outcomes. These can include falls, hospitalization, disability, and even mortality.
Complications frailty may lead to
When we talk about frailty in older adults, we're referring to a state where multiple body systems have declined, reducing the ability to maintain homeostasis in the face of everyday or acute stressors. This can manifest in various ways, including:
- Unintentional weight loss
- Muscle weakness (sarcopenia)
- Decreased walking speed
- Low physical activity levels
- Self-reported exhaustion
Frail elderly individuals often experience a cycle of declining function. Reduced muscle strength can lead to decreased physical activity, further weakening muscles and creating a downward spiral or a potential frailty syndrome.
Clinical Frailty Scale (CFS) Template
Clinical Frailty Scale (CFS) Example
What is the Clinical Frailty Scale (CFS)?
The Clinical Frailty Scale (CFS) is a widely used comprehensive geriatric assessment tool designed to evaluate the level of frailty in older adults. It provides a standardized method for healthcare professionals to assess and communicate about a patient's overall health status and vulnerability to adverse outcomes.
This global clinical measure is based on clinical judgment and considers factors such as comorbidity, function, and cognition. It categorizes individuals on a 9-point scale, ranging from 1 (very fit) to 9 (terminally ill).
How do healthcare professionals use this scale?
Healthcare professionals use this frailty assessment tool in various ways to enhance patient care and clinical practice:
- Risk assessment: The CFS helps identify patients at higher risk of adverse outcomes, allowing for more targeted interventions and care planning.
- Treatment decision-making: In clinical settings, the CFS can guide decisions about treatment intensity. For instance, in critically ill patients, CFS scores can inform discussions about the appropriateness of intensive care interventions.
- Resource allocation: In settings where resources are limited, the CFS can help prioritize care for those most likely to benefit, such as geriatric patients with very severe frailty and critical illness.
- Communication: The CFS provides a common language for healthcare professionals to discuss a patient's health status, facilitating clearer communication within and between healthcare teams.
- Prognostication: CFS scores can help estimate life expectancy and inform end-of-life care discussions.
How is it scored, and how are the results interpreted?
The CFS is scored on a 9-point scale, with each point representing a different level of fitness or frailty. Higher scores are interpreted as indicators of a greater risk of frailty. Considerations are also given when assessing frailty among patients with dementia.
It is also important to note that while the CFS is a valuable tool, it should be used with other clinical assessments or frailty measures and not as a sole determinant of care decisions. The context of the individual patient, including their preferences and goals of care, should always be considered alongside the CFS score.
How to use our CFS template
Using the Clinical Frailty Scale effectively in frailty screening involves a systematic approach. Our template is based on the updated version of the CFS introduced by Rockwood and Theou (2020), which is the CFS 2.0. Here's a concise step-by-step guide for practitioners:
Step 1: Gather information
Begin by collecting relevant information about the patient. This includes their medical history, health status, functional abilities, and cognitive function. Conduct a brief interview with the patient and/or their caregiver to understand their daily activities, exercise habits, and any difficulties they face. Review available medical records and recent test results.
Step 2: Assess functional status
Evaluate the patient's ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Consider their mobility, energy levels, and any symptoms that limit their activities. Pay attention to signs of slowing, fatigue, or need for assistance in various tasks.
Step 3: Apply the CFS criteria
Using the gathered information, match the patient's overall status to the most appropriate CFS level. Remember that the CFS is a judgment-based tool, so consider all aspects of the patient's health and function. Refer to the detailed descriptions for each level (1-9) and select the one that best fits the patient's current state, whether it's very mild frailty or moderate frailty.
Step 4: Document and communicate
Record the CFS score in the patient's medical record and a brief justification for the chosen level. Communicate this score to other healthcare team members. Use the CFS score to inform discussions about treatment options, care goals, and resource allocation.
Interventions that account for an elderly person's frailty
When caring for elderly individuals with frailty, tailored interventions can significantly improve their quality of life and aging health.
Exercise interventions
A structured exercise program that includes resistance training, balance exercises, and aerobic activities can help maintain and improve physical function. These programs should be tailored to the individual's capabilities and gradually increased in intensity as tolerated.
Nutritional support
Malnutrition and weight loss are common in frailty and can exacerbate the condition. Implementing nutritional strategies, such as protein supplementation and ensuring adequate caloric intake, can help maintain muscle mass and improve overall health.
Medication management
As frailty often coexists with multiple chronic conditions, polypharmacy is common. Regular medication reviews can help identify potentially inappropriate medications, reduce adverse drug events, and optimize pharmacotherapy.
Cognitive stimulation and social engagement
Activities challenging the mind, such as puzzles, reading, or learning new skills, can help maintain cognitive function. Encouraging social interactions through group activities or community programs can combat social isolation and improve mental well-being.
Reference
Rockwood, K., & Theou, O. (2020). Using the Clinical Frailty Scale in allocating scarce health care resources. Canadian Geriatrics Journal, 23(3), 254–259. https://doi.org/10.5770/cgj.23.463
Commonly asked questions
Early identification of frailty allows for interventions that may prevent, delay, or reverse frailty, such as exercise, nutritional optimization, and treatment of underlying conditions.
No, frailty exists on a spectrum. Not all frail individuals develop a disability, and some may revert to a less frail state with appropriate interventions.
Healthcare providers should routinely screen for frailty, provide targeted interventions, and coordinate care across settings to optimize outcomes for frail older adults.