Septic Arthritis Diagnosis Criteria
Learn about the diagnosis criteria for septic arthritis in children. Download Carepatron's free PDF for comprehensive information.


What is septic arthritis?
Septic arthritis affects individuals with joint inflammation, leading to joint pain, swelling, and potential joint damage. Such viral infections can be caused by bacteria, viruses, or fungi that invade the joint, often resulting in a rapid onset of symptoms and risk factors.
Children and the elderly are at a higher risk of developing septic arthritis, as well as individuals with weakened immune systems or underlying health conditions such as diabetes or rheumatoid arthritis (Mayo Clinic, 2018; Momodu & Savaliya, 2023).
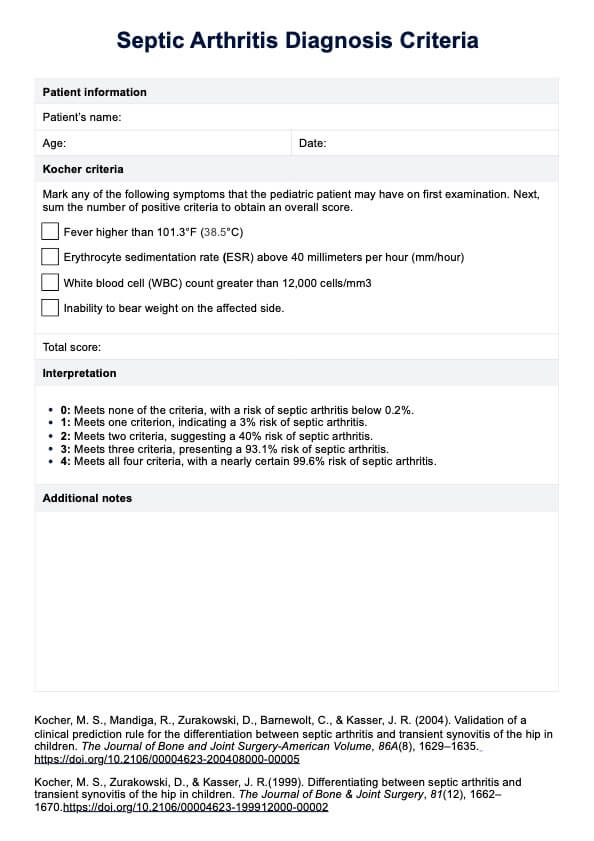
Septic Arthritis Diagnosis Criteria Template
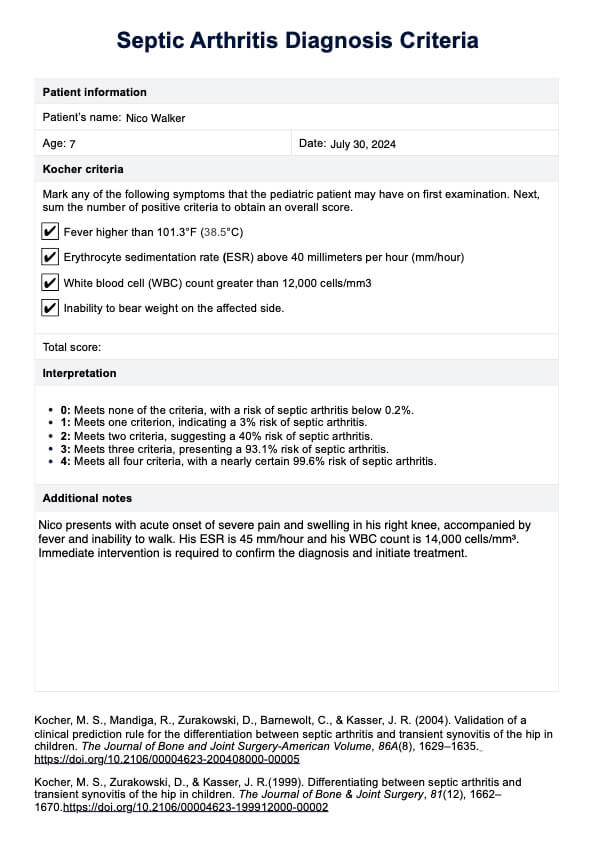
Septic Arthritis Diagnosis Criteria Example
Symptoms of septic arthritis
The symptoms of septic arthritis can vary depending on the severity of the infection and which joint is affected. However, common symptoms include:
- Joint pain
- Swelling
- Redness
- Warmth around the joint
- Limited range of motion in the affected joint
In children, septic arthritis may also cause a high fever and irritability. If left untreated, the infection can spread to other parts of the body and lead to serious complications such as joint damage, bone death, or even sepsis (a life-threatening condition caused by an overwhelming immune response to infection).
How is this different from arthritis?
Septic arthritis differs from other forms of arthritis, such as rheumatoid arthritis, in that it is caused by an infection rather than an autoimmune response. While rheumatoid arthritis involves chronic inflammation due to the immune system attacking the joints, septic arthritis results from bacteria, viruses, or fungi invading the joint spaces. This distinction is crucial for diagnosing septic arthritis, as treatment involves antibiotics or antifungal medications, rather than anti-inflammatory drugs used for arthritis.
Reactive arthritis vs septic arthritis
Reactive arthritis and septic arthritis are distinct conditions with different causes. Reactive arthritis is an autoimmune response triggered by an infection elsewhere in the body, leading to joint inflammation and pain. In contrast, septic arthritis directly involves the infection of the joint itself, resulting in more acute symptoms such as severe joint pain, swelling, and fever. Reactive arthritis is typically diagnosed after ruling out septic arthritis, often through physical examination and joint fluid analysis. Early diagnosis and prompt treatment are essential in managing septic arthritis to avoid joint damage.
How do healthcare professionals diagnose septic arthritis?
The first step in diagnosing septic arthritis is taking a thorough medical history and conducting a physical examination. The doctor will ask about your symptoms, such as pain, stiffness, swelling, and fever. They will also inquire about any recent injuries or surgeries involving the affected joint.
During the physical examination, the doctor will assess the range of motion of the affected joint and look for signs of inflammation, such as redness, warmth, and tenderness.
After the initial assessment, the doctor may order tests to confirm the diagnosis. These tests may include:
- Joint aspiration: This procedure involves taking a sample of fluid from the affected joint with a needle. The fluid is then sent to the laboratory for analysis. In septic arthritis, this fluid will show high levels of white blood cells and bacteria.
- Blood tests: A complete blood count (CBC) can help determine if there is an infection in the body. A high white blood cell count and elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) are suggestive of an infection.
- Imaging tests: X-rays, ultrasound, or MRI of the affected joint may be ordered to rule out other possible causes of joint pain, such as fractures or osteoarthritis. In septic arthritis, these imaging tests may also show signs of inflammation and joint damage.
- Bacterial culture: If fluid is obtained from a joint aspiration, it can be cultured in the laboratory to identify the specific bacteria causing the infection.
In children, septic arthritis may present with different symptoms and require a slightly different approach to diagnosis. Healthcare providers may use additional tests such as blood cultures, bone scans, or joint ultrasounds to confirm the diagnosis for children.
What is the Septic Arthritis Diagnosis Criteria?
Because diagnosing septic arthitis in children can be challenging, doctors often a Septic Artritis Diagnosis Criteria called the Kocher criteria to help identify the condition. The criteria are based on four clinical features: temperature, white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), and the percentage of polymorphonuclear leukocytes (%PMN).
Pediatric patients who present with symptoms can be assessed for the risk of septic arthritis based on specific criteria. Those meeting none of the criteria have a risk below 0.2%. If one criterion is met, the risk increases to 3%. Meeting two criteria suggests a 40% risk, while three criteria present a 93.1% risk. Patients meeting all four criteria have a nearly certain 99.6% risk of septic arthritis (Kocher et, al., 2004).
Please note that these diagnostic criteria are specifically designed for children and have limited applicability to adults. They are less effective for diagnosing septic arthritis in adults, (Borzio et al., 2016).
Septic arthritis affects individuals with joint inflammation, leading to joint pain, swelling, and potential joint damage. Such viral infections can be caused by bacteria, viruses, or fungi that invade the joint, often resulting in a rapid onset of symptoms and risk factors.
Children and the elderly are at a higher risk of developing septic arthritis, as well as individuals with weakened immune systems or underlying health conditions such as diabetes or rheumatoid arthritis (Mayo Clinic, 2018; Momodu & Savaliya, 2023).
How to use our Septic Arthritis Diagnosis Criteria template
Our Septic Arthritis Diagnosis Criteria template includes the Kocher criteria, used to diagnose septic arthritis in children. Follow these steps to get started:
Step 1: Download the template
Access the template using the link on this page. You can also get it from the Carepatron app or our resources library.
Step 2: Print or use the digital format
You can print the template and fill it out manually, or use the digital format on your computer or tablet. Make sure to save a copy of your completed criteria for future reference.
Step 3: Gather patient information
Collect relevant patient information such as age, medical history, and current symptoms. This will help you accurately complete the diagnosis criteria.
Step 4: Complete the Kocher criteria
Follow the instructions on the template to assess each criterion and check off if it is present or absent in the patient. The number of positive criteria will determine the likelihood of septic arthritis.
Step 5: Add any notes
Use the alloted section in the template to add any additional notes or observations about the patient's condition.
Step 6: Review and consult
After completing the criteria, review your findings and assess the likelihood of septic arthritis in the patient. Consult with other medical professionals if necessary.
Next steps after diagnosis
Once septic arthritis is diagnosed, prompt treatment is crucial to prevent further joint damage and complications. The immediate next step is to initiate appropriate antibiotic or antifungal therapy based on the identified pathogen from the joint fluid analysis. This is often coupled with a regimen of anti-inflammatory medications to manage pain and reduce inflammation.
The infected joint may require drainage to remove purulent material and relieve pressure. Regular monitoring through follow-up appointments is essential to assess the effectiveness of the treatment and to make adjustments as needed. Rehabilitation, including physical therapy, should be considered to restore joint function and strength.
Additionally, addressing any underlying conditions, such as diabetes or immune disorders, is vital for comprehensive care. Collaboration with an orthopedic surgeon may be necessary for severe cases or complications. Early and aggressive management improves outcomes and helps prevent long-term joint damage.
References
Borzio, R., Mulchandani, N., Pivec, R., Kapadia, B. H., Leven, D., Harwin, S. F., & Urban, W. P. (2016). Predictors of septic arthritis in the adult population. Orthopedics, 39(4), e657–e663. https://doi.org/10.3928/01477447-20160606-05
Kocher, M. S., Mandiga, R., Zurakowski, D., Barnewolt, C., & Kasser, J. R. (2004). Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. The Journal of Bone and Joint Surgery-American Volume, 86A(8), 1629–1635. https://doi.org/10.2106/00004623-200408000-00005
Mayo Clinic. (2018). Septic arthritis - symptoms and causes. https://www.mayoclinic.org/diseases-conditions/bone-and-joint-infections/symptoms-causes/syc-20350755
Momodu, I. I., & Savaliya, V. (2023, July 3). Septic arthritis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538176/
Commonly asked questions
Septic arthritis is diagnosed through a combination of clinical evaluation and diagnostic tests. Key procedures include arthrocentesis to analyze joint fluid, blood tests to check for infection, and physical examination to assess joint swelling and pain.
According to the Kocher criteria, a fever higher than 101.3°F (38.5°C), an erythrocyte sedimentation rate (ESR) above 40 millimeters per hour (mm/hour), a white blood cell (WBC) counts greater than 12,000 cells/mm3, and an inability to bear weight on the affected side are key indicators.
The gold standard for diagnosing septic arthritis is the analysis of synovial fluid obtained through arthrocentesis. This procedure allows for the identification of pathogens and the assessment of joint inflammation and infection.