Pelvic Organ Prolapse Quantification System
Discover the benefits of using the Pelvic Organ Prolapse Quantification (POP-Q) system for accurate diagnosis and treatment. Download a free template!


What is pelvic organ prolapse?
Pelvic organ prolapse (POP) occurs when one or more of the pelvic organs (such as the bladder, uterus, or rectum) descend into or outside the vaginal canal due to the weakening of the pelvic floor muscles and tissues. This condition can result in a variety of symptoms, including a feeling of heaviness or bulging in the vagina, urinary incontinence, and difficulties with bowel movements.
There are several types of POP, classified based on the organ involved:
- Cystocele: Prolapse of the bladder into the front wall of the vagina. The anterior vaginal wall plays a significant role in anterior vaginal wall prolapse.
- Rectocele: Prolapse of the rectum into the back wall of the vagina. The posterior vaginal wall is crucial in posterior vaginal wall prolapse.
- Uterine prolapse: Descent of the uterus into the vaginal canal.
- Enterocele: Prolapse of the small intestine into the vaginal canal.
Causes of POP include childbirth, aging, menopause, hysterectomy, and activities that increase abdominal pressure, such as heavy lifting, chronic coughing, or constipation. Women with POP may also experience sexual dysfunction, urge incontinence, and a visible or palpable bulge in the vaginal area.
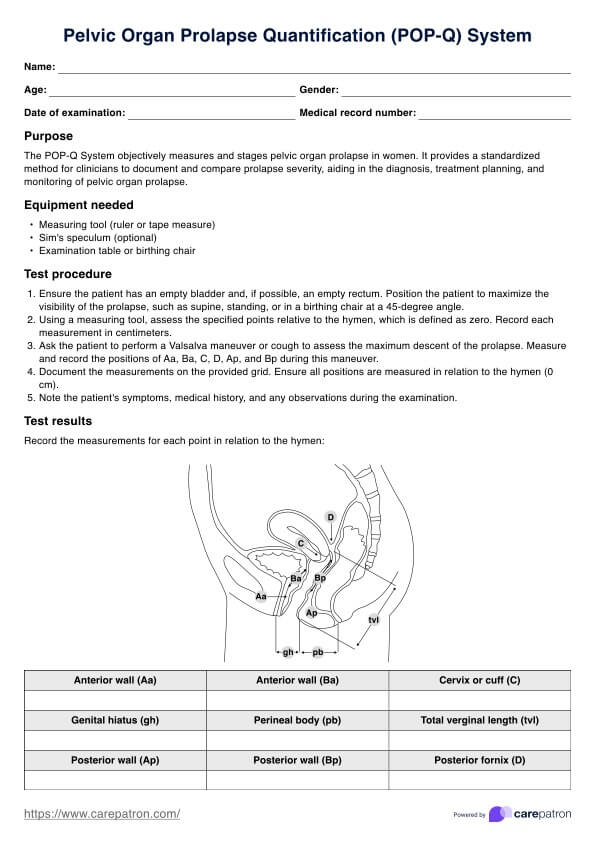
Printable Pelvic Organ Prolapse Quantification System Template
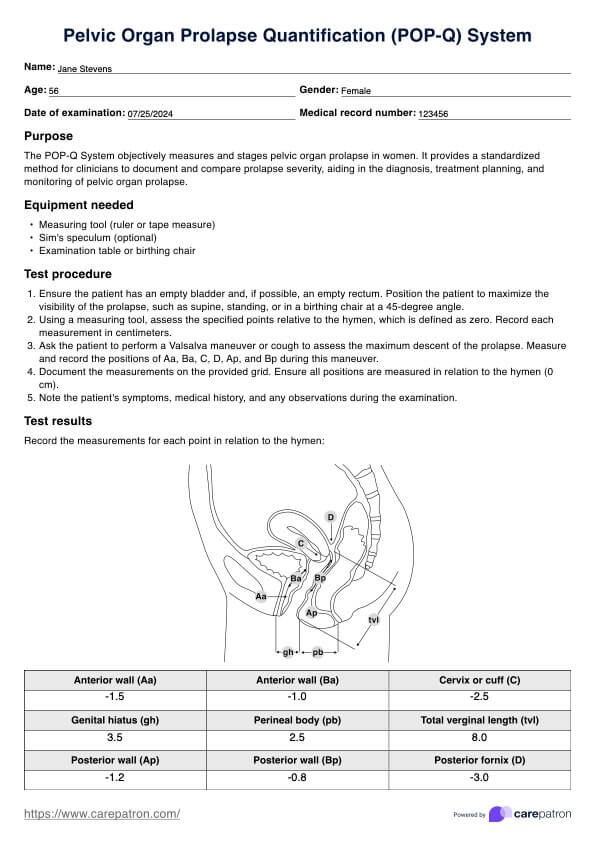
Printable Pelvic Organ Prolapse Quantification System Example
What is the Pelvic Organ Prolapse Quantification System?
The Pelvic Organ Prolapse Quantification (POP-Q) System is an objective, standardized method for assessing and describing the extent of pelvic organ prolapse in women. Developed by the International Continence Society (ICS) and the American Urogynecologic Society (AUS), it uses specific anatomical landmarks and measurements to quantify the severity of the prolapse. By providing a uniform recording method, the POP-Q system allows for consistent documentation and comparison of prolapse across different clinical settings and studies.
The importance of the POP-Q system in pelvic prolapse staging cannot be overstated. It is crucial to provide a standardized tool for describing and staging female pelvic organ prolapse. Additionally, it provides a comprehensive and reliable method for defining the features of a prolapse, making it the most commonly used system in clinical practice and research.
The ICS, the AUS, and the Society of Gynecologic Surgeons (SGS) approve and recommend the system, highlighting its acceptance and use by gynecologic surgeons.
How to use the Pelvic Organ Prolapse Quantification System?
The POP-Q system is a structured approach to accurately measuring and documenting pelvic organ prolapse. Follow these steps to use the system effectively:
Step 1: Download the template
First, download the Pelvic Organ Prolapse Quantification (POP-Q) system template to ensure accurate and consistent documentation. This template includes grids and diagrams for recording measurements.
Step 2: Prepare for the examination
Ensure the patient has an empty bladder and, if possible, an empty rectum to avoid underestimating the prolapse. Position the patient in a way that maximizes the visibility of the prolapse, such as supine, standing, or in a birthing chair at a 45-degree angle.
Step 3: Measure specific points
Using a measuring tool, assess the specified points relative to the hymen (defined as zero). Measure and record points Aa, Ba, C, D, Ap, and Bp during a maximum Valsalva maneuver or cough. Additionally, measure the distance of the upper posterior vaginal wall, which is a critical point in assessing a predominantly posterior support defect within the POP-Q system framework.
Step 4: Record measurements
Document the measurements on the provided grid. During the examination, ensure to retract and assess the posterior vaginal walls for prolapse, documenting and measuring them as part of the comprehensive POP-Q assessment. Note each point's distance in centimeters relative to the hymen. Positive values indicate positions below the hymen, while negative values indicate positions above.
Step 5: Analyze and interpret results
Use the recorded measurements to stage the prolapse, ranging from Stage 0 (no prolapse) to Stage 4 (complete vaginal eversion). This helps determine the severity of the condition and plan appropriate treatment.
Recording and staging
Accurately recording and staging pelvic organ prolapse (POP) is crucial for diagnosis and treatment planning. The POP-Q system provides a structured approach, using specific anatomical points and measurements relative to the hymen. During the examination, measure six distinct points: Aa, Ba, C, D, Ap, and Bp. Record these measurements in centimeters, noting whether they are above (negative values) or below (positive values) the hymen.
The measurement of the genital hiatus (GH) is also important as it is correlated with and predictive of apical vaginal support loss, which may necessitate further assessment before planning treatments such as hysterectomy or POP repair surgery. Once all measurements are documented, classify the prolapse into stages:
- Stage 0: No prolapse observed.
- Stage 1: The most distal portion is >1 cm above the hymen.
- Stage 2: The most distal portion is between 1 cm above and 1 cm below the hymen.
- Stage 3: The most distal portion is >1 cm below the hymen but not beyond 2 cm less than the total vaginal length.
- Stage 4: Complete vaginal eversion or within 2 cm of the total vaginal length.
The POP-Q system is also reliable for evaluating and staging pelvic floor dysfunction, providing reproducible results in clinical research and practice. Accurate staging helps determine the severity of the prolapse and guides the treatment approach.
Next steps
After recording and staging the prolapse using the POP-Q system, the next steps involve discussing treatment options with the patient. Treatment choices depend on the severity of the prolapse and the patient's symptoms and preferences. For mild cases, conservative management such as pelvic floor exercises, lifestyle modifications, and pessary use might be recommended.
In more severe cases (Stage 3 or 4), surgical intervention may be necessary. Options include vaginal or abdominal approaches, depending on the patient's condition and the surgeon's expertise. Post-treatment follow-up is essential to monitor the patient's recovery and ensure the effectiveness of the intervention.
Additionally, educating the patient about maintaining pelvic floor health is crucial to prevent recurrence. This includes discussing exercises, diet, and habits that support pelvic floor strength. Using the POP-Q system template helps ensure a comprehensive and standardized approach to managing pelvic organ prolapse.
Benefits of using our template
Using our Pelvic Organ Prolapse Quantification (POP-Q) system template offers several advantages for healthcare providers:
Enhanced accuracy and consistency
Our template ensures that all measurements are recorded precisely and consistently, which is essential for accurate diagnosis and treatment planning. This consistency helps compare results over time and across different clinicians.
Improved patient communication
Our template's standardized format makes it easier to explain the condition and treatment options to patients. Clear visual aids and consistent measurements enhance patient understanding and engagement in their care.
Streamlined workflow
Using a structured template saves healthcare providers time and reduces errors in documenting pelvic organ prolapse. This streamlined process improves efficiency and allows more focus on patient care.
Commonly asked questions
The POP-Q system quantifies and stages pelvic organ prolapse, providing a standardized method for diagnosis and treatment planning.
The POP-Q system uses specific anatomical landmarks and measurements, offering a more objective and reproducible assessment than subjective grading systems.
Yes, the POP-Q system can assess various types of pelvic organ prolapse, including cystocele, rectocele, and uterine prolapse.