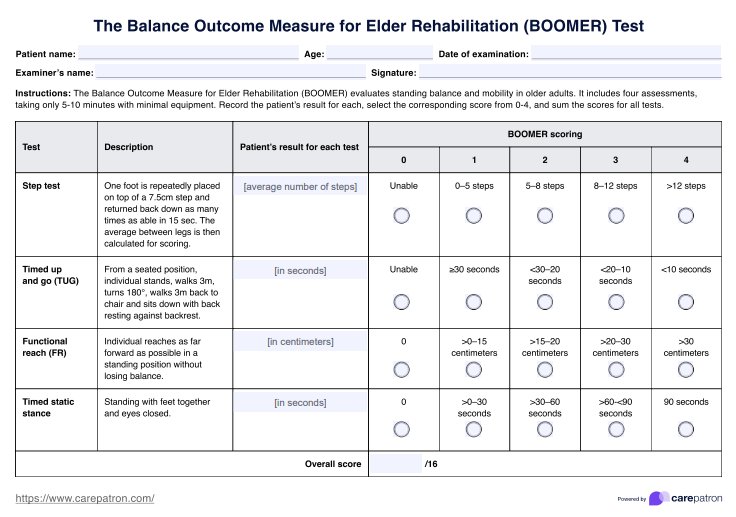
BOOMER Test
Use this BOOMER Test to evaluate standing balance and functional mobility in geriatric patients. Get it for free.


What factors affect an older adult's mobility and balance?
Mobility and balance are two important aspects of an individual's life, most especially for the elderly population. Common conditions that affect these aspects include muscle weakness, joint problems, pain, disease, and neurological difficulties. When these occur together, they can significantly impact mobility (Health in Aging Foundation, n.d.). These conditions can affect factors such as the gait speed displayed by a person, which is a key indicator of mobility. As a healthcare professional, you know better than anyone that addressing these factors can improve a person's life.
BOOMER Test Template
BOOMER Test Example
What risks arise from impaired mobility and balance?
Impaired mobility and balance can lead to several risk factors, including an increased likelihood of the following:
Falls
Annually, millions of people 65 years and older experience falls. Statistics reveal that one in ten falls results in an older adult needing to limit activities or seek medical attention (Centers for Disease Control and Prevention, 2024). Impaired mobility and balance definitely increase the risk of falls, a common issue for older adults.
Higher rates of disease
If older adults have mobility and balance problems, this may mean less physical activity. When an individual is active, they may be less prone to certain diseases like hypertension, stroke, diabetes, etc. (World Health Organization, 2020). A simple walk daily is vital for an older adult's health, which will be impossible if they cannot move well.
Disability
Disability can hinder geriatric patients' ability to do things independently. Most of the time, they will need help or assistance from other people and may require caregivers.
Poor quality of life
Another problem that older adults may face when they cannot move or steady themselves is poor quality of life. This is because they will be primarily sedentary, just staying in their homes, which can bring them feelings of isolation or depression, significantly impacting their well-being.
Increased mortality
Combining the risks above from impaired mobility and balance can contribute to increased mortality risk. Mobility impairments predict higher mortality and dependence, yet physical activity can lower these risks for those affected. Despite their overall greater risk, mobility-impaired individuals may prevent further disability and mortality through regular exercise (Hirvensalo et al., 2000).
What is the BOOMER Test?
The Balance Outcome Measure for Elder Rehabilitation (BOOMER) Test evaluates standing balance and functional mobility in older adults. This functional balance measure combines multiple simple tests into one efficient assessment, taking only 5-10 minutes with minimal equipment. BOOMER consists of four assessments. Here's how each test is conducted:
1. Step test
The individual repeatedly steps up onto a 7.5 cm high step and then back down as many times as possible within 15 seconds. This is done with each foot, and the average number of steps from both legs determines the score.
2. Timed up and go
The individual starts from a seated position, stands up, walks 3 meters, turns 180 degrees, and walks back 3 meters to the chair. The client then sits down again with their back resting against the backrest.
3. Functional reach
The individual stands upright and reaches as far forward as possible without losing balance.
4. Time static stance
The individual is standing with feet together and eyes closed. The time they can maintain this position without moving is recorded to evaluate their balance and stability.
Test validity
The BOOMER Test demonstrated high internal consistency and strong correlation with the modified elderly mobility scale (MEMS) and the functional independence measure (FIM) motor score, with a minimum clinically significant change of 3 points on a 17-point scale (Haines et al., 2007).
A further validation study compared BOOMER's concurrent validity with the Berg Balance Scale (BBS) and gait speed in older adults. BOOMER showed a high correlation with the BBS and a moderate to fair correlation with gait speed. While the BOOMER and BBS displayed moderate correlation in change scores, the gait speed revealed only fair correlation (Kuys et al., 2011).
Based on this, the BOOMER Test is a reliable and valid tool for assessing balance and mobility in elderly adults. However, it may be more closely aligned with balance measures rather than gait speed.
How is it scored and how are the results interpreted?
Results for each test are considered to score the BOOMER Test. The average number of steps from both legs is used to determine the score for the step test. Meanwhile, you record the duration in seconds for both timed up and go and static standing with eyes closed test. The functional reach test measures the distance reached (in meters) to assess their stability and balance.
In our template, we've created a column where you can indicate the patient's results for each test. In the next column, you indicate the corresponding patient score based on their test results. The scale ranges from 0 (unable to perform the test) to 4 (excellent). To get the total score, add up all scores
How to use our BOOMER Test template?
Because we know the importance of ready-made tools when conducting a BOOMER Test, here's one for you. Follow the steps to incorporate it during your session with your client:
Step 1: Download the template
You can grab a copy of our PDF template by clicking on the download link on this page. If you are logged in through the Carepatron platform, you may find it in the templates library.
Step 2: Use during assessment
Before the assessment, explain how the test is performed to your patient. It's best to instruct them beforehand that the four tests will be conducted in one session to measure their mobility, balance, and perceived confidence. This way, they can prepare.
Step 3: Store for future uses
Regular monitoring and follow-up are vital for improving a patient's condition. Store the template and use it as a baseline for comparison in future conducts of the BOOMER Test in your clinic or in geriatric rehabilitation units.
How physical therapists rehabilitate elderly mobility and balance
If you are a physical therapist, rehabilitation is essential for older adults to improve their quality of life. As a start, remember that your clients' needs differ, so it's important to provide them with customized programs aligned to their needs. This can include exercises for strengthening muscles, improving flexibility, and enhancing balance.
You can also assess the home environment and suggest modifications to reduce fall risks, like installing grab bars and removing tripping hazards. Additionally, coordinating with a nutritionist for a protein-rich diet can help manage weight and reduce strain on joints.
References
Centers for Disease Control and Prevention. (2024, May 9). Facts about falls. Older Adult Fall Prevention. https://www.cdc.gov/falls/data-research/facts-stats/index.html
Haines, T., Kuys, S. S., Morrison, G., Clarke, J., Bew, P., & McPhail, S. (2007). Development and validation of the balance outcome measure for elder rehabilitation. Archives of Physical Medicine and Rehabilitation, 88(12), 1614–1621. https://doi.org/10.1016/j.apmr.2007.09.012
Health in Aging Foundation. (n.d.). Caregiver guide: Mobility problems. https://www.healthinaging.org/tools-and-tips/caregiver-guide-mobility-problems
Hirvensalo, M., Rantanen, T., & Heikkinen, E. (2000). Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. Journal of the American Geriatrics Society, 48(5), 493–498. https://doi.org/10.1111/j.1532-5415.2000.tb04994.x
Kuys, S. S., Morrison, G., Bew, P. G., Clarke, J., & Haines, T. P. (2011). Further validation of the balance outcome measure for elder rehabilitation. Archives of Physical Medicine and Rehabilitation, 92(1), 101–105. https://doi.org/10.1016/j.apmr.2010.10.001
World Health Organization. (2020). Physical activity. https://www.who.int/health-topics/physical-activity#tab=tab_1
Commonly asked questions
The Balance Outcome Measure for Elder Rehabilitation (BOOMER) Test evaluates standing balance and functional mobility in older adults.
The BOOMER Test requires a stopwatch, a chair with armrests, a ruler or tape measure, duct tape, a cone, a yardstick, and a 7.5 cm high step.
It usually takes only 5-10 minutes, performed in one session.