SLAP Lesion Treatment Guidelines
Learn about SLAP Lesion Treatment Guidelines and get Carepatron's free PDF download of an example treatment plan.


What are SLAP lesions?
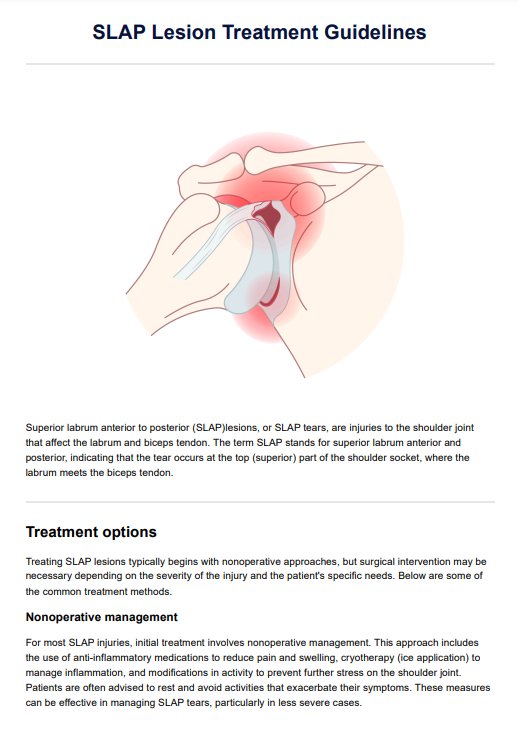
Superior labrum anterior to posterior (SLAP) lesions or SLAP tears, are injuries to the shoulder joint that affect the shoulder labrum and biceps tendon. The term SLAP stands for superior labrum anterior and posterior, indicating that the tear occurs at the top (superior) part of the shoulder socket and shoulder blade, where the shoulder labrum meets the biceps tendon. This area is crucial because it helps stabilize the shoulder joint by ensuring the upper arm bone (or humerus upper arm bone) fits securely into the shoulder socket.
Symptoms of SLAP tears or lesions
Symptoms of SLAP tears or lesions typically manifest as persistent shoulder pain, particularly during overhead activities or when lifting objects. Many individuals experience a deep, aching pain that may extend into the back of the shoulder muscles or down the arm. A common symptom is a feeling of instability in the shoulder joint, often described as a "catching" or "clicking" sensation during movement.
In addition to pain and instability, people with SLAP lesions may notice a decrease in range of motion, making it difficult to perform daily activities that involve reaching or lifting. Weakness in the muscles surrounding, especially when trying to lift objects overhead, is another common complaint. In some cases, there may also be a sensation of the shoulder "locking up," which can be both painful and limiting. These symptoms can worsen over time, particularly without proper treatment and management.
Causes of SLAP lesions
SLAP tears are often caused by repetitive stress or acute trauma, leading to deep pain in the shoulder. Patients may experience a reduced range of motion and a clicking or catching sensation during certain movements. These injuries are common in athletes and individuals who engage in overhead activities that strain the shoulder joint.
SLAP Lesion Treatment Guidelines Template
SLAP Lesion Treatment Guidelines Example
How are SLAP lesions diagnosed?
Diagnosing SLAP lesions involves a systematic approach to ensure accurate identification and to rule out other serious conditions that could cause shoulder pain, such as myocardial infarction or aortic dissection. A combination of clinical evaluation and advanced imaging techniques is used to confirm the presence of SLAP tears.
Clinical evaluation
The first step in diagnosing SLAP lesions is a thorough clinical evaluation by a healthcare professional. During this assessment, the patient's medical history, symptoms, and any recent injuries are reviewed. Physical exam tests, such as the O'Brien test or the Crank test, may be performed to provoke symptoms and help identify the presence of a SLAP tear. These tests focus on reproducing the pain or instability typically associated with SLAP lesions.
Magnetic resonance imaging (MRI)
If a SLAP lesion is suspected, magnetic resonance imaging (MRI) is often recommended to confirm the diagnosis. MRI is a powerful imaging tool that can visualize soft tissues, including the glenoid labrum fibrocartilage. In some cases, an MRI with contrast dye, known as MR arthrography, is used to provide a more detailed view of the labrum and detect any tears or abnormalities. The MRI results, combined with the clinical evaluation, allow for an accurate diagnosis and appropriate treatment planning.
How do healthcare professionals treat SLAP lesions?
Treating SLAP lesions typically begins with nonoperative approaches, but surgical intervention may be necessary depending on the severity of the injury and the patient's specific needs. Below are some of the common treatment methods that are minimally invasive techniques.
Nonoperative management
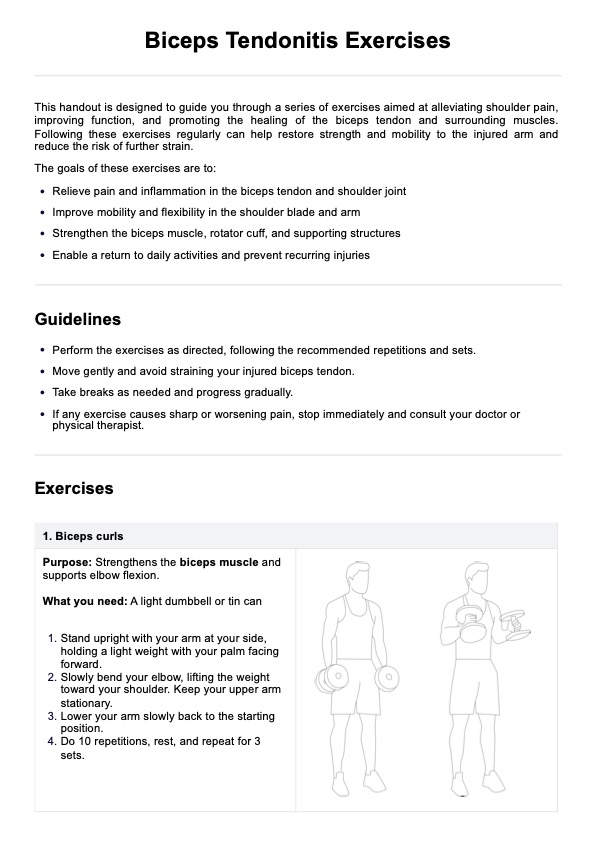
For most SLAP injuries, initial treatment involves nonoperative management. This approach includes the use of anti-inflammatory medications to reduce pain and swelling, cryotherapy (ice application) to manage inflammation, and modifications in activity to prevent further stress on the shoulder joint. Patients are often advised to rest and avoid activities that exacerbate their symptoms. These measures can be effective in managing labrum tears, particularly in less severe cases.
Surgical treatment
When conservative management proves ineffective, surgical intervention becomes necessary. The choice of surgical technique varies based on the type of SLAP lesion:
- Type I lesions: Characterized by fraying of the labrum, these are typically treated through debridement, where damaged tissue is removed to create a stable edge.
- Type II lesions: The most prevalent type, these lesions frequently require arthroscopic repair. This procedure involves reattaching the labrum to the glenoid using sutures or suture anchors to restore stability.
- Type III lesions: These lesions present with a bucket-handle tear of the labrum, which is usually excised, and the remaining labrum is smoothed to ensure stability.
- Type IV lesions: Involving the biceps tendon, treatment may include tenotomy (cutting the tendon) or tenodesis (reattaching the tendon at a different site), in conjunction with labral repair, based on the severity of tendon damage.
Surgical procedures are generally performed arthroscopically, allowing for smaller incisions and a quicker recovery time. The selected technique is influenced by various factors, including the patient's age, activity level, and the presence of other shoulder injuries.
Physical therapy management
Physical therapy management is essential for patients recovering from SLAP lesions. For individuals with Type I SLAP lesions, conservative treatment may be sufficient. This typically begins with a cessation of throwing activities and a short course of anti-inflammatory medication to reduce pain and inflammation. Once pain subsides, physical therapy program focuses on restoring normal shoulder motion and strengthening the shoulder girdle musculature, which is critical for maintaining proper shoulder biomechanics.
Postoperative rehabilitation
For patients undergoing SLAP repair, postoperative rehabilitation varies based on the type of SLAP lesion and the specific surgical procedure performed. Initially, the patient's shoulder is immobilized in internal rotation using a sling. The following is a general guideline for postoperative rehabilitation:
- Week 0 to 3: The shoulder remains immobilized, with external rotation and abduction limited to 60°. Patients can perform pendulum exercises and elbow range-of-motion exercises.
- Week 4 to 8: Sling use is discontinued, and shoulder motion is gradually increased using active-assisted and passive techniques. External rotation is limited to 30° to minimize strain on the labrum, while internal and external rotation activities progress to 90° of shoulder abduction.
- Week 8: Resistance exercises focusing on scapular strengthening can be initiated, provided the patient has achieved approximately 115° to 120° of shoulder external rotation. Resisted biceps tendon activities are prohibited for two months to protect the healing of the biceps tendon anchor.
- Week 16: A sport-directed throwing program can commence for overhead athletes, focusing on exercises such as forward flexion in a side-lying position, prone extension, seated rowing, and serratus punch (protraction with the elbow extended).
- Week 24: Patients can generally return to contact sports, depending on their progress and recovery.
How healthcare professionals will benefit from this handout
The SLAP Lesion Treatment Guidelines handout is a valuable resource for healthcare professionals, offering several key benefits that enhance patient care and streamline the treatment process. Below are three major advantages of using this handout.
Clear and concise treatment guidelines
This handout provides healthcare professionals with clear and concise treatment guidelines for managing SLAP lesions. By outlining both nonoperative and surgical approaches, it helps practitioners quickly identify the most appropriate treatment plan based on the type and severity of the SLAP tear. This structured approach ensures that patients receive consistent and effective care, reducing the risk of mismanagement.
Enhanced patient communication
The handout serves as an excellent tool for improving communication with patients. It simplifies complex medical information, making it easier for healthcare professionals to explain SLAP lesions, the available treatment options, and the expected outcomes. This not only increases patient understanding but also fosters trust and cooperation, leading to better adherence to treatment plans.
Streamlined documentation and care planning
Using the SLAP Lesion Treatment Guidelines handout streamlines the documentation and care planning process. It provides a standardized format that healthcare professionals can use to record patient progress, treatment responses, and follow-up needs. This helps ensure that all aspects of care are thoroughly documented, facilitating more efficient coordination among the healthcare team and improving overall patient outcomes.
Commonly asked questions
A superior labrum anterior to posterior (SLAP) lesion may heal on its own if it's a minor tear, especially with rest, physical therapy, and activity modification. However, more severe labrum tears often require medical intervention for full recovery.
Superior labrum anterior to posterior (SLAP) lesions are typically treated with a combination of nonoperative methods like anti-inflammatory medications, cryotherapy, and physical therapy. In more severe cases, surgical options may be considered to repair the labrum and restore shoulder function.
Type II SLAP lesions, where the labrum is detached, and Type III SLAP lesions, involving a "bucket handle" tear, generally require surgical intervention to reattach or remove the damaged tissue.
The first aid for a superior labrum anterior to posterior (SLAP) tear includes resting the shoulder, applying ice to reduce inflammation, and avoiding activities that cause pain. Over-the-counter anti-inflammatory medications may also help manage pain and swelling in the short term.