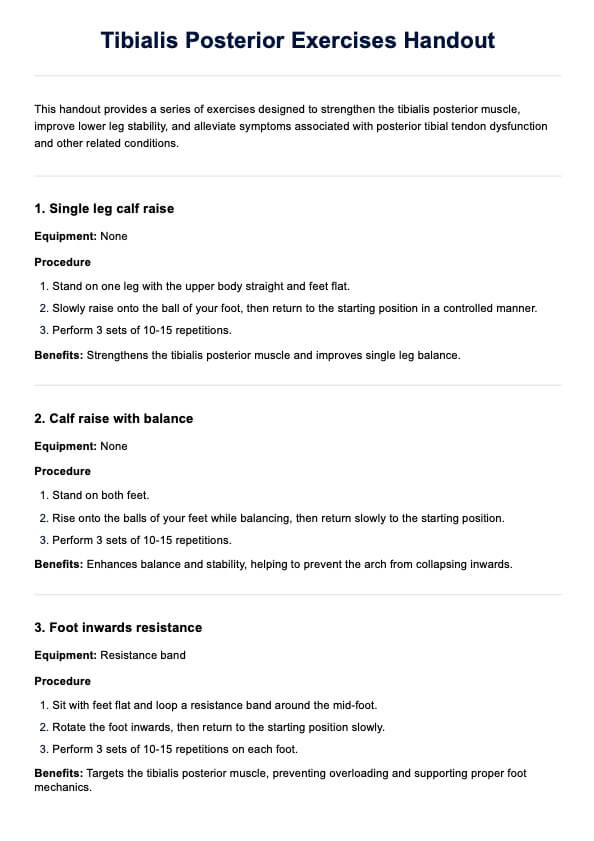
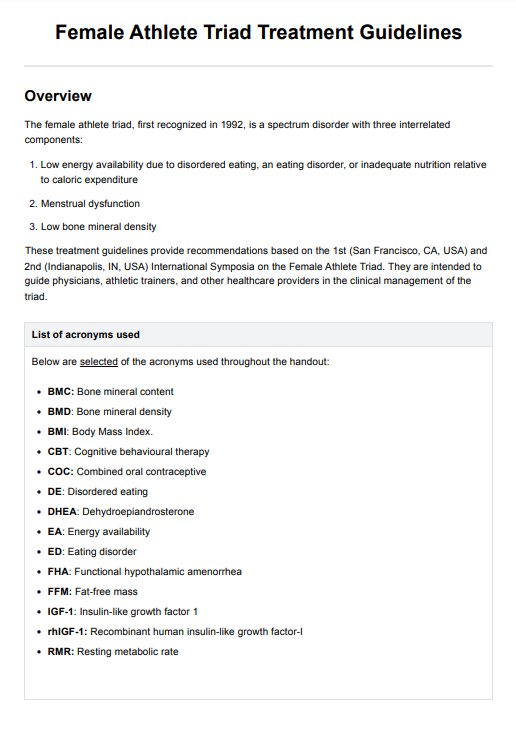
Tibialis Posterior Exercises Handout
Get our handout to help manage posterior tibial tendon dysfunction, strengthen the tibialis posterior, and effectively reduce shin pain.


Importance of tibialis posterior exercises
Tibialis posterior exercises are crucial for maintaining foot health, especially for those dealing with conditions like posterior tibial tendon dysfunction (PTTD) and tibialis posterior tendinopathy. Strengthening this muscle helps stabilize the lower leg and supports the arch, preventing the foot from collapsing inwards.
These exercises can significantly benefit individuals with PTTD, an injured leg, or those experiencing their foot turning inwards. Strengthening the tibialis posterior can prevent further degeneration of the medial malleolus area and improve stability. Incorporating exercises like the single leg calf raise and focusing on keeping the arch from collapsing inwards are effective strategies.
For those recovering from tibial tendon dysfunction PTTD or managing tibialis posterior tendinopathy, consistent practice of these exercises can lead to notable improvements. Remember to keep your foot halfway up during each raise to maximize the benefits.
Tibialis Posterior Exercises Handout Template
Tibialis Posterior Exercises Handout Example
10 exercises for tibialis posterior tendon
Physical therapists can teach these exercises to patients to strengthen the tibialis posterior tendon, improve foot stability, and manage conditions like PTTD. These exercises help physical therapists guide patients in strengthening the tibialis posterior muscle, preventing pain, and improving lower leg stability.
Here are some exercises you can demonstrate for your patients:
1. Single-leg calf raise
Equipment: None
Stand on one leg with the upper body straight. Slowly raise the ball of your foot and return to the starting position. Perform this exercise slowly and control to strengthen the tibialis posterior.
2. Calf raise with balance
Equipment: None
Stand on both feet, rise onto the balls of your feet while balancing, and slowly return to the starting position. This exercise helps with single-leg balance and reduces the risk of the arch collapsing inward.
3. Foot inwards resistance
Equipment: Resistance band
Sit with feet lying flat, loop a band around the mid-foot, and rotate the foot inwards. Slowly return to the starting position. This exercise targets the tibialis posterior muscle and prevents overloading.
4. Standing posterior tibialis stretch
Equipment: None
Stand facing a wall with one leg behind and the knee straight. Lean forward to stretch the leg and maintain a good arch throughout this exercise. This helps reduce the gradual degeneration and weakening of the tendon.
5. Arch support exercise
Equipment: None
Stand on one leg, balance the other leg and focus on maintaining a good arch. Hold for 30 seconds, then switch legs. This prevents overloading the tibialis posterior and reduces pain or shin splints.
6. Seated foot flexion
Equipment: None
Sit with legs extended, and feet should be flat on the floor. Flex your foot toward the shin and then return slowly to the starting position. This motion exercise helps strengthen the tibialis posterior and maintains a neutral position.
7. Single leg balance with heel raise
Equipment: None
Stand on one leg with the upper body slightly backward. Slowly raise the heel of the standing leg and then return to the ground. This improves leg balance and strengthens the tibialis posterior.
8. Resistance band foot eversion
Equipment: Resistance band
Sit with feet flat and loop a band around the mid-foot. Evert the foot outward and return to the starting position. This exercise targets the tibialis posterior and helps with types of shin pain.
9. Standing toe touches
Equipment: None
Stand with the feet on the floor and bend forward to touch your toes, keeping the knee straight. This stretch helps reduce the causes of shin pain and supports the posterior tibialis.
10. Wall press arch exercise
Equipment: None
Stand facing a wall and press the ball of your foot against it. Maintain the arch and slowly return to the starting position. This exercise strengthens the posterior tibialis and prevents gradual degeneration of the tendon.
By incorporating these exercises into a patient's routine, physical therapists can effectively address tibialis posterior tendinopathy, strengthen the tibialis posterior muscle, and improve overall lower leg stability.
How to use our Tibialis Posterior Exercises Handout
This handout helps healthcare practitioners guide patients through exercises to strengthen the tibialis posterior muscle, improve lower leg stability, and prevent pain.
Step 1: Introduce the handout
Explain to patients that these exercises are designed to strengthen the tibialis posterior muscle, crucial for maintaining foot stability and preventing conditions like PTTD and tibialis posterior tendinopathy.
Step 2: Demonstrate each exercise
Show patients how to perform each exercise correctly. Emphasize the importance of maintaining proper form, such as keeping feet flat at the starting position and avoiding overloading the tibialis posterior. For example, demonstrate the single leg calf raise, ensuring the patient understands the correct motion.
Step 3: Supervise initial practice
Watch patients perform the exercises, providing feedback and corrections as needed. Ensure they move in a slow and controlled manner to maximize the benefits and prevent injuries. Highlight key points, such as maintaining a good arch throughout the exercise and avoiding the arch collapsing inwards.
Step 4: Customize the routine
Adjust the exercise routine based on the patient's specific needs and progress. Some patients might require more focus on leg balance exercises, while others might benefit from additional stretching for the lower leg.
Step 5: Provide follow-up and support
Schedule regular check-ins to monitor progress and make necessary adjustments. Encourage patients to contact you if they are currently experiencing shin pain or shin splints. Offer tips for success, such as gradually increasing the intensity of the exercises.
By following these steps, healthcare practitioners can effectively use this handout to help patients strengthen their tibialis posterior muscle, improve lower leg stability, and prevent or manage conditions like PTTD. Regular supervision and customization of the exercise routine are crucial to achieving the best outcomes for each patient.
How do professionals benefit from using this handout?
Using this handout helps professionals provide targeted care, improving patient outcomes and enhancing their practice. Here are its benefits:
Streamlined patient education
The handout offers a clear, structured approach to educating patients about strengthening the tibialis posterior muscle, preventing conditions like tibial tendon dysfunction, plantar fasciitis, and causes of shin pain.
Improved patient outcomes
By following the exercises, patients can reduce the risk of PTTD and enhance stability during sporting activities, which leads to better overall foot health.
Enhanced professional efficiency
Providing a standardized handout saves time for healthcare professionals. It allows them to focus on personalized care while ensuring patients receive consistent, high-quality information.
Comprehensive care plan
The handout covers various aspects of posterior tibialis health, including exercises to prevent overloading the posterior tendon during running and tips for maintaining the foot with your arch properly supported.
Increased patient compliance
A well-designed, easy-to-follow handout encourages patients to adhere to their exercise regimen. This leads to better management of conditions like tibial tendon dysfunction and plantar fasciitis and reduces the types of shin pain associated with weak posterior tibial muscles.
Commonly asked questions
If the posterior tibialis muscle is weak, it can lead to a condition known as posterior tibial tendon dysfunction (PTTD). This can cause pain and discomfort in the foot and ankle, making it difficult to walk or stand for long periods of time.
Weak posterior tibialis can be caused by various factors such as overuse or strain on the muscle, age-related degeneration, obesity, flat feet or fallen arches, injury or trauma to the foot or ankle, and certain medical conditions such as rheumatoid arthritis.
Exercises that can help strengthen the tibialis posterior include heel raises, toe curls, and resistance band exercises. It is important to gradually increase the difficulty and intensity of these exercises to avoid injury and ensure proper strengthening of the muscle.