Tinea Infection Treatment Guidelines
Learn about the guidelines and treatment options for tinea infections with Carepatron's free PDF download and effectively manage this common skin condition.


Tinea fungal infection types
Tinea fungal infections, commonly known as ringworm, are contagious fungal infections that can affect various parts of the body. These infections are caused by dermatophytes, fungi that thrive in warm, moist environments. Tinea infections are highly contagious and often spread through skin-to-skin contact, sharing personal items, or contact with contaminated surfaces.
Here are the different types of tinea infections:
Tinea pedis
Tinea pedis, or athlete's foot, is a superficial fungal infection affecting the feet, particularly between the toes. It causes itching, redness, and peeling skin, and can spread to other areas of the body if not treated promptly.
Jock itch
Jock itch, also known as tinea cruris, affects the groin area, inner thighs, and buttocks. This condition presents as red, scaly rash that can be uncomfortable and persistent.
Tinea capitis
Tinea capitis, or scalp ringworm, primarily affects children. It leads to scalpy patches on the scalp, which can result in hair loss if not treated. Tinea capitis requires prescription antifungal medications for effective management.
Ringworm
Ringworm, or tinea corporis, affects the body's skin, presenting as circular, red, and itchy patches. It is one of the most common fungal infections and can be treated with antifungal creams.
Tinea manuum
Tinea manuum targets the hands, causing dry, thickened, and peeling skin. It often accompanies other tinea infections, such as athlete's foot.
Tinea corporis
Tinea corporis resemble ringworm that affects the body. It creates ring-shaped, itchy patches on the affected skin and is commonly spread through skin-to-skin contact.
Tinea unguium
Tinea unguium, or nail fungus, affects the nails, causing them to become thick, discolored, and brittle. This infection can be challenging to treat and doctors may prescribe antifungal pills.
Tinea Infection Treatment Guidelines Template
Tinea Infection Treatment Guidelines Example
Symptoms of tinea corporis
Tinea corporis, commonly known as ringworm of the body, presents with distinctive symptoms that are typically easy to recognize. The infection often begins as a scaly, ring-shaped area that appears on the buttocks, trunk, arms, or legs. This ring gradually expands outward, with the edges being slightly raised and often more prominent than the center. The area inside the ring may be clear or scaly, and can sometimes include small bumps.
The color of the rash varies depending on skin tone, ranging from red on white skin to reddish, purplish, brown, or gray on black and brown skin. Itchiness is a common symptom, adding to the discomfort caused by this condition. These expanding rings and their distinct appearance are key indicators of tinea corporis, making it easier to identify and treat the infection promptly.
Causes of a ringworm infection
Ringworm, despite its name, is not caused by a worm but by a group of fungi. The most common fungi responsible for ringworm infections belong to the genera Trichophyton, Microsporum, and Epidermophyton. These fungi thrive in warm, moist environments and can easily infect the skin, nails, and scalp. Ringworm spreads through direct contact with an infected person, animal, or contaminated surface. Fungal nail infections, a form of ringworm, occur when these fungi enter the nail through small cracks in the nail or the surrounding skin. Once inside, the fungi can grow and spread, leading to the characteristic symptoms of ringworm.
Tinea infection treatment options
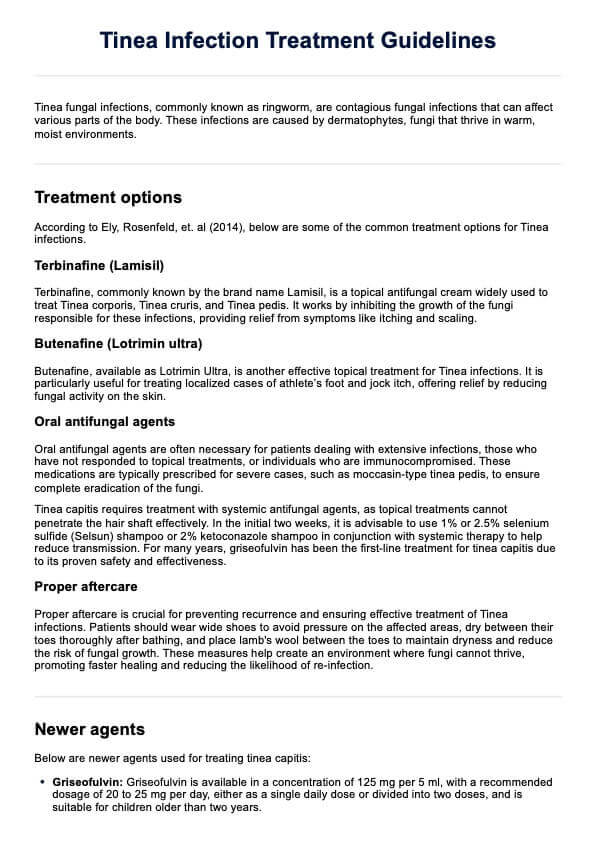
Treating tinea infections effectively requires a combination of topical and oral antifungal medication, along with proper aftercare measures. The treatment approach depends on the type and severity of the infection, as well as the patient's overall health. According to Ely, Rosenfeld, et. al (2014), below are some of the common treatment options for tinea infections.
Terbinafine (Lamisil)
Terbinafine, commonly known by the brand name Lamisil, is a topical antifungal cream widely used to treat tinea corporis, tinea cruris, and tinea pedis. It works by inhibiting the growth of the fungi responsible for these infections, providing relief from symptoms like itching and scaling.
Butenafine (Lotrimin ultra)
Butenafine, available as Lotrimin Ultra, is another effective topical treatment for tinea infections. It is particularly useful for treating localized cases of athlete’s foot and jock itch, offering relief by reducing fungal activity on the skin.
Oral antifungal agents
Oral antifungal agents may be necessary for patients with extensive infections, failed topical treatments, or those who are immunocompromised. These medications are often prescribed for severe cases, such as moccasin-type Tinea pedis, to ensure thorough eradication of the fungi.
Newer agents for tinea capitis and tinea unguiuim
For tinea capitis, Griseofulvin is typically administered at a dosage of 125 mg per 5 ml, with a recommended daily intake of 20-25 mg for children over two. Terbinafine comes in 250 mg tablets and 125 mg granules, with dosages varying according to the child's weight for those aged four and older. Fluconazole is available in various forms and recommended at 6 mg/kg daily for 3-6 weeks, or weekly for children over six months. Itraconazole is offered as a 10 mg/ml solution and 100 mg capsules, with dosages dependent on the form and duration of treatment.
For tinea unguium, Ciclopirox serves as a topical treatment for individuals over 12, applied daily. Fluconazole can also be utilized, with dosages of 3-6 mg/kg weekly for children and 150-300 mg weekly for adults.
Other treatments
Patients dealing with chronic or recurrent tinea pedis can find relief by wearing wide shoes, thoroughly drying their toes after bathing, and placing lamb's wool between them. For individuals with tinea gladiatorum, a common variant of tinea corporis seen in wrestlers, it is crucial to apply topical treatment for 72 hours before returning to wrestling activities.
Proper aftercare
Proper aftercare is crucial for preventing recurrence and ensuring effective treatment of tinea infections. Patients should wear wide shoes to avoid pressure on the affected areas, dry between their toes thoroughly after bathing, and place lamb's wool between the toes to maintain dryness and reduce the risk of fungal growth. These measures help create an environment where fungi cannot thrive, promoting faster healing and reducing the likelihood of re-infection.
How this handout may benefit healthcare providers
Using Carepatron's Tinea Infection Treatment Guidelines handout can provide healthcare providers with valuable tools and resources to enhance patient care and streamline treatment processes. Below are three key benefits that medical professionals can gain from using this handout.
Enhanced patient education
The handout offers clear and concise information on tinea infection treatment, making it easier for healthcare providers to educate their patients. Providers can help patients better understand skin conditions, treatment options, and the importance of adhering to prescribed care plans. This improved understanding can lead to more effective treatment outcomes and greater patient satisfaction.
Streamlined treatment planning
Carepatron's Tinea Infection Treatment handout serves as a comprehensive guide, helping healthcare providers quickly reference the most appropriate treatments for various types of tinea infections. This streamlined approach ensures that patients receive timely and effective care, reducing the need for trial-and-error methods and allowing for a more efficient clinical workflow.
Improved documentation and follow-up
The handout also aids in documentation and follow-up care by providing a structured format for recording treatment plans and patient progress. This organized approach helps healthcare providers track treatment effectiveness, make necessary adjustments, and ensure that patients are on the right path to recovery. By using the handout, providers can maintain thorough and consistent records, improving overall patient management.
Reference
Ely, J. W., Rosenfeld, S., & Stone, M. S. (2014). Diagnosis and management of tinea infections. American Family Physician, 90(10), 702–711. https://www.aafp.org/pubs/afp/issues/2014/1115/p702.htmlp702.html
Commonly asked questions
Yes, ringworm is a contagious fungal infection that can spread through direct skin-to-skin contact with an infected person or animal. It can also be transmitted by touching contaminated surfaces, such as gym equipment, towels, or clothing.
If ringworm goes untreated, it can lead to more severe symptoms, including widespread skin irritation, inflammation, and secondary bacterial infections. The infection may also become chronic, making it more difficult to treat ringworm and manage over time.
Ringworm remains contagious as long as the infected person has visible symptoms, such as rashes or lesions. Generally, it can take about 24 to 48 hours after starting appropriate treatment for the infection to become less contagious.
Tinea often presents as circular, red, and scaly patches with raised edges, giving it a ring-like appearance. The center of the affected area may appear clear or scaly, and the color can vary depending on skin tone, ranging from red on lighter skin to reddish-brown or purplish on darker skin.