Bilirubin Levels
Monitor, assess, and manage bilirubin levels effectively through Bilirubin Levels Charts. Discover more about this life-saving tool.


What are bilirubin levels?
Bilirubin levels in the blood offer a crucial insight into a person's liver function, overall health, and potential issues with the breakdown or excretion of red blood cells. Essentially, bilirubin is a yellowish substance the body creates when red blood cells break down. The liver is vital in processing this compound, making its levels a valuable diagnostic indicator.
Bilirubin production happens when red blood cells reach the end of their lifecycle, around 120 days. They are broken down, releasing hemoglobin, which is then converted into bilirubin.
Bilirubin levels may build up because of obstructed bile ducts, which may lead bile build up in the liver and cause jaundice.
Interpreting bilirubin levels in the context of a patient's medical history, physical examination, and other laboratory and diagnostic tests is essential to determining the underlying cause and guiding appropriate treatment.
What is the difference between conjugated and unconjugated bilirubin?
There are two primary forms of bilirubin:
- Unconjugated (indirect) bilirubin: This form is insoluble and cannot be excreted in bile or urine. It is transported to the liver, where it undergoes conjugation (binding to a sugar molecule) to become soluble.
- Conjugated (direct) bilirubin: This form is soluble and can be excreted through bile and urine. It is produced in the liver when unconjugated bilirubin is conjugated. Elevated levels can impact bilirubin excretion and can be associated with diseases such as Rotor syndromes and other types of liver disease.
Elevated bilirubin levels can indicate conditions like hemolytic anemia or liver diseases impairing conjugation or uptake. Elevated levels of conjugated bilirubin may suggest biliary tract obstruction or liver disease that impairs bile excretion (Wehbi, 2020). This can then impact the body's excretion processes, which can be noted through the appearance of dark urine, delayed passage of meconium, and pale stools.
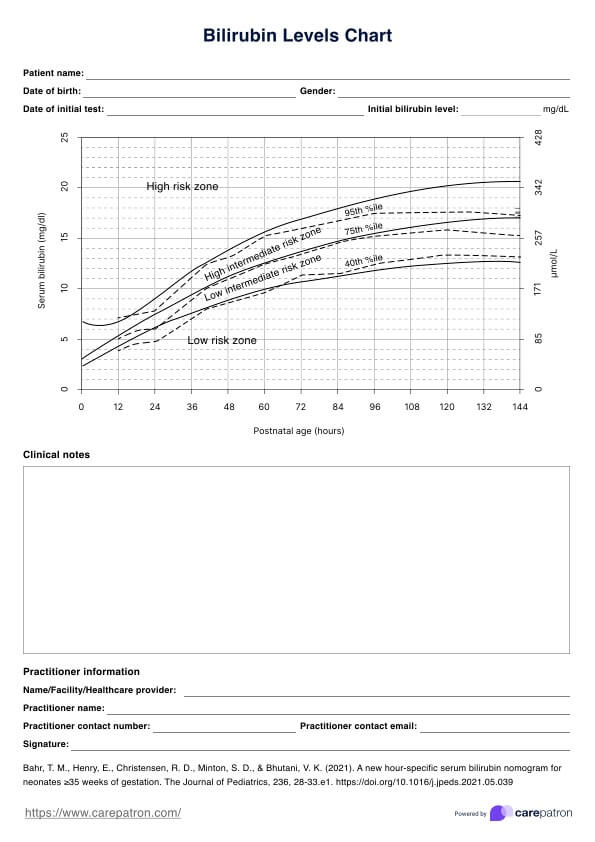
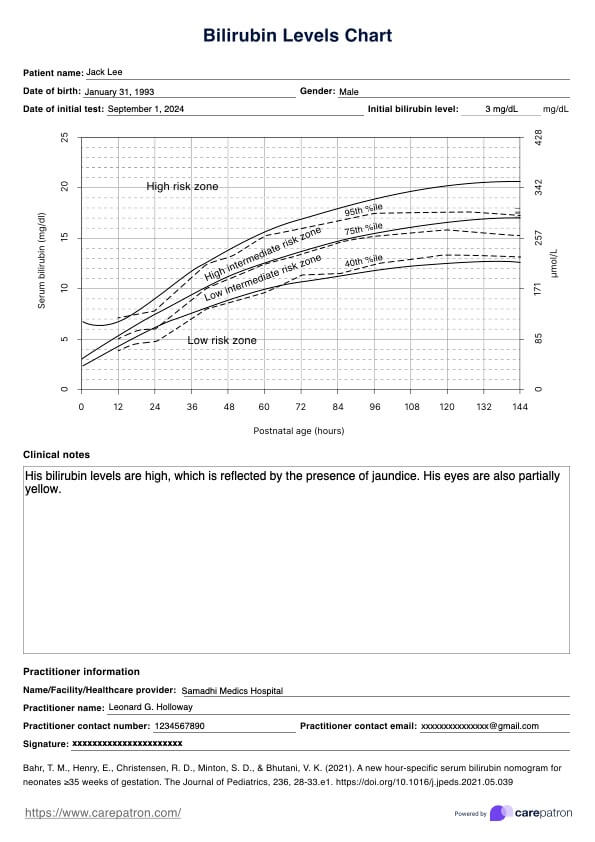
Bilirubin Levels Chart Template
Bilirubin Levels Chart Example
What is a Bilirubin Levels Chart?
A Bilirubin Levels Chart, also known as a bilirubin nomogram, evaluates the total amount of serum bilirubin in a newborn's bloodstream. This chart aids healthcare professionals in diagnosing jaundice, a common condition in infants. This tool can help healthcare professionals with the treatment that may be necessary to decrease bilirubin levels.
How to use our Bilirubin Levels Chart?
Using a Bilirubin Levels Chart is a straightforward process that can provide valuable insights into the interpretation and management of neonatal hyperbilirubinemia. Here's a step-by-step guide on how to use a Bilirubin Levels Chart effectively:
Step 1: Determine potential heightened bilirubin levels
A physical exam of the infant should be conducted, and it should involve bilirubin tests. First, the practitioner will inspect the skin for the extent of jaundice, typically using gentle pressure to help reveal the presence of the condition.
Step 2: Take necessary medical steps
Bilirubin levels can be measured using typical medical practices. Once the initial blood test returns, the healthcare professional can plot the levels of bilirubin found in the bloodstream against the individual's age.
Step 3: Complete the Bilirubin Levels Chart
Use Carepatron's printable Bilirubin Levels Chart to get a clear visual of how the bilirubin level is progressing within the individual. Repeat the process as many times as medically needed. The graph will begin to take shape, and practitioners will be able to see a progression line as the graph continues to be filled in.
Step 4: Plan for appropriate treatment
Utilize the data gathered on the Bilirubin Levels Chart to make necessary treatment decisions based on the bilirubin levels. Examples of next steps may include phototherapy and exchange transfusion, or conducting other tests to check for any underlying conditions influencing bilirubin levels in a patient.
Measuring levels through a bilirubin blood test
A bilirubin blood test measures bilirubin levels. The procedure entails the collection of a blood sample from the patient, which is subsequently dispatched to a specialized laboratory for comprehensive analysis. There are two types of Bilirubin Blood Test (Wehbi, 2020):
- Total bilirubin (TBil): This measures both unconjugated and conjugated (direct) bilirubin. Normal bilirubin levels typically fall between 0.2 to 1.2 mg/dL.
- Direct bilirubin (Dbil): Specifically measuring conjugated bilirubin, normal levels are usually under 0.3 mg/dL.
These total and direct bilirubin levels can then be interpreted as the following:
- Normal levels: As mentioned, fall within the ranges of 0.2 to 1.2 mg/dL for total bilirubin and up to 0.3 mg/dL for direct bilirubin.
- High bilirubin levels: Elevation can indicate several conditions. An increase in unconjugated bilirubin may suggest hemolytic anemias or Gilbert's syndrome, while elevated conjugated bilirubin could indicate liver diseases such as hepatitis, cirrhosis, or bile duct obstruction.
How are bilirubin levels measured in newborns?
Measuring the total serum bilirubin level in newborn babies is crucial for identifying and managing physiological jaundice or breastfeeding jaundice. This common condition can potentially lead to severe complications if left untreated. Several methods are used to measure newborns' bilirubin levels, each with advantages and limitations.
- Transcutaneous bilirubinometry (TcB): This noninvasive method uses a handheld device to estimate serum bilirubin level by measuring the yellowish discoloration of the baby's skin and subcutaneous tissues. The device is placed on the newborn's forehead or sternum, emitting light waves absorbed by the bilirubin in the skin. The device then calculates the baby's bilirubin level based on light absorption (Kuzniewicz et al., 2009).
- Total serum bilirubin (TSB) blood test: This directly measures the total bilirubin concentration in the newborn's serum or plasma. It is considered the gold standard for bilirubin measurement and provides accurate results. The baby's blood sample is collected through heel prick or venipuncture and analyzed in a laboratory (Bhutani & Wong, 2013). While measuring total serum bilirubin levels is the most accurate method, it is invasive and can cause discomfort to the newborn.
- End-tidal carbon monoxide (ETCOc) measurement: This method indirectly measures bilirubin levels by quantihemolysis rate hemolysis (breakdown of red blood cells). It involves measuring the concentration of carbon monoxide in the newborn's exhaled breath, which is a byproduct of heme degradation (Christensen et al., 2016).
When interpreting the results of a bilirubin test in newborns, healthcare professionals consider factors such as gestational age and postnatal absence of risk factors for hyperbilirubinemia (elevated bilirubin levels). A newborn bilirubin chart can also be a helpful tool in this process. Timely identification and management of neonatal jaundice are crucial to prevent potential complications, such as acute bilirubin encephalopathy (kernicterus) (Bhutani & Wong, 2013).
Why is measuring bilirubin levels necessary?
Measuring bilirubin levels is essential for several reasons in healthcare practice. It provides valuable insights into various medical conditions and helps guide appropriate diagnosis and management.
Identifying hemolytic disorders
When bilirubin levels remain high for a significant period, this can indicate liver diseases that affect bile excretion, such as hepatitis, cirrhosis, or biliary obstruction. It can also indicate conditions affecting the liver's ability to process bilirubin.
Monitoring newborn jaundice
In newborns, jaundice occurs when there is an excessive buildup of bilirubin in the blood. Measuring bilirubin levels is essential for detecting and managing breast milk jaundice, a common condition caused by the breakdown of excess red blood cells. Timely intervention can prevent potential complications as jaundice occurs, such as kernicterus (brain damage) (Bhutani & Wong, 2013).
Tracking treatment response
Bilirubin levels can be used to monitor the effectiveness of treatments for conditions like hemolytic anemia, liver diseases, or biliary tract obstruction. A decrease in bilirubin levels can indicate a positive response to treatment.
References
Bhutani, V. K., & Wong, R. J. (2013). Bilirubin neurotoxicity in preterm infants: risk and prevention. Journal of Clinical Neonatology, 2(2), 61–69. https://doi.org/10.4103/2249-4847.116402
Christensen, R. D., Malleske, D. T., Lambert, D. K., Baer, V. L., Prchal, J. T., Denson, L. E., Gerday, E., Weaver, Lewis, K. A., & Shepherd, J. G. (2016). Measuring end-tidal carbon monoxide of jaundiced neonates in the birth hospital to identify those with hemolysis. Neonatology109(1), 1–5. https://doi.org/10.1159/000438482
Kuzniewicz, M.W., Escobar, G.J., & Newman, T.B. (2009). Impact of universal bilirubin screening on severe hyperbilirubinemia and phototherapy use. Pediatrics, 124, 1031 - 1039. https://doi.org/10.1542/peds.2008-2980
Wehbi, M. (2020, March 4). Bilirubin: Reference range, interpretation, collection, and panels. Medscape. https://emedicine.medscape.com/article/2074068-overview
Commonly asked questions
A safe bilirubin level for adults is generally below 1.5 mg/dL. Bilirubin levels above this threshold can indicate liver dysfunction or other underlying medical conditions. In adults, bilirubin levels above 2.5 mg/dL may be considered toxic and can lead to complications such as jaundice, liver damage, and even liver failure.
A toxic level of bilirubin in adults is typically considered to be above 3.5 mg/dL. At this level, bilirubin can accumulate in the brain and other organs, leading to severe complications such as kernicterus, a condition characterized by brain damage and intellectual disability. Bilirubin levels above 5 mg/dL are often considered life-threatening and require immediate medical attention.
A Bilirubin Levels in Newborns Chart would consider below 12 mg/dL as an acceptable bilirubin level among newborns. Newborns have increased bilirubin production compared to adults due to the breakdown of fetal hemoglobin, which is rich in bilirubin. Bilirubin levels above 15 mg/dL in newborns can indicate jaundice, which is a common condition in newborns. In severe cases, bilirubin levels above 20 mg/dL may require phototherapy or exchange transfusion to prevent complications.