Depending on the patient's symptoms and medical history, various healthcare practitioners, including cardiologists, hepatologists, oncologists, and primary care physicians, can request an LDH Blood Test.
LDH Blood
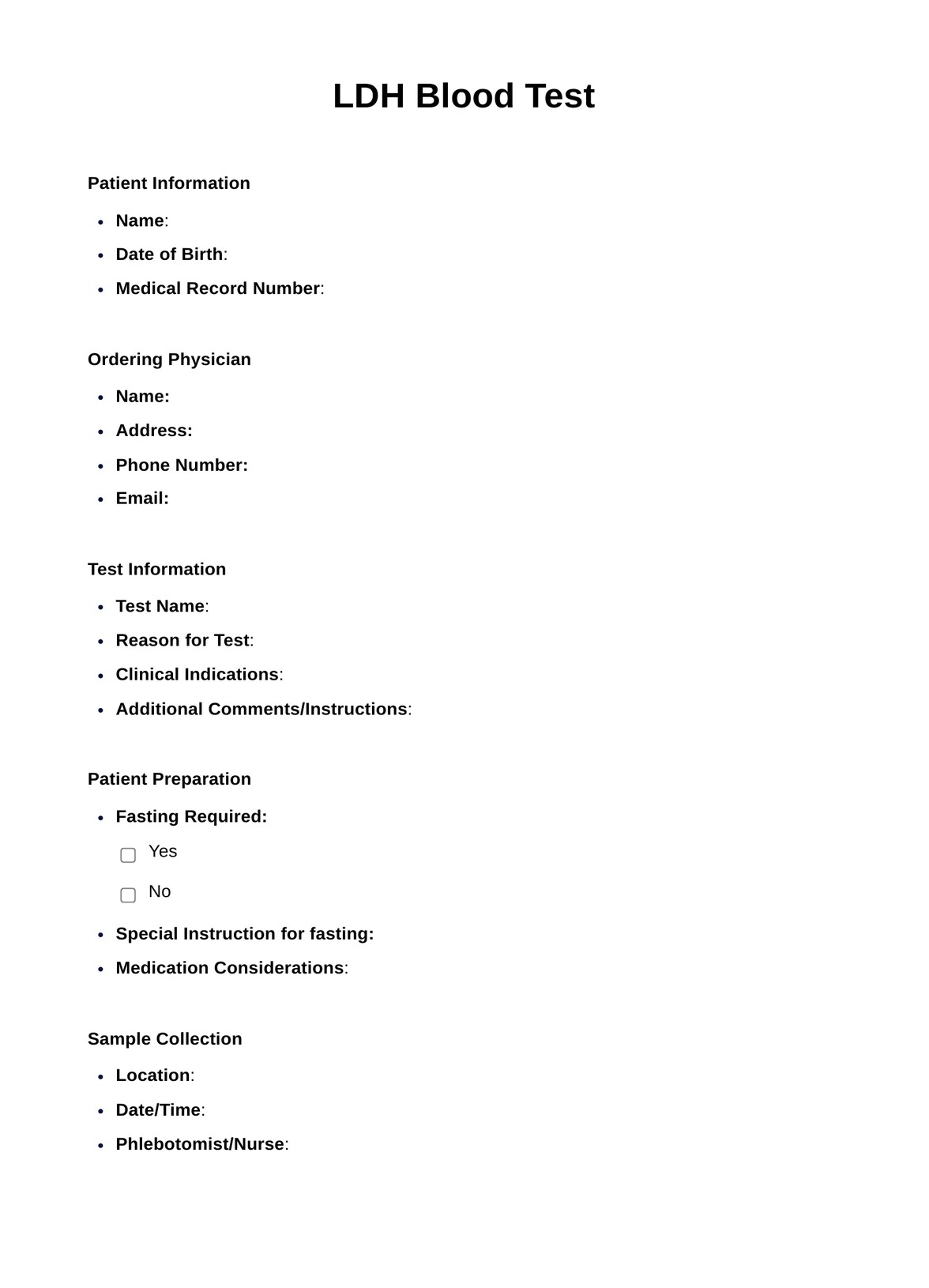
Discover the significance of LDH Blood Test results. Learn about normal ranges and clinical implications for accurate health assessment.
LDH Blood Template
Commonly asked questions
LDH Blood Tests are used when there is suspicion of tissue damage or disease in organs like the heart, liver, muscles, or cases of certain cancers. They aid in diagnosis, monitoring, and treatment assessment.
LDH Blood Tests involve collecting a blood sample from a patient's vein, which is then processed in a clinical laboratory to measure LDH enzyme levels. Results help healthcare providers identify tissue damage or underlying medical conditions.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











