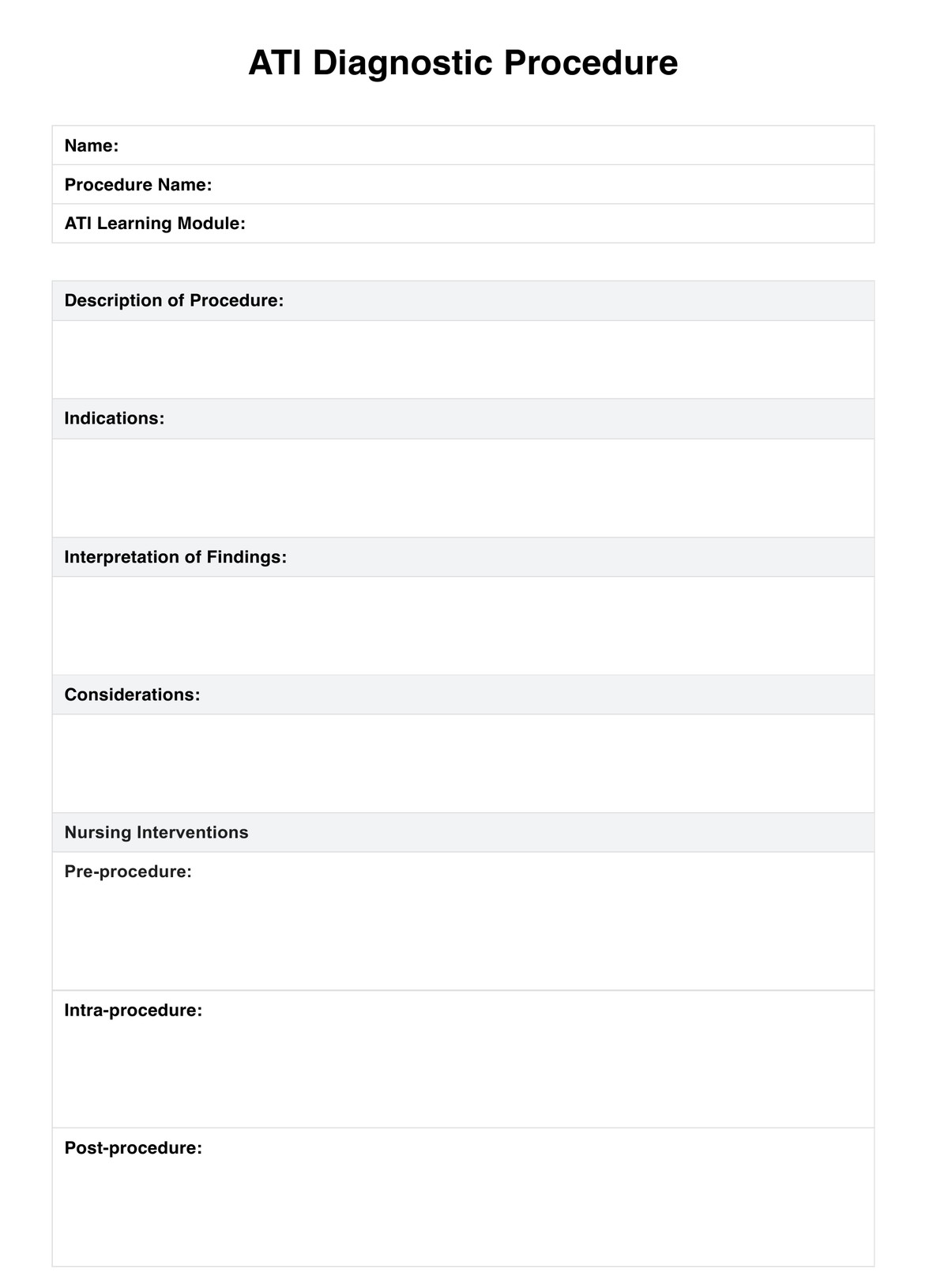
ABCDE Assessment
Document your patient's condition and your interventions on our ABCDE Assessment template.


What is the ABCDE Assessment?
The Airway, Breathing, Circulation, Disability, and Exposure (ABCDE) Assessment is a standard examination in any hospital or clinic with a resuscitation room. This initial assessment aims to examine critically ill patients who have been rushed into the emergency room, resuscitation room, or critical care setting due to an illness or an injury. It is a systematic method of identifying and addressing life-threatening problems, often included in adult advanced life support, to keep patients with a critical illness alive and buy doctors enough time to diagnose and treat patients so they can hopefully survive.
The assessment is divided into the following:
- Airway: The assessment conductors will check for foreign bodies and swollen tissues obstructing the patient’s airways.
- Breathing: After confirming that the airway is not obstructed, the medical team will check the patient’s breathing by gauging their respiratory rate, whether they have any chest deformities and even their oxygen status.
- Circulation: For this part of the assessment, the medical team will gauge the patient’s heart rate, blood circulation, and blood pressure. They will also check if the critically ill patient has hypovolemia and hemorrhages or any sign of poor cardiac output, such as prolonged CRT that indicates poor peripheral perfusion.
- Disability: The penultimate part of this assessment involves the medical team gauging the patient for any neurological damage caused by their illness or injury by examining their motor responses, pupil reactions, and level of consciousness.
- Exposure: The final part of this assessment will have the team expose their patient (removing their clothes) while prioritizing their dignity and maintaining their body heat to check the patient's temperature, bruises, rashes, bleeding, etc.
These will be done urgently to improve patient outcomes and give them a good chance of surviving.
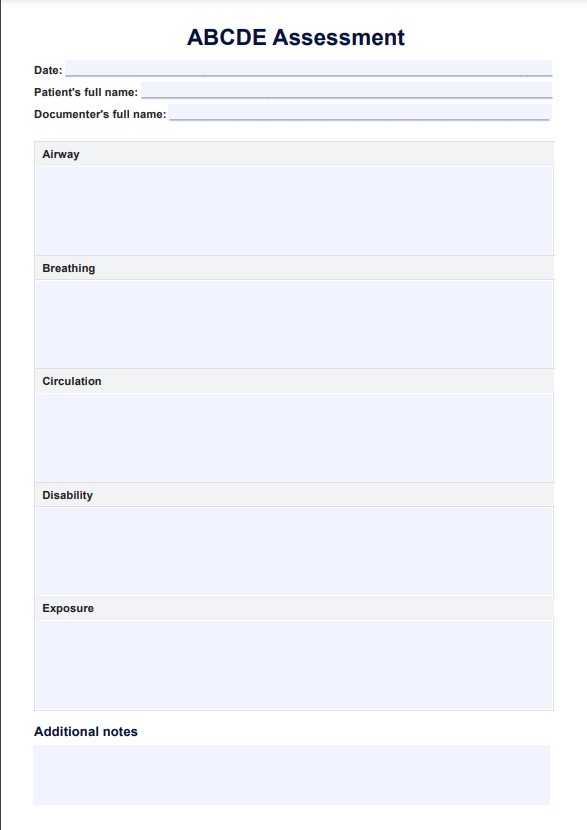
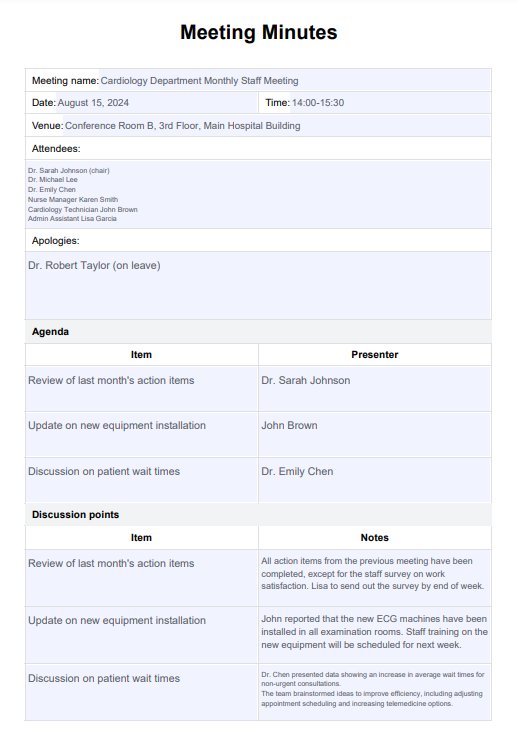
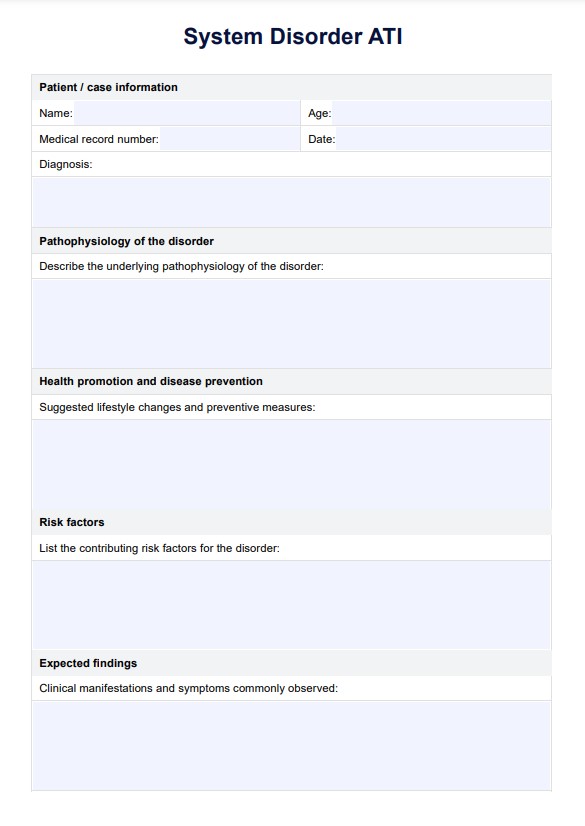
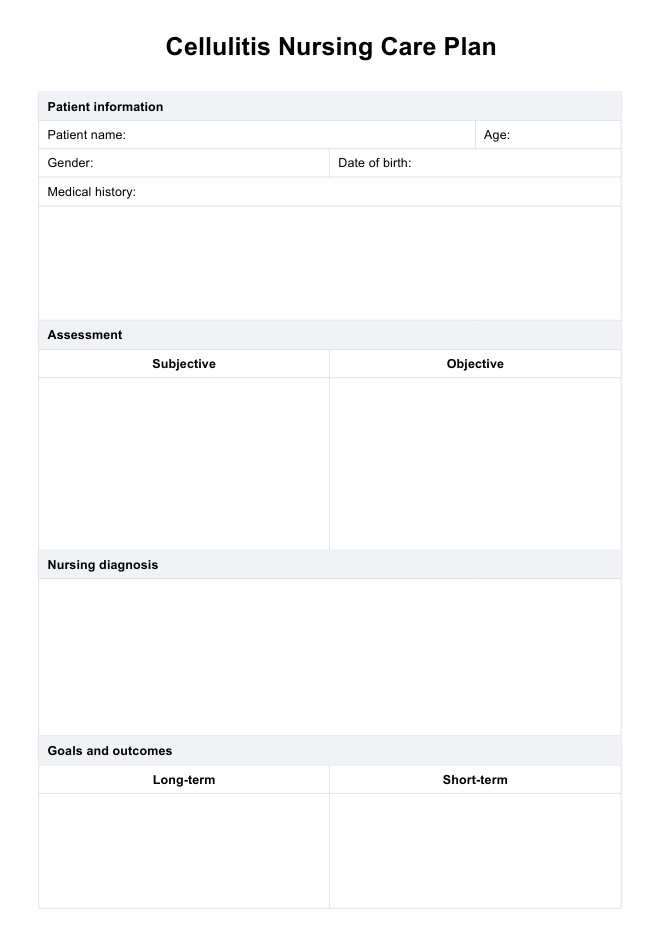
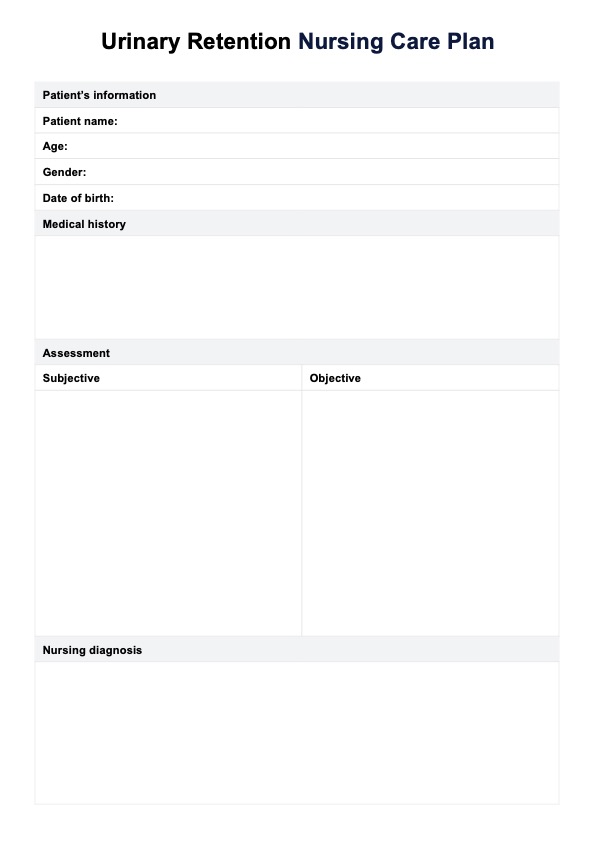
ABCDE Assessment Template
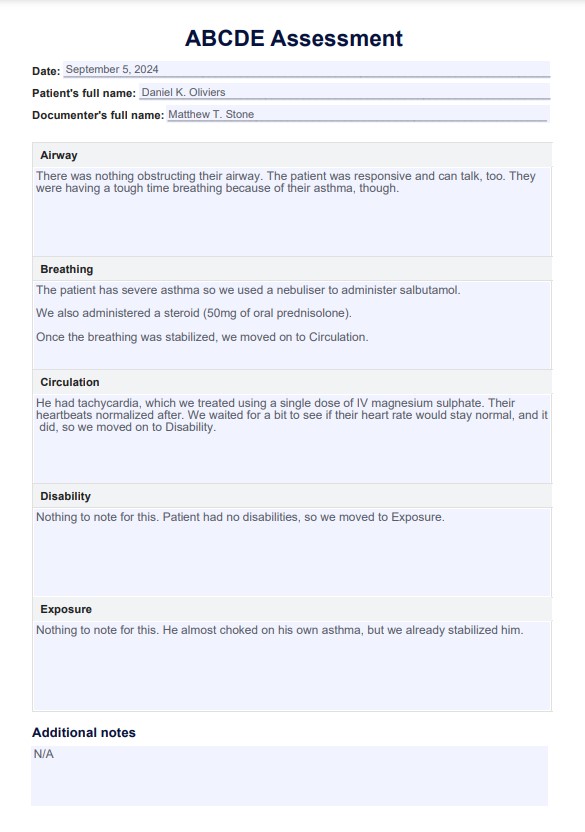
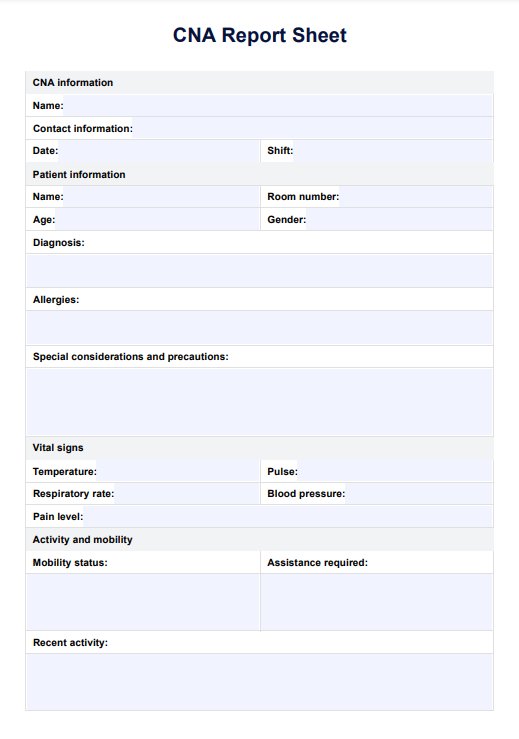
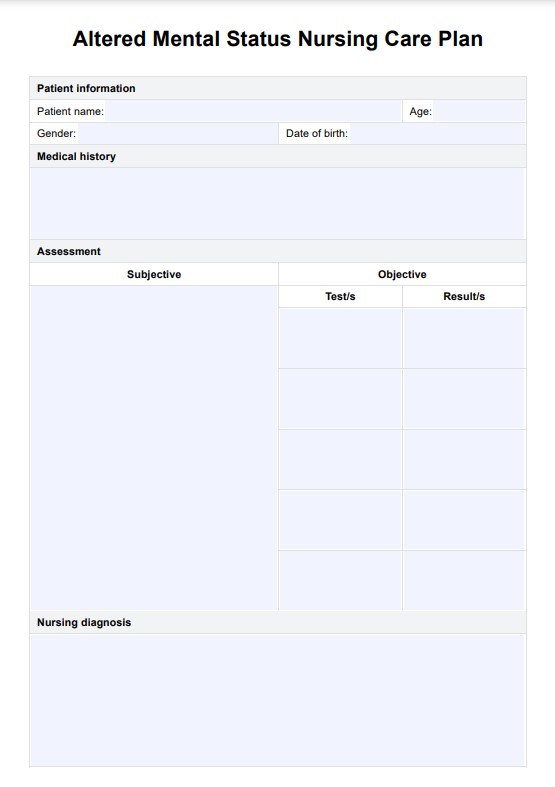
ABCDE Assessment Example
How the ABCDE Assessment works
The ABCDE Assessment is a straightforward procedure that must be done in order to ensure that the patient is well taken care of during emergencies. To help you out, here's a rundown of what to do during every step of the assessment:
Step 1: Assess airway
The medical team must check if the patient can talk or not, especially if the patient appears unconscious. If they can, the team will move on to Breathing. If not, they need to check for signs of airway obstruction, such as:
- See-saw respirations
- Central cyanosis
- Use of accessory muscles
- Diminished breath sound
The team must also open the patient's mouth to inspect for foreign bodies, blood, vomit, etc., that may obstruct the airway and cause brain damage, cardiac arrest, etc.
If the patient has an airway obstruction, the conductor must ask for support from their team so that appropriate interventions can be provided. Examples of intervention are CPR, head-tilt x chin-lift maneuver, jaw thrust, oropharyngeal airway, and nasopharyngeal airway.
After enacting the necessary interventions, the medical team must reassess the patient's airway before Breathing.
Step 2: Check breathing
For this part of the assessment, the medical team needs to assess the following:
- The patient's respiratory rate (normal rate should be 12 to 20 breaths per minute)
- Oxygen saturation (normal rate should be 94 to 98%) for healthy patients and 88 to 92% for patients with chronic obstructive pulmonary disease (COPD).
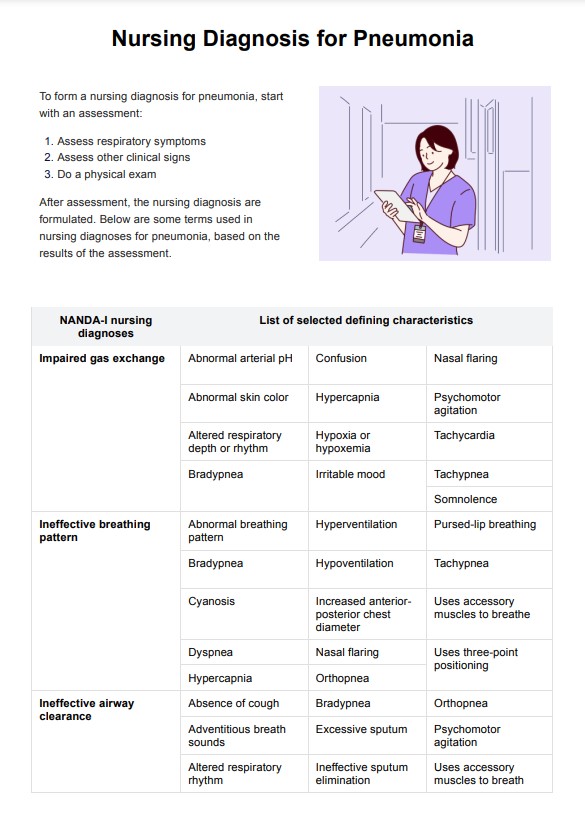
They must also inspect to check for bradypnoea, tachypnoea, hypoxemia, cyanosis, stridor, coughs, shortness of breath, Kussmaul's respiration, and Cheyne-Stokes's respiration.
These can be assessed by doing the following:
- Gently assessing the position of the trachea
- Assessing the patient's chest expansion when they breathe
- Percussing the patient's chest
- Auscultating the patient's chest
- Taking arterial blood gas if the oxygen saturation is not normal
- X-rays to check for pathologies
If interventions are required, the medical team can consider CPR if the patient falls unconscious, Providing supplementary oxygen, steroids, and using a nebulizer for those with asthma, Antibiotics
Like with the first one, the patient must be reassessed after interventions have been implemented before moving to Circulation.
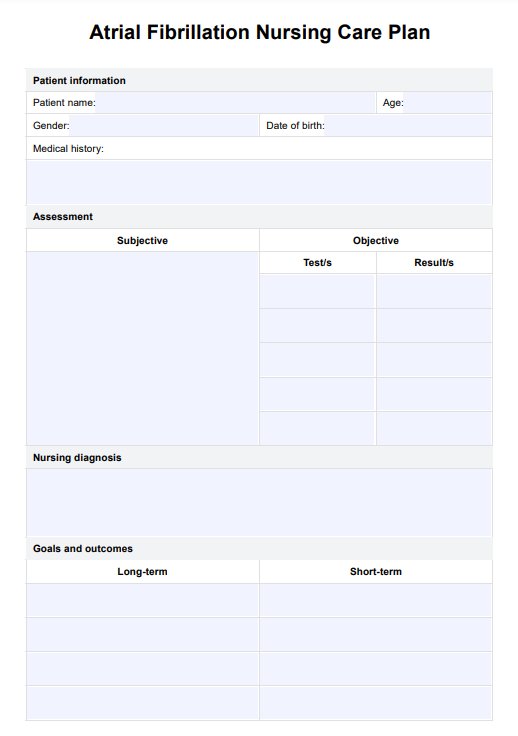
Step 3: Check circulation
For this part of the assessment, the medical team will check the following:
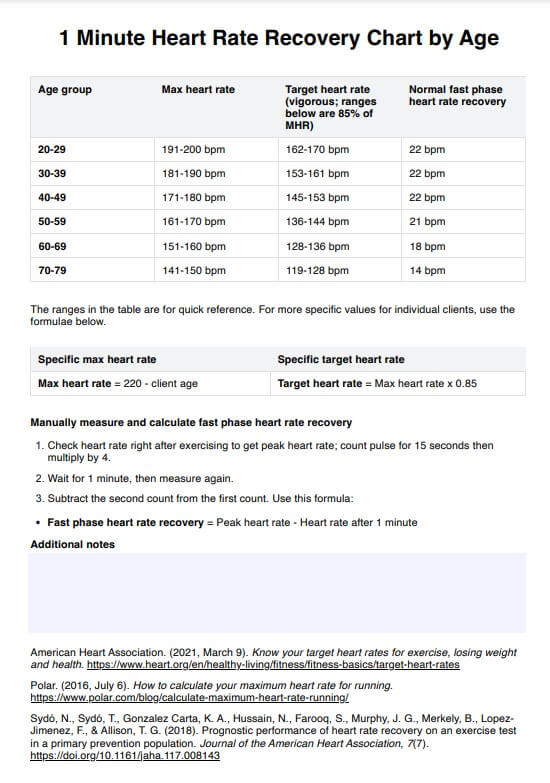
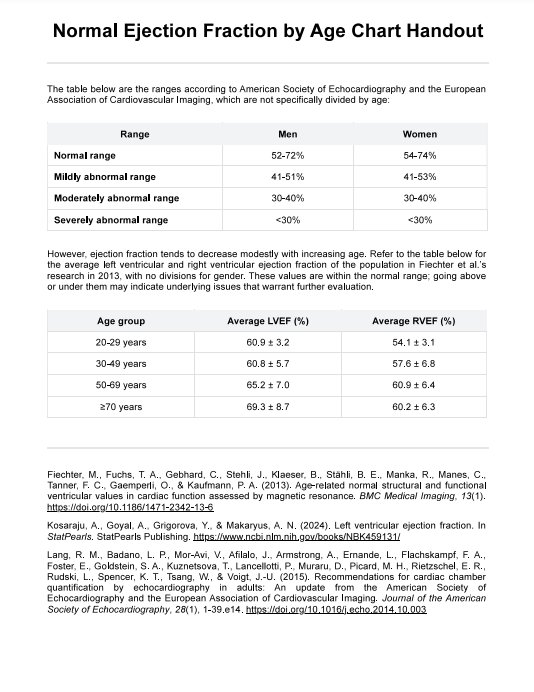
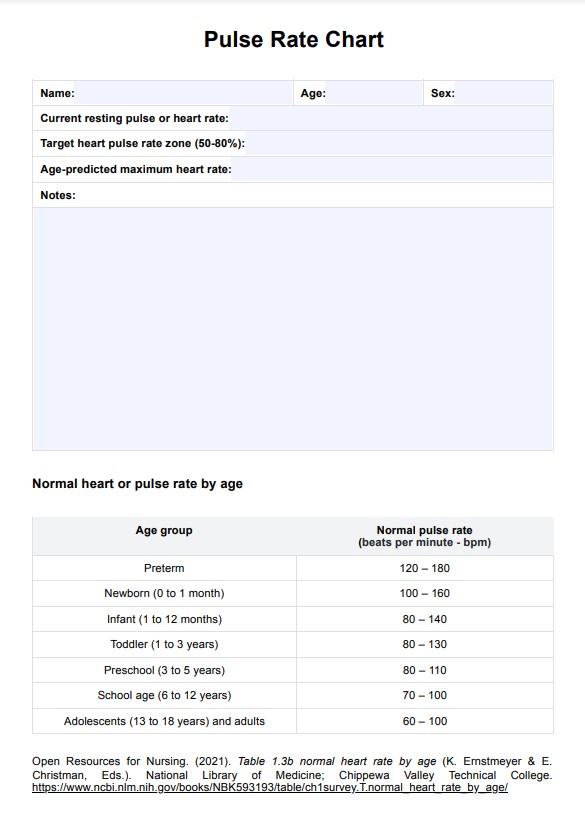
- The patient's heart rate (normal is 60-99 beats per minute)
- The patient's blood pressure (normal is 90/60mmHg and 140/99mmHg)
- Calculate the patient's current fluid balance
They must also conduct an inspection to check if they have tachycardia, bradycardia, hypertension, hypotension, pallor, edema, heart failure, acute coronary syndrome, or jugular venous pressure.
They can inspect the aforementioned problems and more by doing the following:
- Blood tests
- Intravenous cannulation
- ECG monitoring
- Bladder scan
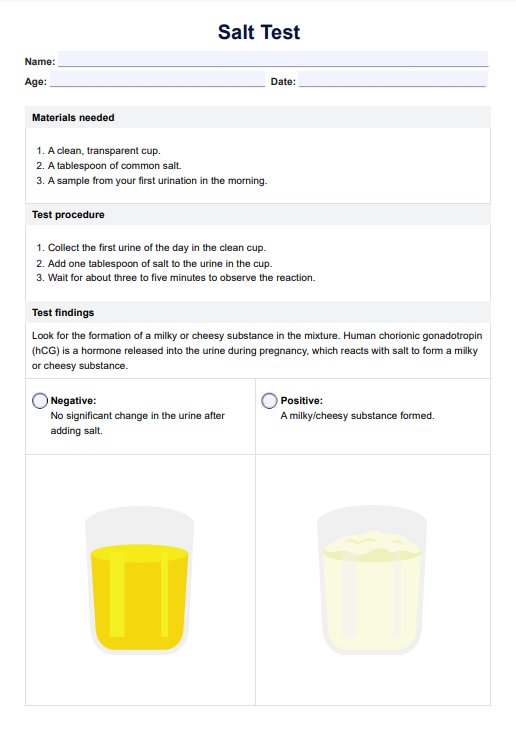
- Urine pregnancy tests for females
- Collecting of culture/swabs
- Catheterization
Possible interventions required depending on problems found are:
- CPR if patients are unconscious or lose consciousness
- Fluid resuscitation
- Pain relief
- Nitrates
- Aspirin
- Clopidogrel
- Supplementary oxygen
- Sepsis 6 Pathway
- Diuretics
- Replacing intravascular volume
- Controlling the heart rate and rhythm
After implementing interventions, they must reassess the patient's response in terms of Circulation before moving to Disability.
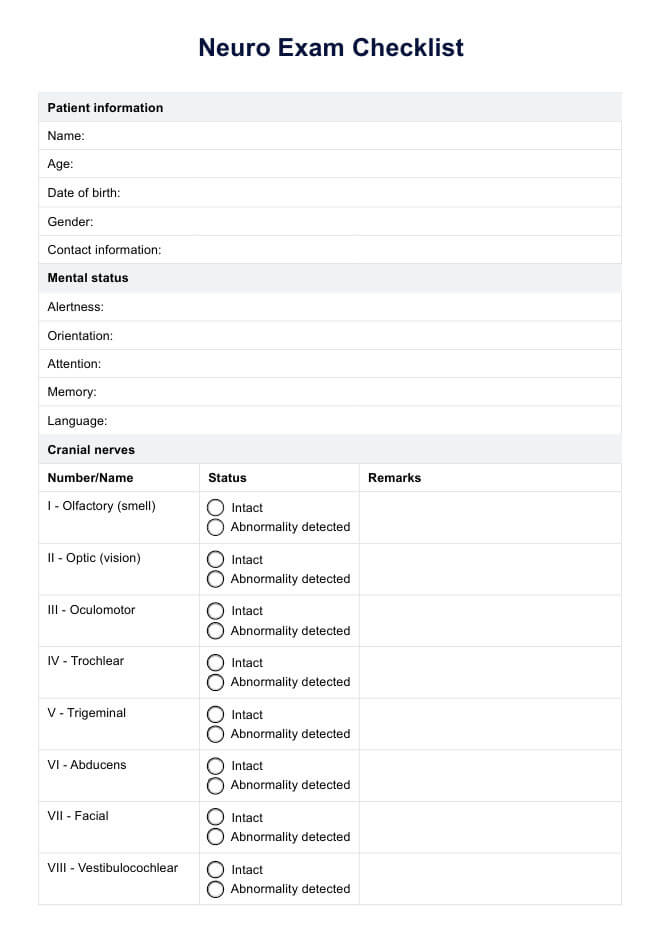
Step 4: Assess disability
For this part of the assessment, the medical team needs to check the patient for the following:
- Their level of consciousness
- The size and symmetry of their pupils
- The responses of their pupils to light
- Review the patient's drug chart to identify medications that might lead to neurological issues
- Capillary blood glucose (normal range is 4.0 to 5.8 mmol/l)
They should also check for:
- Hypoglycemia
- Diabetic ketoacidosis
- Intracranial pathology (via CT head)
- Opioid toxicity
Interventions that can be used for this part of the assessment are:
- CPR for patients who lose consciousness
- Naloxone
- Glucose administration
- Intravenous fluids
- Insulin
After implementing interventions, they must reassess the patient before moving to Exposure.
Step 5: Check for exposure
The medical team will have to undress the patient while prioritizing the patient's dignity and body heat.
They must check the patient for the following:
- Rashes
- Bruises
- Infections
- Erythema
- Discharge
- Swelling
- Tenderness
- Bleeding/hemorrhages
- Body temperature (normal is 36C to 37.9C)
The interventions that can be used for this part of the assessment are:
- CPR (if the patient loses consciousness)
- Blood products
- 2 large-bore intravenous access
- Antibiotics
Once interventions have been implemented, they must reassess the patient.
Step 6: Review, document, and proceed to next steps
After all the procedures are done and the patient has been stabilized, here are the next steps:
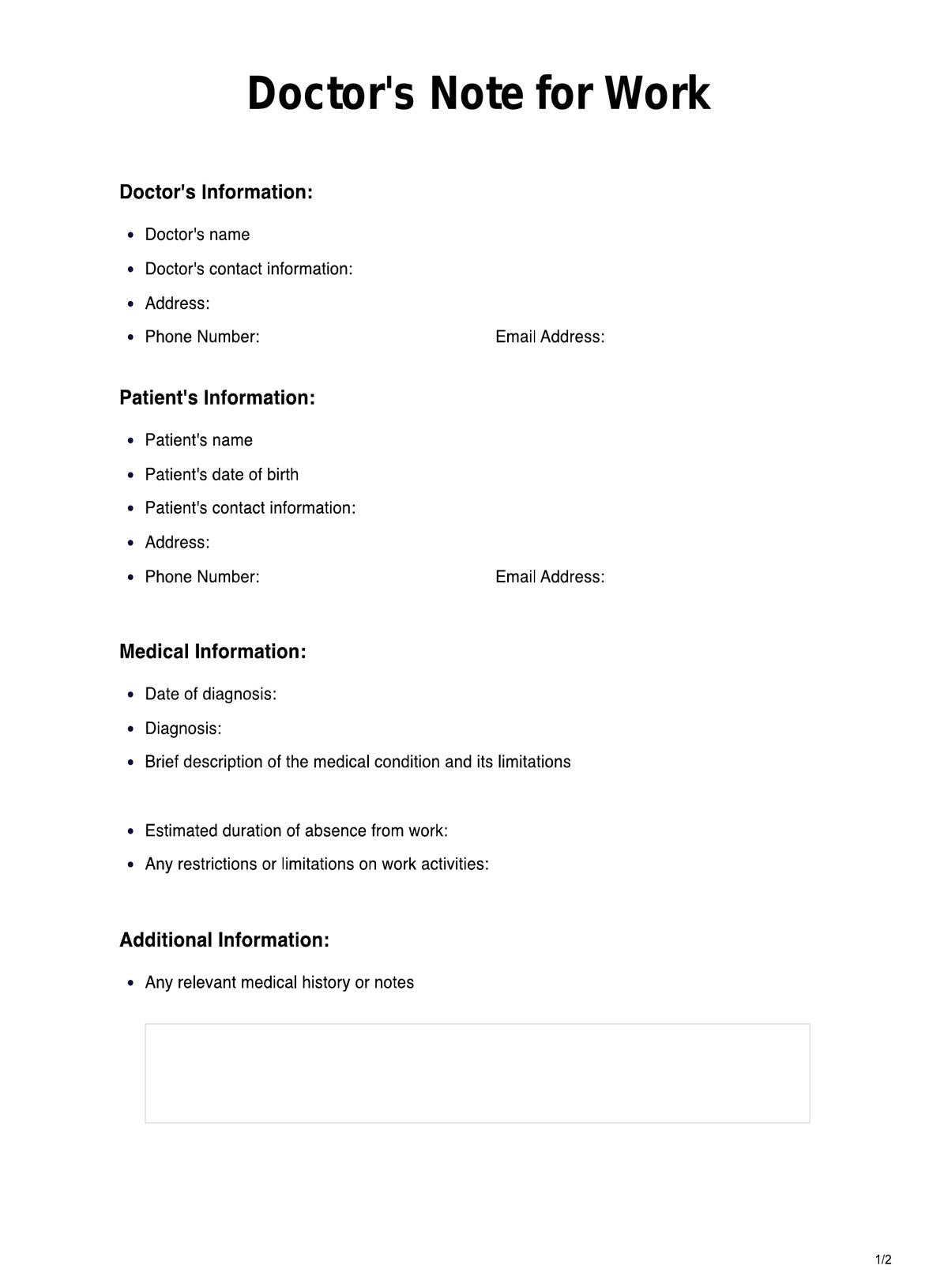
- Take a full clinical history, whether from the relevant parties
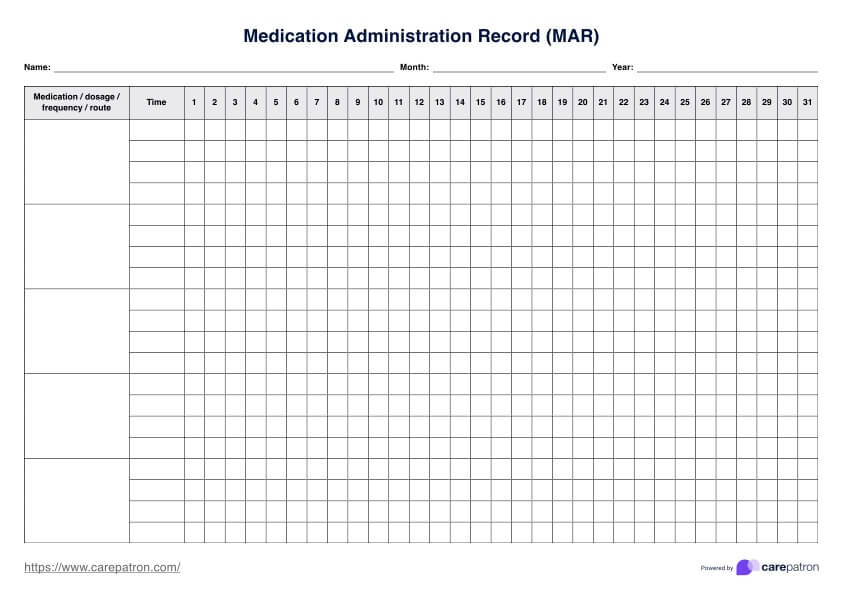
- Review the patient's notes, charts, recent investigation results, current medications, and prescribed medications
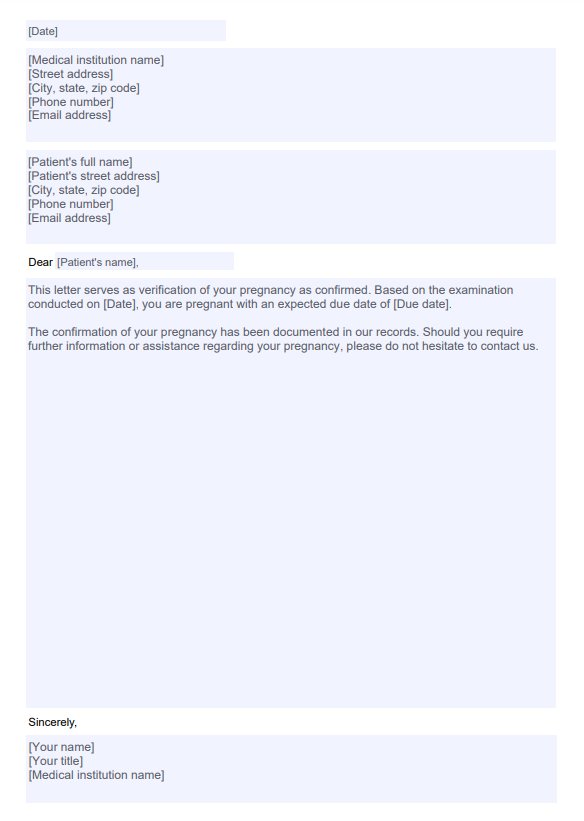
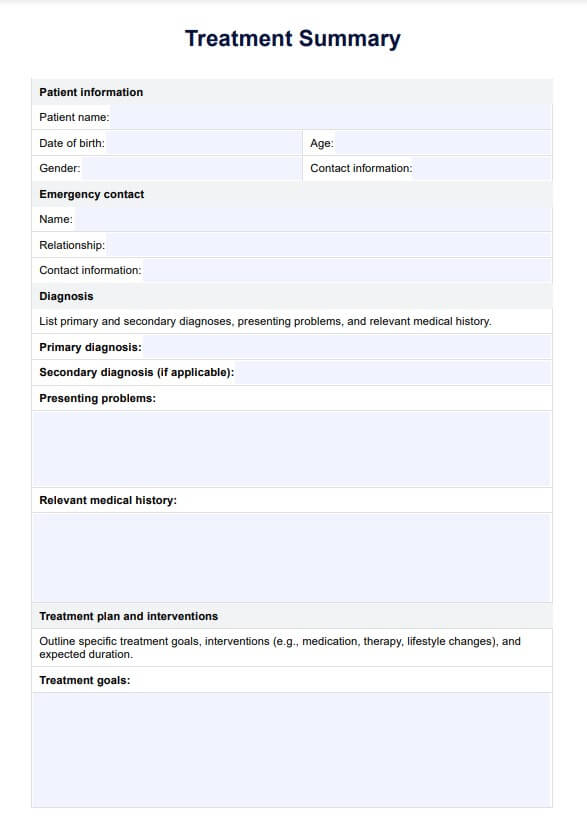
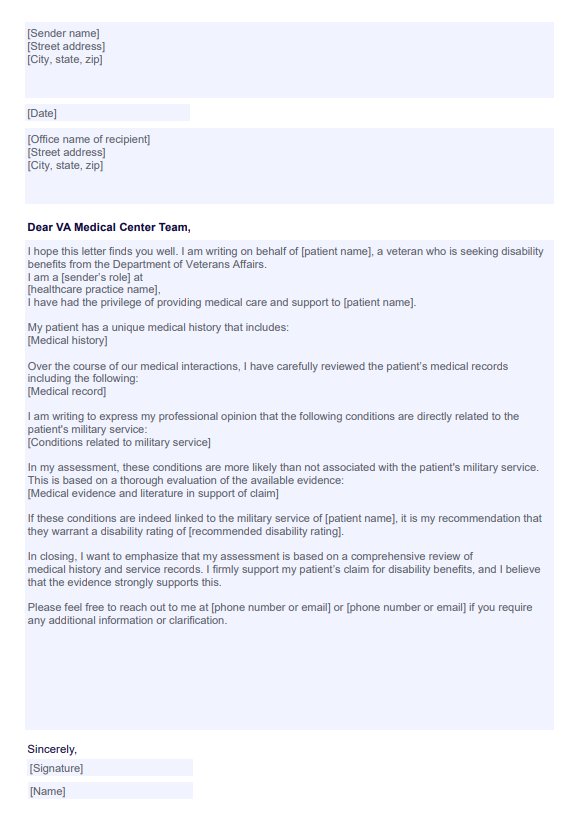
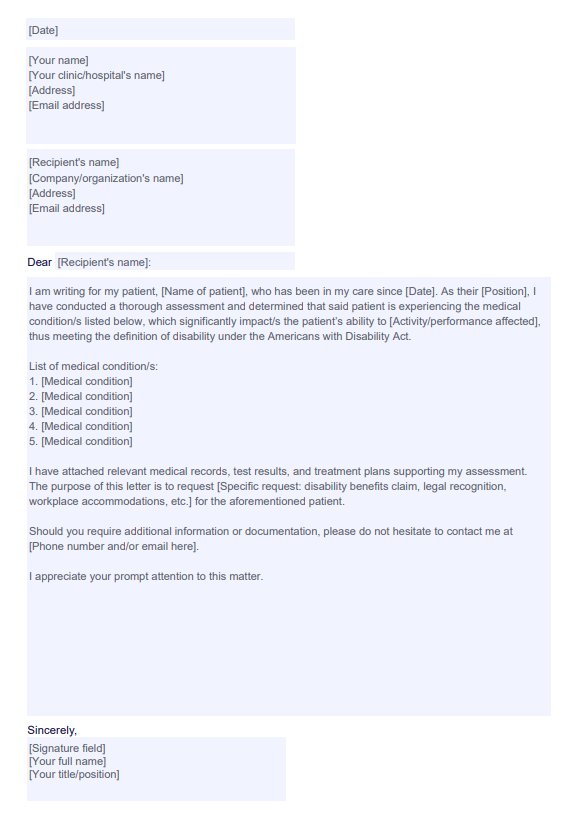
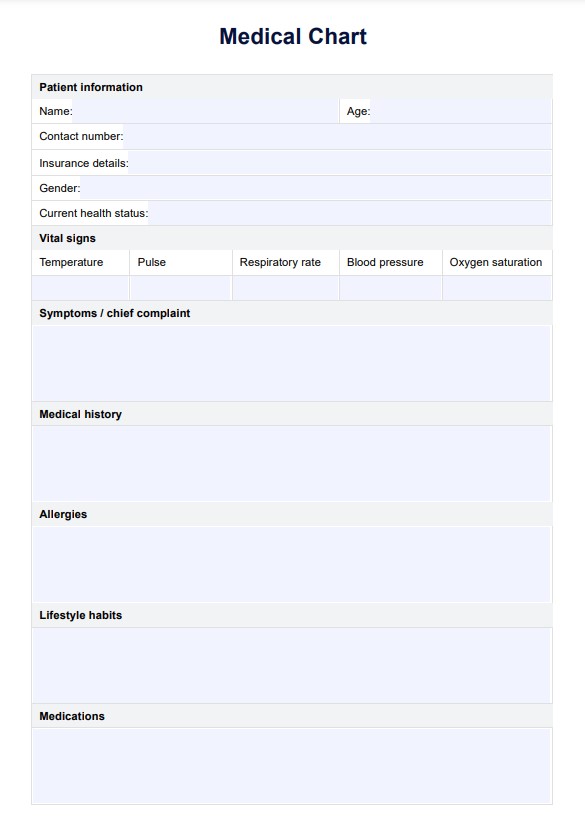
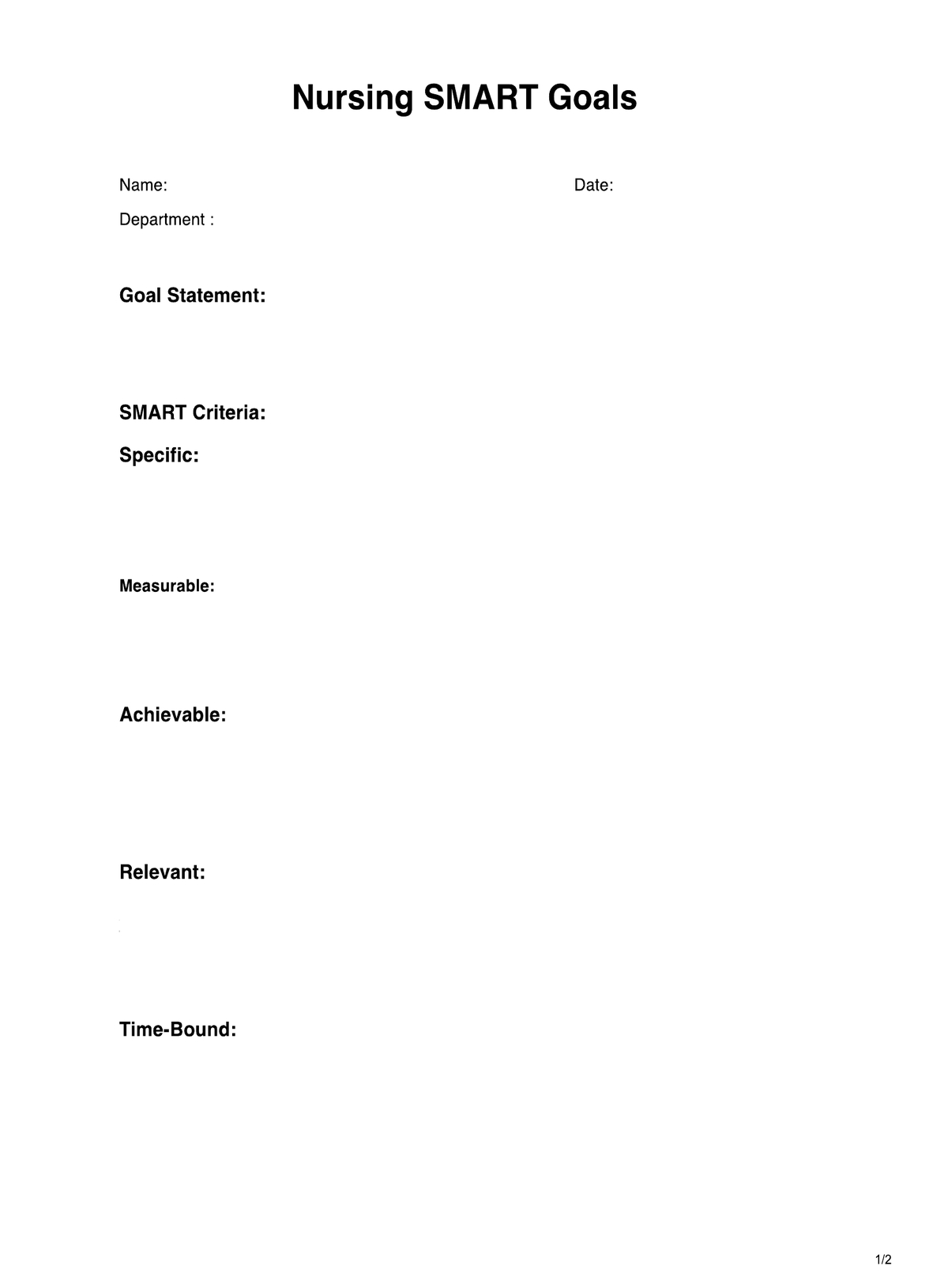
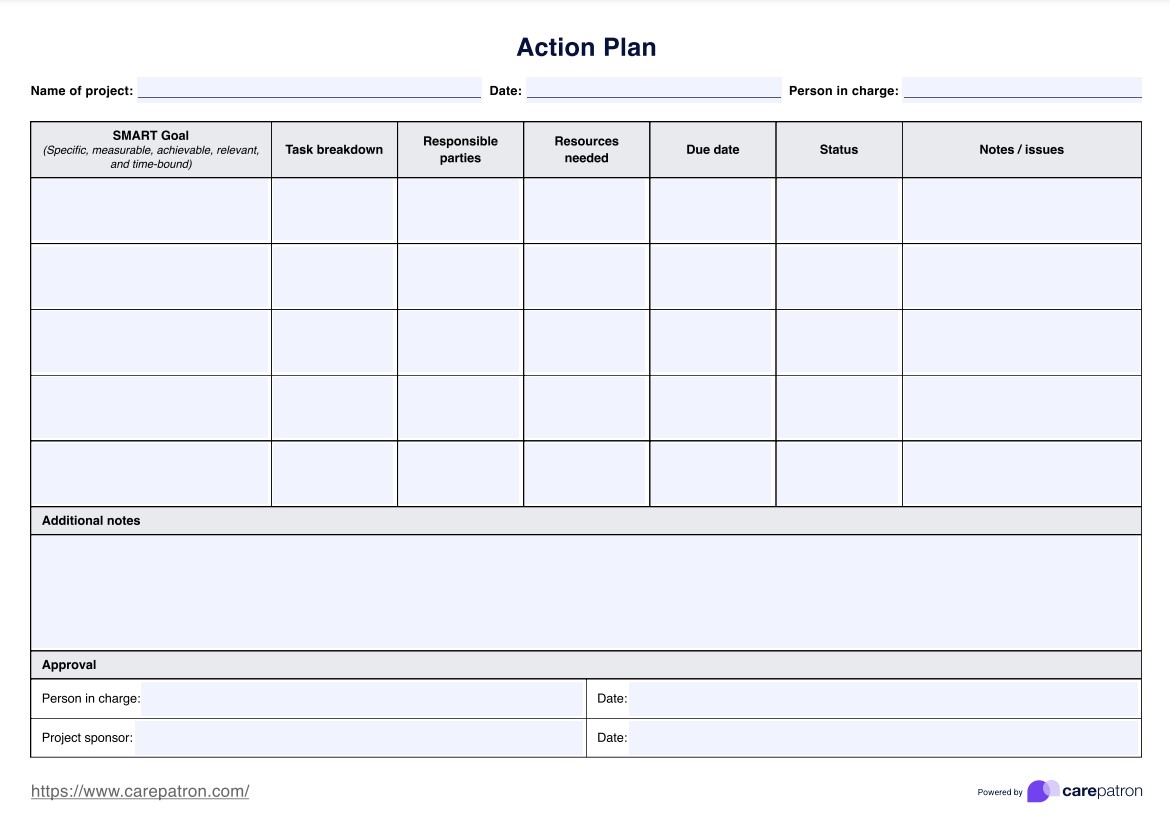
- Document the ABCDE Assessment on the ABCDE assessment template
- Discuss the patient's current condition with a senior member of the team and prepare for handover. if needed
Benefits of the ABCDE Assessment and template
There are several benefits to performing the ABCDE assessment and using our ABCDE assessment PDF template. Here are a few of them:
Quickly identify life-threatening issues
The ABCDE Assessment gives the staff a structured procedure for assessing patients that will help them identify and intervene with life-threatening issues their patients are dealing with. By providing immediate intervention, medical teams can prevent the patient's health and vitals from deteriorating further and keep the patient alive and stable to the point that the patient has a fighting chance to survive. Stabilizing a patient on the verge of death will also give medical teams a chance to do their part and treat their patient with the best care possible so they can recover.
Be thorough when stabilizing the patient
One of the great things about the ABCDE Assessment is that it has a set structure that frames how medical teams will stabilize a patient. By following the procedure, medical teams can cover all possible bases and have less chance of overlooking anything critical that may make things worse. So, not only does this assessment set a standardized procedure, but it can protect the patient from further deterioration and even death if things are done correctly.
The template can help with handing over information
Just as the assessment provides a structure for inspecting and treating patients, it also provides a structure for how things should be documented. If you download our template, you can jot down all the procedures, findings, and interventions implemented for each assessment stage. By detailing everything that has taken place, you can ensure that you will provide all the necessary information during handovers.
Commonly asked questions
That depends on the condition of the patient. You need to remember that all the procedures are done rapidly to stabilize the patient as soon as possible and maintain them in a stabilized state.
Whenever a patient is rushed to an emergency department, critical care, intensive care, or resuscitation room if they are on the verge of death because of a life-threatening illness or injury. Any of these scenarios require an ABCDE assessment to get more favorable patient outcomes.
They will address the problem. The procedure will be different depending on the problem. One ABCDE assessment example is the medical staff detects airway obstruction in unconscious patients during the Airway assessment stage. They need to clear the obstruction and then reassess the patients.