Elderly Mobility Scale
If you are treating a supposedly frail elderly patient, you can gauge them using the Elderly Mobility Scale to assess their mobility. Learn more about this scale with this guide!


What is the Elderly Mobility Scale?
The Elderly Mobility Scale (EMS) is a clinical assessment tool created to assess the physical health and mobility of patients of advanced age to see if they are at risk of accidents (specifically falling) and if they require any assistance to do certain things, specifically activities of daily living (ADLs).
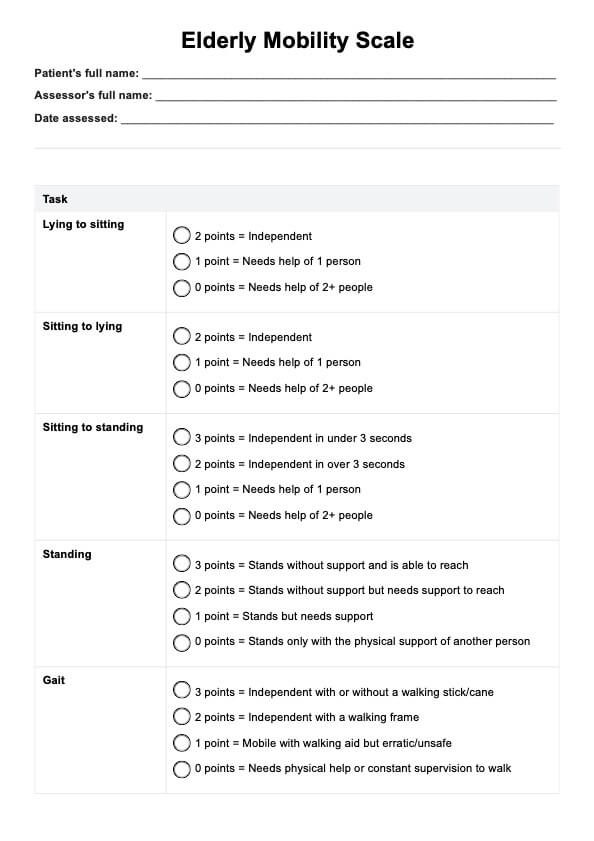
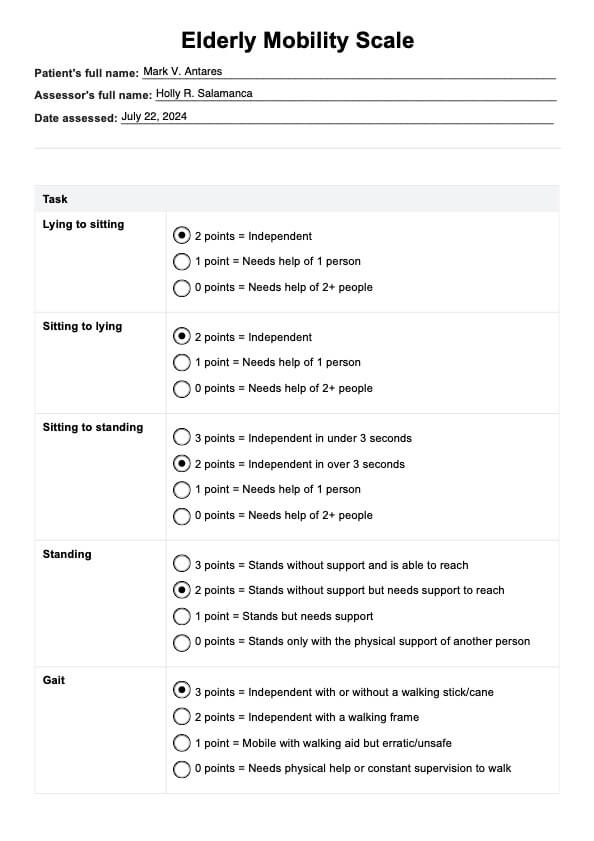
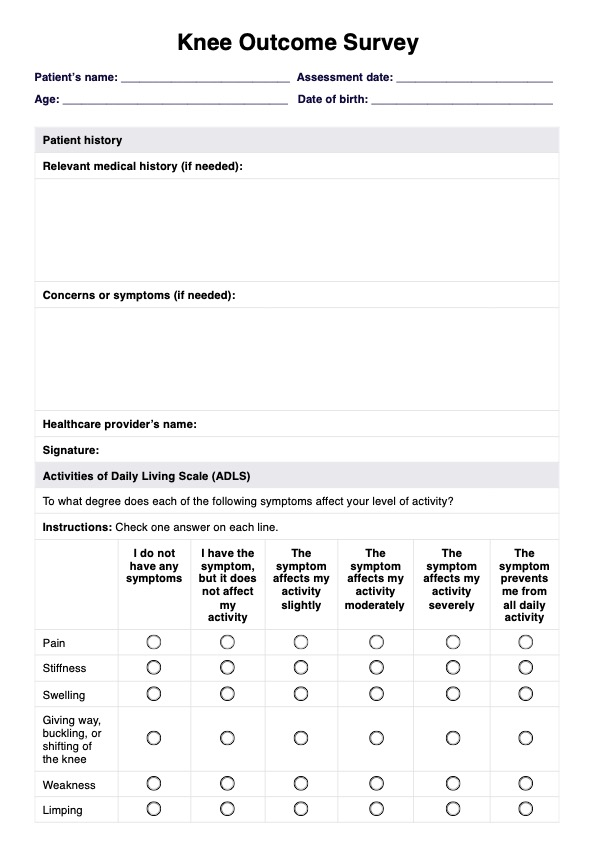
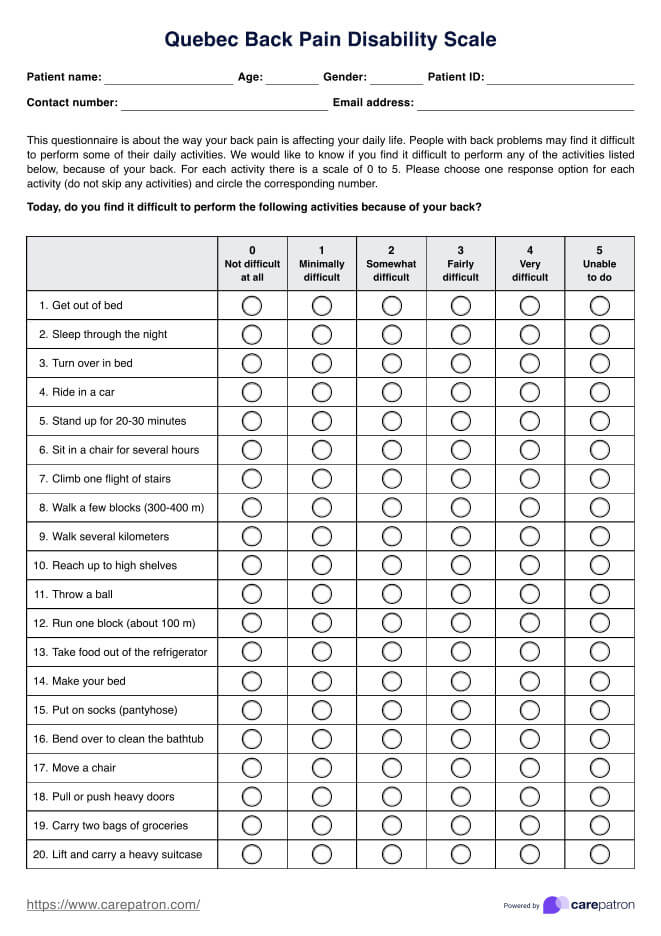
The scale is divided into seven parts, each one covering a certain activity. Here are the seven sections of the scale used for assessing mobility:
- Lying to sitting
- Sitting to lying
- Sitting to standing
- Standing
- Gait
- Timed 6-meter walk
- Functional reach
Health professionals using this scale, such as physiotherapists, occupational therapists, nurses, or geriatricians, will have to administer a few tests to observe the patient performing certain actions. The tests will be scored based on the scale’s criteria, which will be discussed in depth later.
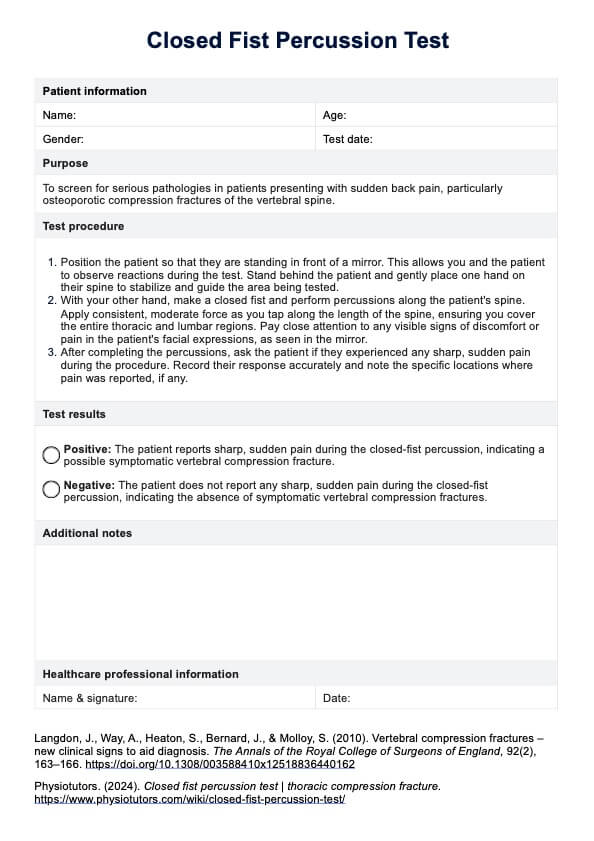
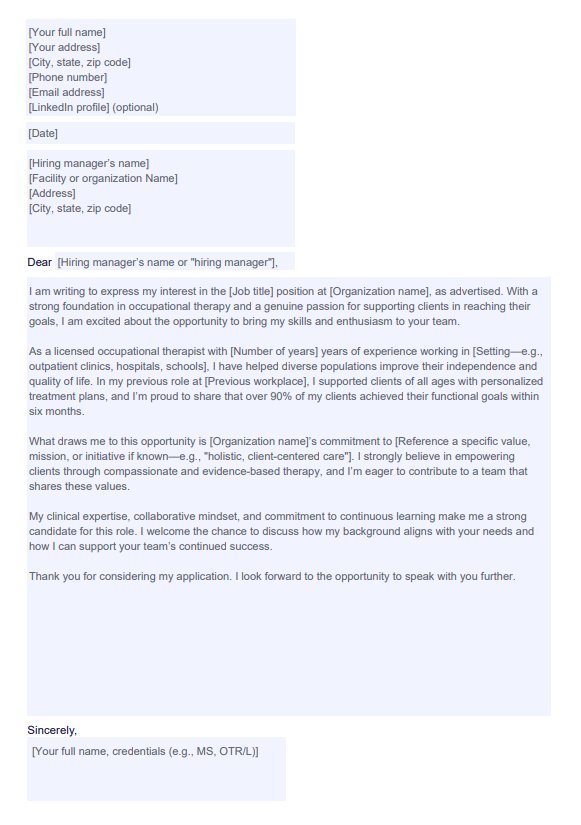
Elderly Mobility Scale Template
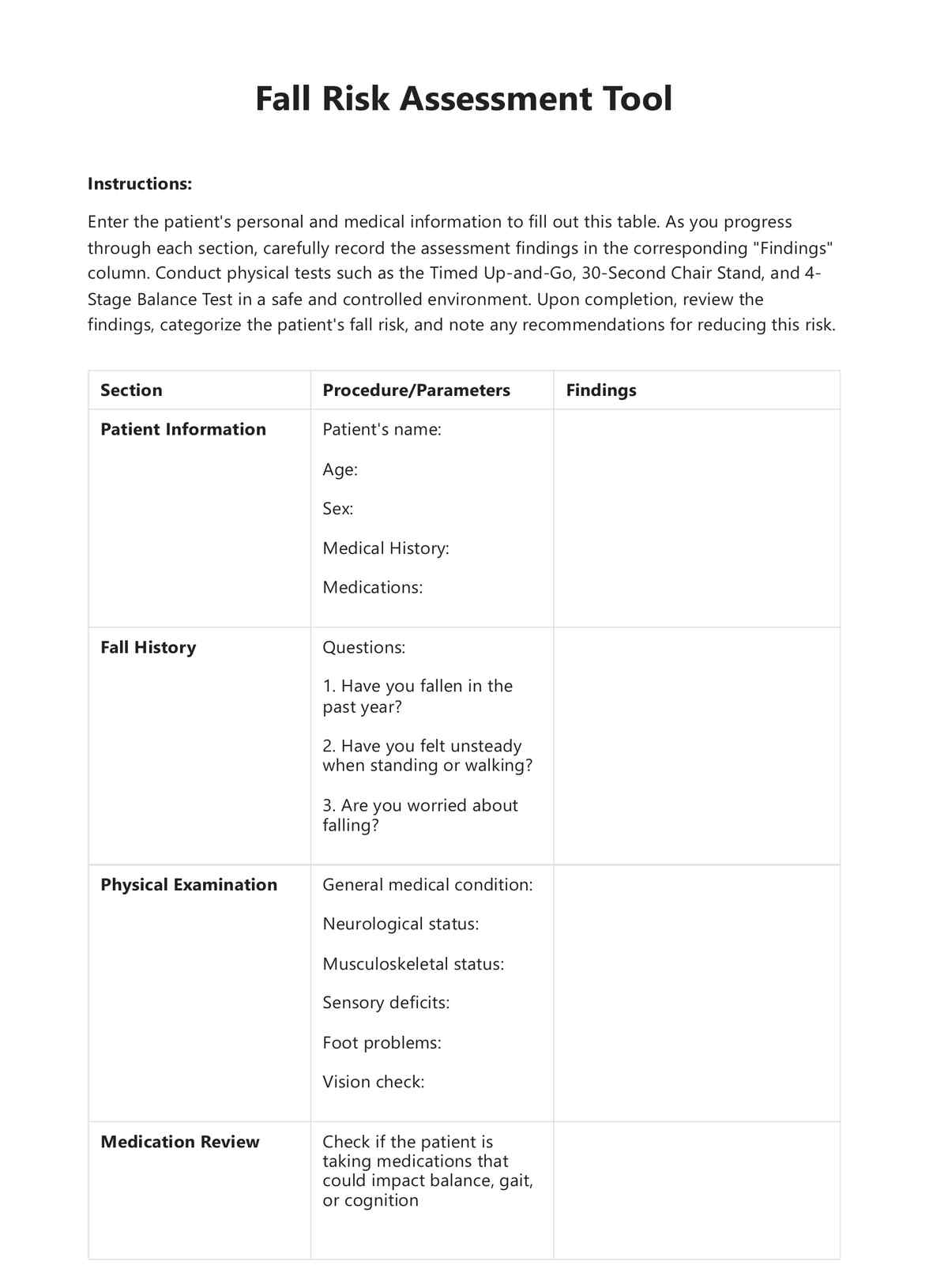
Elderly Mobility Scale Example
How to use the Elderly Mobility Scale
The Elderly Mobility Scale is easy to use. Each part has set rating options for you to select from based on observations. You need to pick the best rating. Here's an overview of the seven parts and what you need to do for each.
Before anything, make sure to prepare the following:
- A comfortable examination bed
- A chair (the patient must be able to plant both feet on the floor when seated)
- A room or big enough space with a flat surface
- Tape to mark the distance
- A yardstick to measure distance
- A stopwatch
- Assistants to help you and the patient if needed
- A copy of the Elderly Mobility Scale PDF from this guide
Once you have the above, you can conduct the tests necessary for the Elderly Mobility Scale.
Lying to sitting
- Have your patient lie down on an examination bed in a supine position with their legs straightened.
- Make them assume a sitting position (with their legs off the bed, not on).
- Make sure to assist if they need it.
Sitting to lying
- Begin with a sitting position and have them lie down again in a supine position with their legs straightened.
- Make sure to assist if they need it.
Sitting to standing
- Have your patient sit down on a chair. Make sure that the chair is high/low enough that the patient is able to sit with their back straightened and can plant both their feet on the floor.
- Have them stand up on their own or with assistance from others if needed.
- Tell them to stand up as soon as you say, “Begin.” You're going to time them using a stopwatch. When they assume a full-standing position, deactivate the stopwatch.
Standing
- Have them stand up and maintain their balance for ten to twenty seconds. They can stand with their feet together or with one foot in front of the other (with the back of their foot touching their toes).
- Make sure to ask them to reach for something or someone nearby while maintaining balance, so make sure there's a non-sharp object they can grab or a person they can extend their hand to near them.
Gait
- Have your patient walk around the area or room for two minutes. Observe how they walk.
Timed 6-meter walk
- Before anything, draw a starting line and a finish line. These lines must be 6 meters apart. Use a yardstick to measure this.
- Then, same as test #5, but this time, the patient has to follow a few instructions
- Tell them to walk in a straight line from the starting line to the finish line.
- Make sure to say “Begin” to signal them to start.
- Make sure to walk with them to prevent them from falling, if ever.
Functional reach
- Have your patient stand before a wall. They should be standing alongside the wall, with their arm close to the wall at 90 shoulder flexion, and having them close their fist.
- First, measure the starting position of your client, specifically the starting position of the third metacarpal head on the yardstick.
- Afterward, instruct your patient to reach forward as far as possible without moving their feet. Make sure to be close to them just in case they show signs of falling.
- Record their reach, a.k.a the third metacarpal head on the yardstick. When recording the reach, keep in mind that you're recording in centimeters.
Elderly Mobility Scale scoring and interpretation
The Elderly Mobility Scale has set answer choices per part, which are used to determine EMS scale scores. Here are the choices for each one and what their corresponding scores are:
Lying to sitting and sitting to lying
- Independent = 2 points
- Needs help of 1 person = 1 point
- Needs help of 2+ people = 0 points
Sitting to standing
- Independent in under 3 seconds = 3 points
- Independent in over 3 seconds = 2 points
- Needs help of 1 person = 1 point
- Needs help of 2+ people = 0 points
Standing
- Stands without support and is able to reach = 3 points
- Stands without support but needs support to reach = 2 points
- Stands but needs support = 1 point
- Stands only with the physical support of another person = 0 points
Gait
- Independent with or without a walking stick/cane = 3 points
- Independent with a walking frame = 2 points
- Mobile with walking aid but erratic/unsafe = 1 point
- Needs physical help or constant supervision to walk = 0 points
Timed 6-meter walk
- Was able to finish under 15 seconds = 3 points
- Was able to finish between 16 – 30 seconds = 2 points
- Took over 30 seconds to finish = 1 point
- Unable to cover 6 meters = 0 points
Functional reach
- Their reach is over 20 cm. = 4 points
- Their reach is between 10 - 20 cm. = 2 points
- Their reach is under 10 cm. = 0 points
After getting all scores, calculate the sum, then refer to the result interpretation per score provided below:
Scores of 0-9
A score of 0-9 means that the patient depends on mobility maneuvers. They require help/support for basic activities of daily living.
Scores of 10-13
Having a score of 10-13 means that the patient is borderline in terms of safe mobility and independence when it comes to activities of daily living, but they still require help with some mobility maneuvers.
Scores of 14+
Having a score of more than 14 means that the patient can perform mobility maneuvers alone and safely, plus, they are independent when it comes to basic activities of daily living.
When is it best to use the Elderly Mobility Scale?
The tests involved in the scale will give the healthcare professional a good picture of the elderly patient’s functional status, physical health, and mobility. The results of these tests can help guide treatment decisions and plans that will hopefully improve the patient’s functional mobility or at least help them cope, live, and accept their new reality if the decline in their mobility can’t be reversed.
If an older person is scheduled for an appointment with you because they want to be checked for mobility disabilities or deterioration, healthcare professionals often conduct comprehensive evaluations of a patient, including various tests such as this one, which is perfect for assessing if they have an array of potential problems they are dealing with or are at risk of developing.
What are the benefits of the Elderly Mobility Scale?
There are numerous benefits to including the Elderly Mobility Scale in the comprehensive tests you will conduct on your patient. Here are a few of them:
- Identify the risk of falling: By having your patients perform the activities, you can observe if they show signs that could indicate them being at risk of falling.
- Identify other potentially related mobility problems: Besides falling, the scale can also assess whether the patient is dealing with other possible mobility-related nerve and muscle function problems or if they risk developing them. This will become evident when they do activities tied to this scale, like simply changing positions from Lying to Sitting and vice versa.
- Help develop appropriate care plans: The patient's final score and observations of them while they did the activities tied to the scale should serve you well when it comes to developing a tailor-fitted care plan for them. This plan may include exercises for improving mobility, a diet to better care for their bone health, or a plan to bring the patient to an assisted living facility.
- Used as a monitoring tool: You can use this scale again for patients who follow your implemented treatment plan, especially if they visit you for a routine check-up. It can be a monitoring tool to determine if your treatment plan is effective or needs tweaking based on their progress.
Commonly asked questions
That depends. This scale comes with several activities that need to be done to score the patient, so it may take 15 minutes to an hour.
Yes. These activities involve a person’s mobility, and since the primary population for this scale is elderly people, they are at risk of losing their balance. That’s why you and your assistants should help support these patients while performing the activities so they don’t get hurt.
Of course, if you ever conduct a house call, you can definitely administer this in a home setting, so long as you have the needed equipment.
Studies have demonstrated high inter-rater reliability in measurements, suggesting that scores determined by different physiotherapists or researchers are comparable, thus reinforcing the credibility of the assessment tools discussed. Additionally, studies have shown that the scale has demonstrated concurrent validity, showing a significant correlation between EMS scores and the Functional Independence Measure, indicating that EMS effectively relates to established clinical instruments for evaluating daily living activities and mobility in acute hospital settings.