Falls Efficacy Scale
Use the Falls Efficacy Scale to gauge how afraid your patient is of falling while doing activities of daily living.


What is the fear of falling?
The also known as Basophobia, is a specific fear characterized by an intense and sometimes irrational dread of falling. Whether it's descending a flight of stairs, being at a great height, or even plummeting from the sky, this fear encompasses more than just the act of falling itself. It extends to the fear of losing balance and the inability to regain stability. Those afflicted by this fear often experience panic or anxiety when in elevated or precarious locations, with even the simple act of ascending a staircase causing distress.
The response to this fear varies depending on its severity. Some individuals may feel uneasy or experience mild discomfort, while others may actively avoid certain places due to their overwhelming fear of falling and losing balance. Remarkably, this fear can harm a person's life. It can limit employment opportunities, particularly those involving tall buildings, and hinder travel experiences by restricting visits to certain locations or participation in specific activities.
Moreover, this fear can significantly impact an individual's ability to carry out everyday tasks, particularly in older individuals. In this guide, we will delve into the challenges posed by this fear and explore potential solutions.
Here is another resource that assesses the risk of falling in patients:
Falls Efficacy Scale Template
Falls Efficacy Scale Example
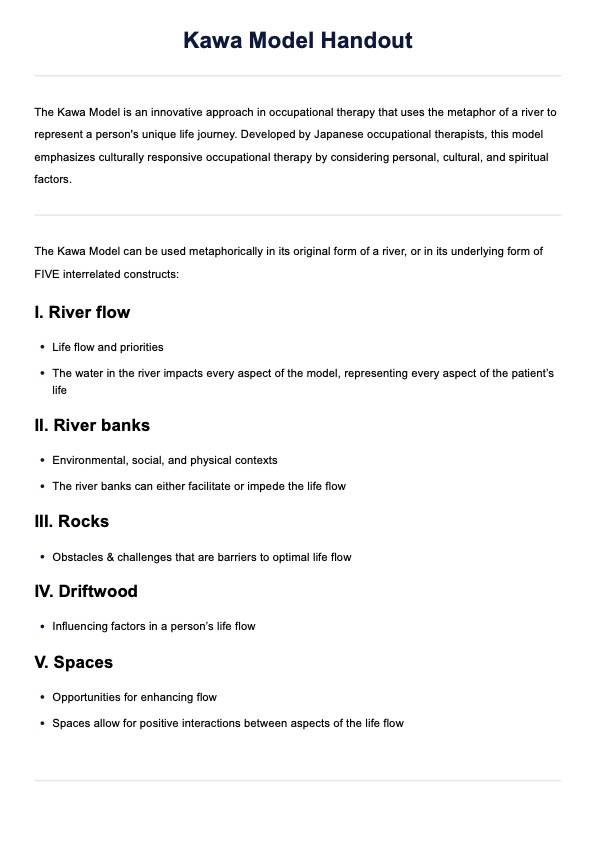
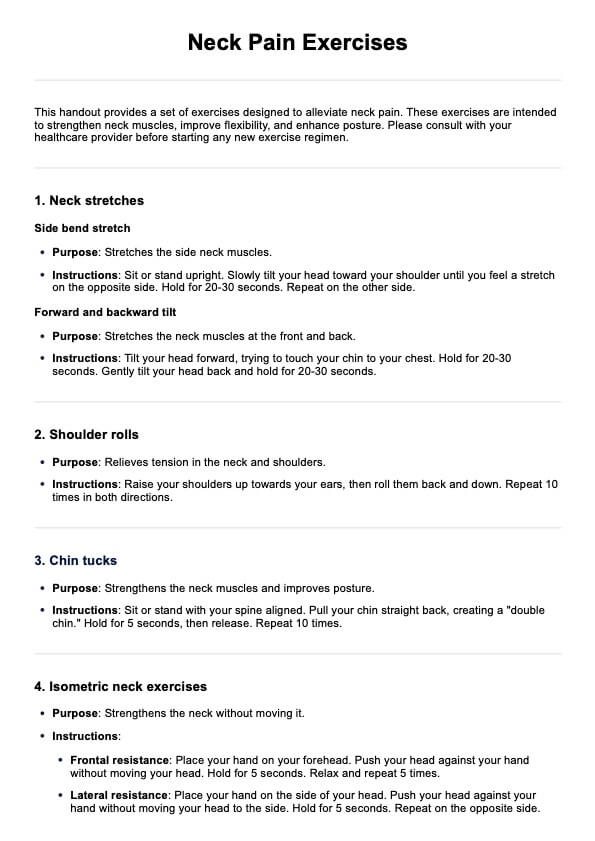
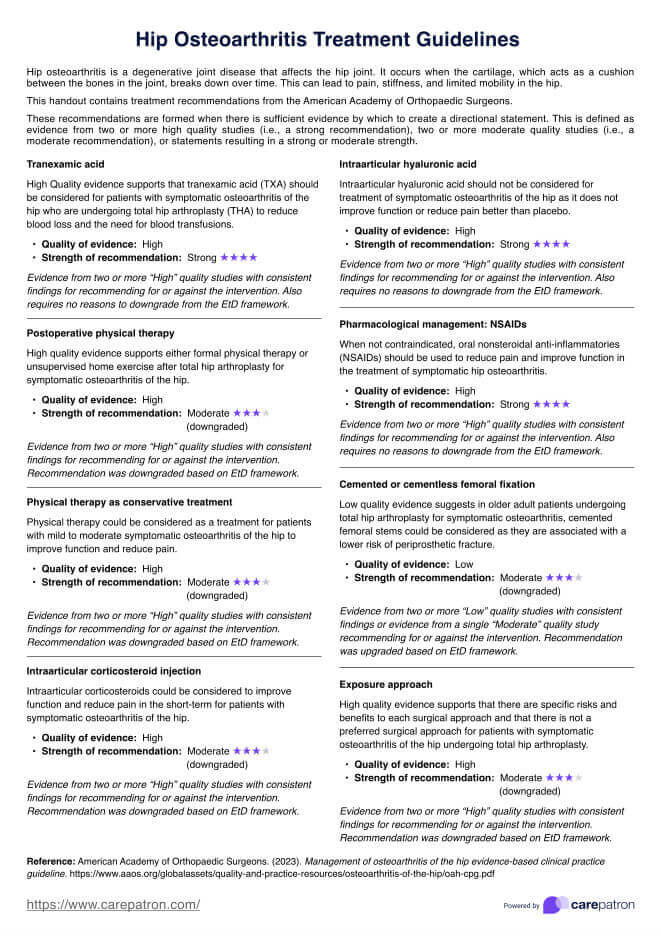
How to use the Falls Efficacy Scale:
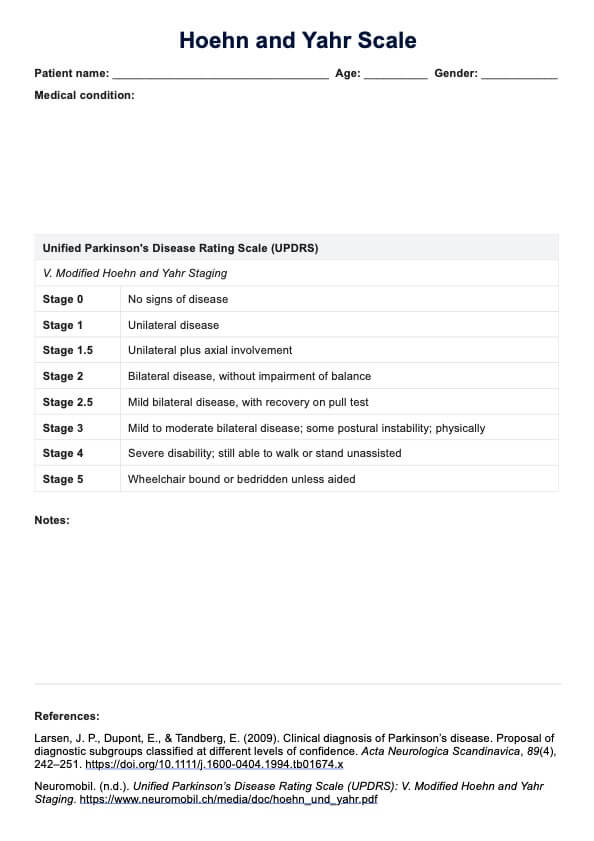
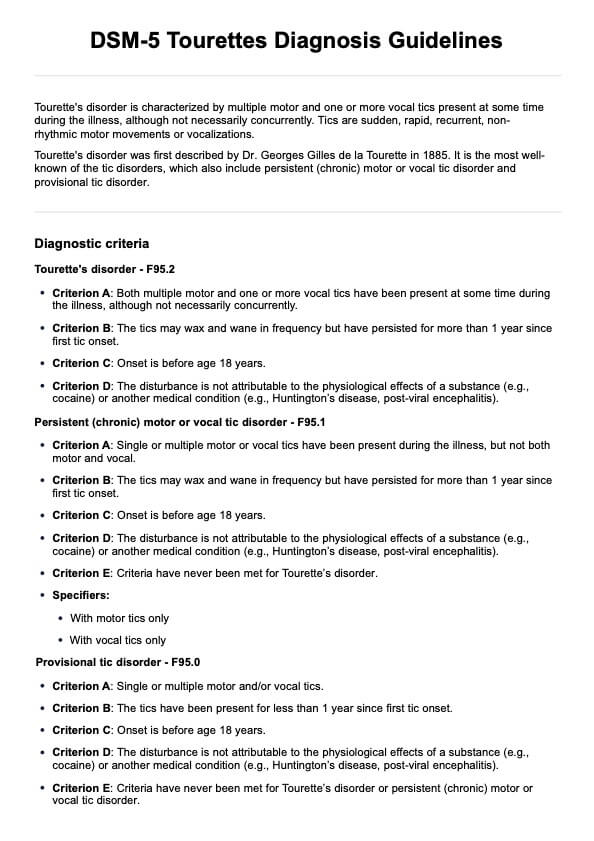
The Falls Efficacy Scale is a nifty clinical tool used to assess a patient's fear of falling. It is often used to gauge elderly patients, patients who have fallen before and have been dealing with problems that were caused by their fall, and patients dealing with neurological conditions such as stroke and Parkinson's Disease.
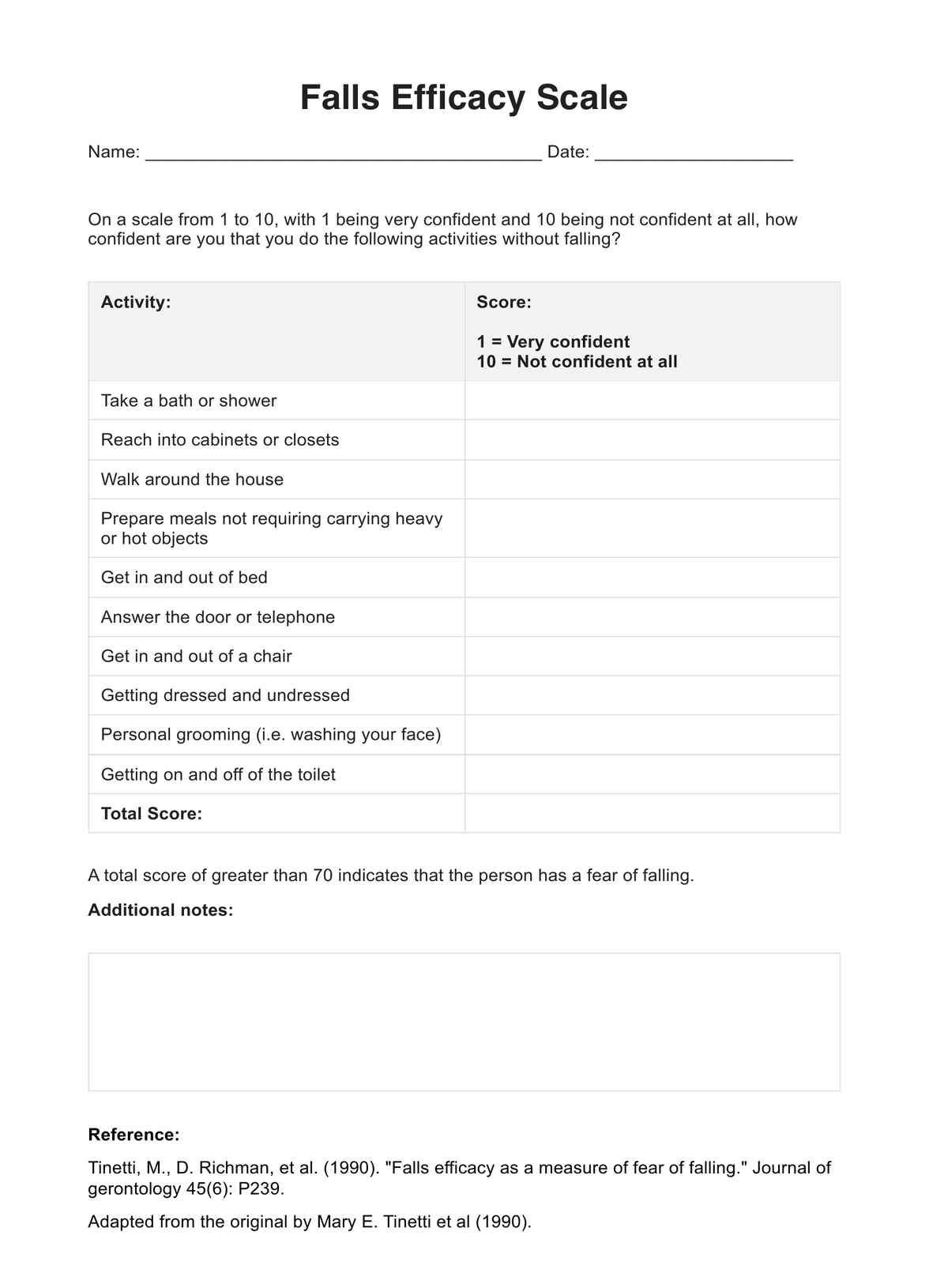
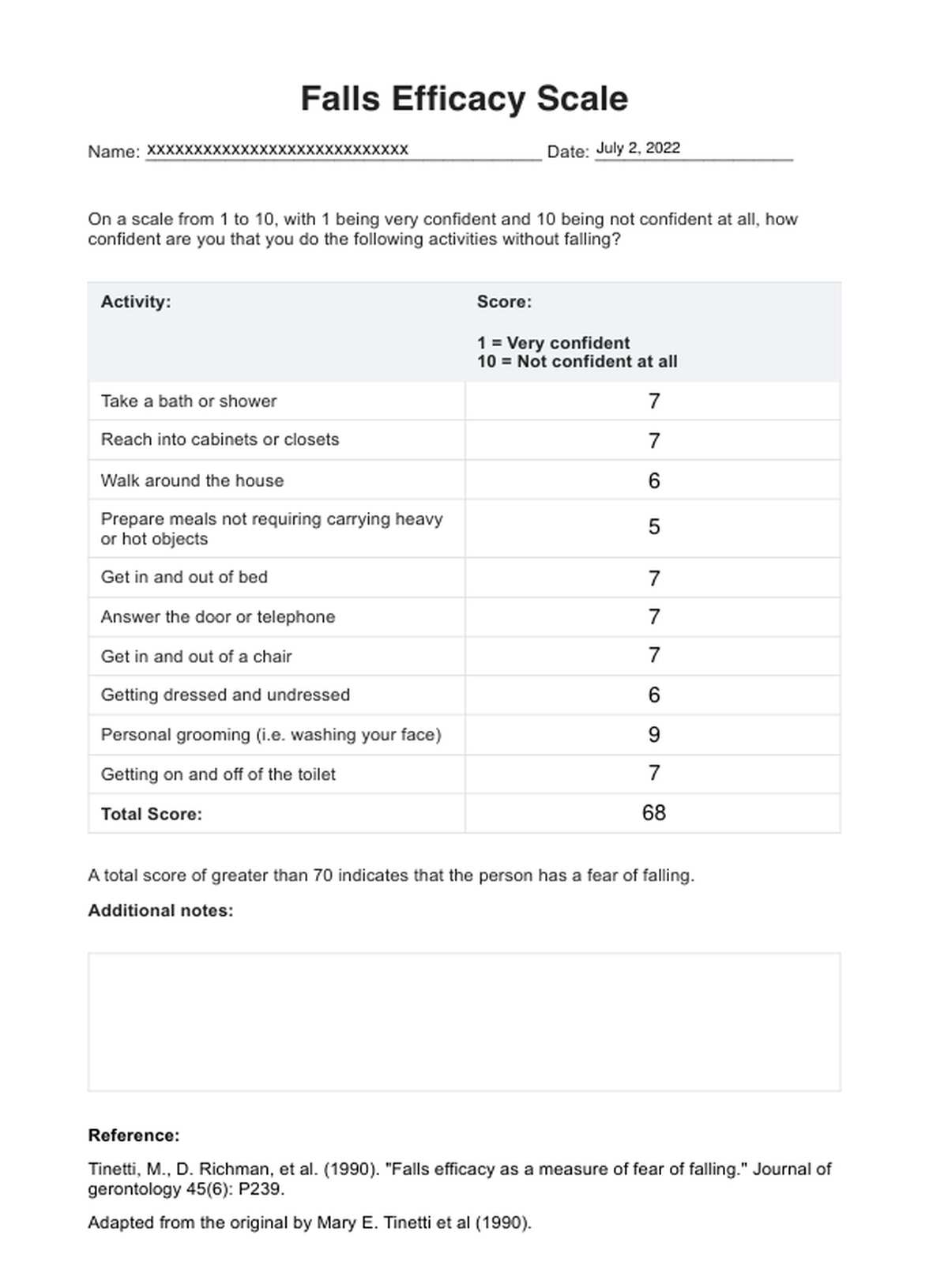
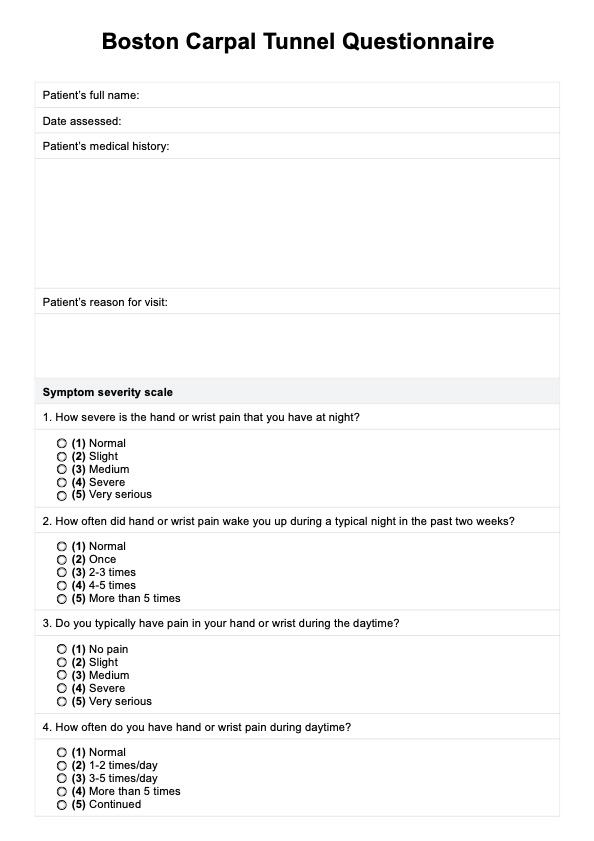
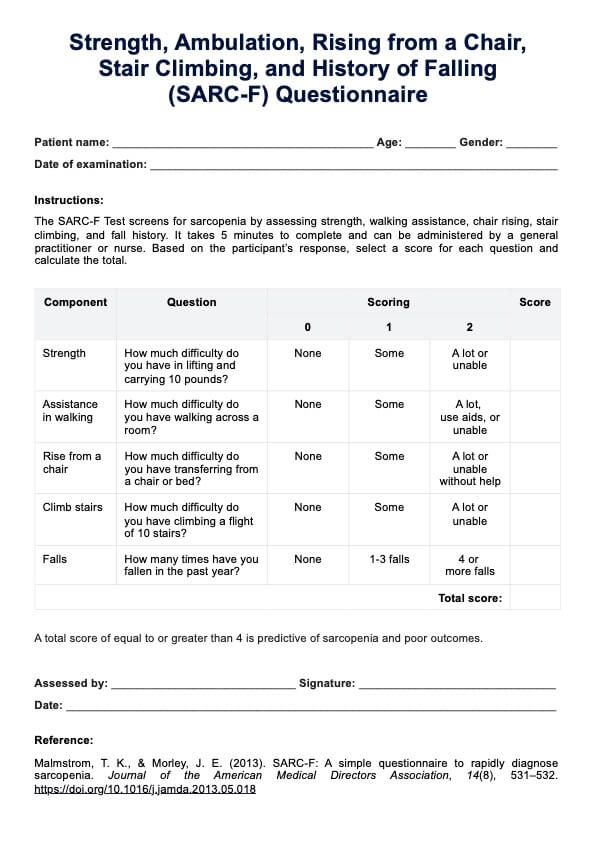
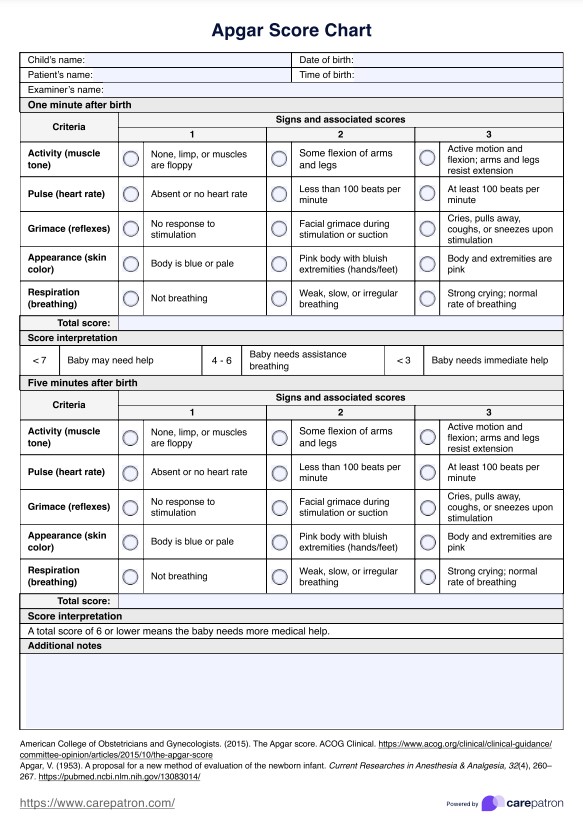
There are different variations of the Falls Efficacy Scale. The one we will discuss and show you is the Tinetti version, which focuses on activities of daily living. These include the following:
- Taking a bath or shower
- Reaching into cabinets or closets
- Walking around the house
- Preparing meals that don't require carrying heavy or hot objects
- Getting in and out of bed
- Answering the door or telephone
- Getting in and out of a chair
- Getting dressed and undressed
- Personal grooming
- Getting on and off of the toilet
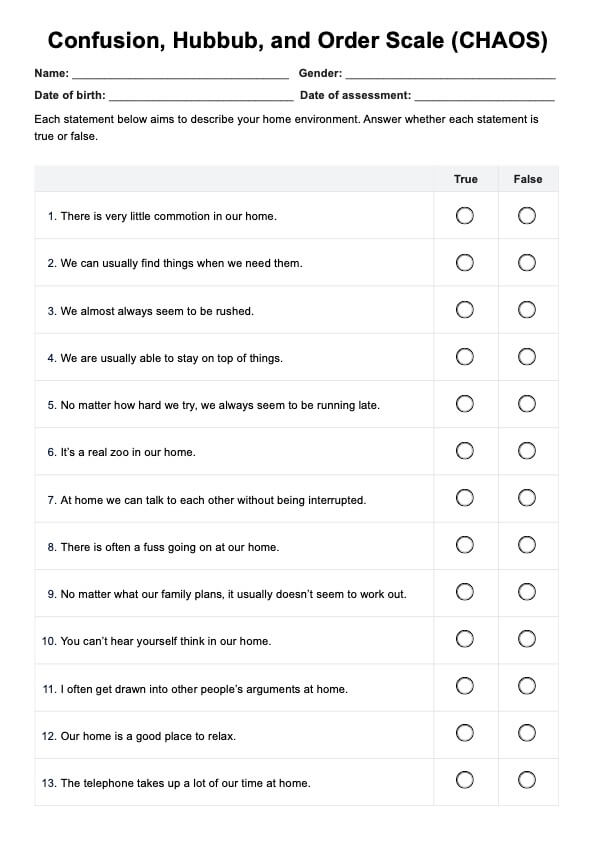
Patients simply need to rate themselves on a scale of 1 to 10, reflecting their confidence in performing daily activities without the risk of falling. A rating of 1 indicates utmost balance confidence, whereas 10 signifies a lack of confidence. The total score can range from 10 to 100 with just ten items to assess. A patient scoring 71 or above suggests a fear of falling.
When is it best to use the Falls Efficacy Scale?
The Falls Efficacy Scale primarily targets elderly patients, community-living older adults, individuals with a history of fall-related injuries, those whose mobility and capacity to engage in ambulatory activities have been affected, those with Chronic Obstructive Pulmonary Disease, Osteoarthritis, and those with neurological conditions. These patients are likely to have experienced a decline in mobility and limitations in performing daily activities and pursuits they enjoy.
When evaluating these patients, assessing their fear of falling is crucial. It is recommended to provide them with a clear explanation of the purpose and significance of this scale before conducting the assessment. Additionally, it is important to use this scale in conjunction with other assessments to develop a comprehensive and personalized treatment plan. This entails incorporating other clinical tools that evaluate both the fear and risk of falling.
Also, note that this scale is not intended for individuals who fear falling unrelated to any underlying medical conditions. In such cases, it would be more beneficial to guide them toward therapy options like Cognitive Behavioral Therapy, which can assist in reframing their thoughts and addressing their fear.
What are the benefits of using the Falls Efficacy Scale?
The Falls Efficacy Scale can identify areas of concern.
The Falls Efficacy Scale aims to gauge the confidence of a person to perform certain activities of daily living without losing their balance and falling. By looking at the self-ratings that patients write on the scale sheet, professionals can identify specific areas of concern that they need to address.
The Falls Efficacy Scale can help professionals develop personalized treatment plans.
Professionals can have their patients expound on their self-ratings so that they can understand their situation better. Numbers can only do so much, but expounded explanations can work wonders for the healthcare professionals handling them. By knowing the patient's situation, they can use the results of the scale and other assessments to create personalized treatment plans for their patients that focus on addressing key identified issues.
The Falls Efficacy Scale used to monitor patients down the line.
The Falls Efficacy Scale doesn't have to be used during a comprehensive assessment process. The scale can be used again, especially down the line after a treatment plan's developed and implemented. To check on the patient's status, a healthcare professional can schedule a routine checkup to assess if the patient is improving and has regained confidence to do certain activities of daily living without losing balance or falling.
If their self-ratings result in a lower score, they are more confident in their ability to perform ADLs. This means that your treatment plan is working. If the score becomes higher, make adjustments to your treatment plan and see if your changes will do the trick. Just make sure that your treatment plan considers the safety of your patients.
What else should I do after getting Falls Efficacy Scale results?
It's not enough to assess fear in patients, especially if they've had a history of injurious falls and if they're dealing with mobility issues as a result of aging, injuries, or ailments like multiple sclerosis. It would be best to conduct assessments that specifically assess their balance control.
Examples of such assessments that you can conduct are the following:
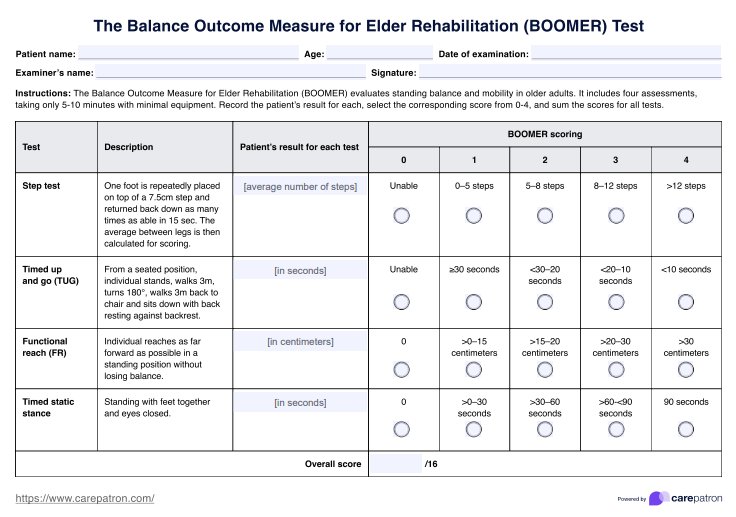
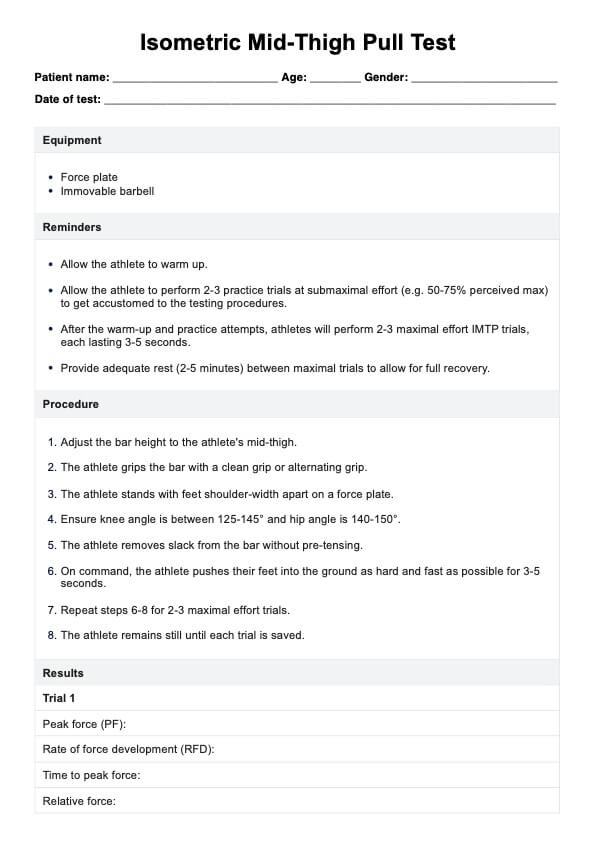
- Timed Up & Go Test
- Dynamic Gait Index
- 4-Stage Balance Test
- Berg Balance Scale
- Y-Balance Test
- Romberg Test
- Four-square Step Test
- Balance Evaluation Systems Test
The target populations of these tests are mostly community-dwelling older people, people with mobility issues, people with fall history, and those who are dealing with limited physical functioning as a result of neurological conditions.
These assessments can assess the risk of falling and functional ability of a person through exercises like standing in different stances, a functional reach test, standing up or sitting down without support, and walking back and forth for a certain distance and time. For assessments that are scored, lower scores indicate an increased risk of future falls, while higher scores indicate independence and having the capability to maintain their balance with minimal support and without much problem.
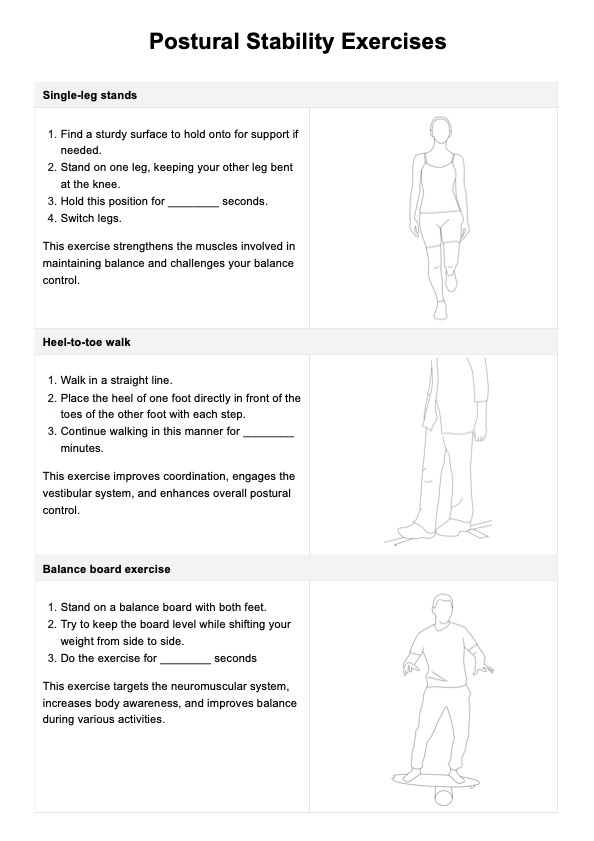
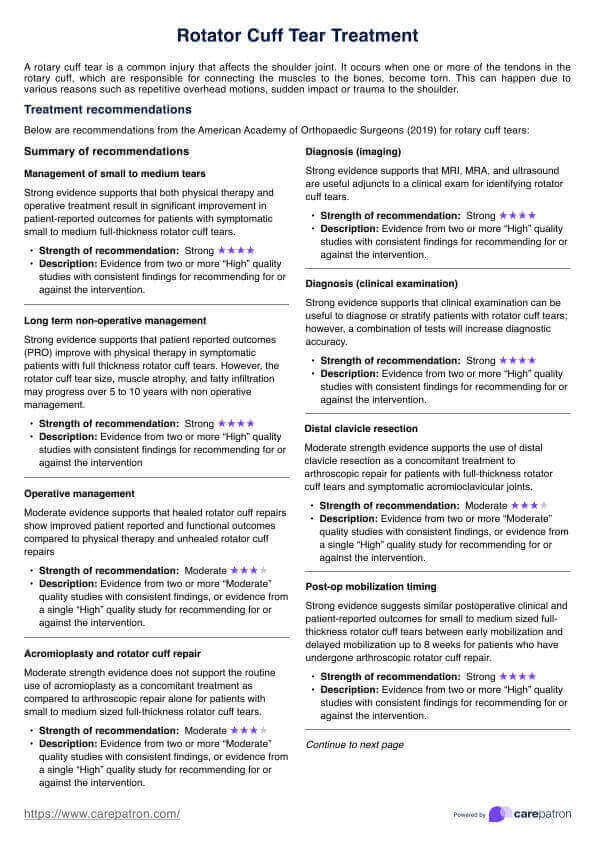
For those who have a high risk of falling based on test results, it would be best to develop a treatment plan that seeks to boost their physical strength by having them participate in physical activity as part of rehabilitation and physical therapy so they can develop more confidence when it comes to balancing themselves, and more importantly, to make them strong enough to ensure they are able to balance themselves while performing activities like preparing simple meals or reaching for things.
Strengthening the patients through rehabilitation and physical therapy can improve their confidence. If they keep fearing falls, it can lead to mental health problems and impact their quality of life because they might become unwilling to do certain things that might give them joy if those things even have the slightest risk of falling. Rehabilitation and physical therapy can improve their physical function, which is helpful when it comes to increasing fall prevention.
For those who have a high risk of falling because of cognitive impairment or other neurological problems, plans can be created that take into account the patient requiring support. Plans for falls prevention can be made so they can avoid being in situations or places where they can fall, like walking on an uneven surface, slippery surface, or a poorly-maintained pavement.
What's great about tests like the Berg Balance Scale is that they have excellent test-retest reliability and excellent internal consistency. This means you can conduct the same assessments from time to time to see if there are any improvements in the patient in terms of their balance confidence and capabilities.
Commonly asked questions
It can be accomplished within five minutes.
You can conduct the scale in an interview format. Just explain what they need to do, then have them say what their self-ratings are. You can jot them down on the sheet. If you conduct it like an interview, you can have them expound on their self-ratings and record them in the comments box.
Geriatricians, physical therapists, neurologists, and adjacent healthcare professionals can use this scale.