Cervical Torsion Test
Learn how to perform the Cervical Torsion Test. Get a free PDF template to streamline your documentation today!


What is cervicogenic dizziness?
Cervicogenic dizziness is a condition characterized by dizziness or vertigo originating from neck issues, particularly those involving the cervical spine. This type of dizziness is typically associated with neck pain and can be triggered or worsened by neck movements. The exact mechanism is not fully understood, but it involves dysfunctional sensory inputs from the cervical spine to the central nervous system, which disrupts the body's normal balance and orientation systems.
Causes and symptoms
The causes of cervicogenic dizziness often relate to disorders of the neck, which can arise from whiplash, cervical spine degeneration, or other neck injuries that affect the joints, muscles, or nerves of the cervical spine. Symptoms usually include a spinning sensation or imbalance exacerbated by moving the neck. This dizziness often accompanies other neck-related symptoms, such as limited range of motion, neck pain, and sometimes headaches.
Comparing Cervical Torsion Test and BPPV diagnosis
The Cervical Torsion Test is essential for diagnosing cervicogenic dizziness by isolating the cervical spine's movement to see if it induces symptoms. This contrasts with diagnosing benign paroxysmal positional vertigo (BPPV), which involves the Dix-Hallpike maneuver. BPPV is characterized by brief episodes of dizziness caused by head position changes, linked to displaced crystals within the inner ear. While the Cervical Torsion Test evaluates the neck's role in dizziness by observing symptoms upon neck movement, BPPV testing specifically looks for dizziness triggered by particular head movements, helping to distinguish between the two conditions based on the origin and trigger of the symptoms.
How to diagnose cervicogenic dizziness
Diagnosing cervicogenic dizziness involves a detailed assessment to rule out other causes of dizziness and vertigo. The diagnostic process includes a thorough medical history, physical examination, and possibly imaging studies like MRI or X-rays if a cervical spine pathology is suspected. One specific test used in the diagnosis is the Cervical Torsion Test, which evaluates the contribution of the cervical spine to the dizziness experienced by the patient.
Cervical Torsion Test Template
Cervical Torsion Test Example
What is the Cervical Torsion Test?
The clinical Cervical Torsion Test is a clinical diagnosis tool used to identify cervicogenic dizziness, which stems from neck issues.
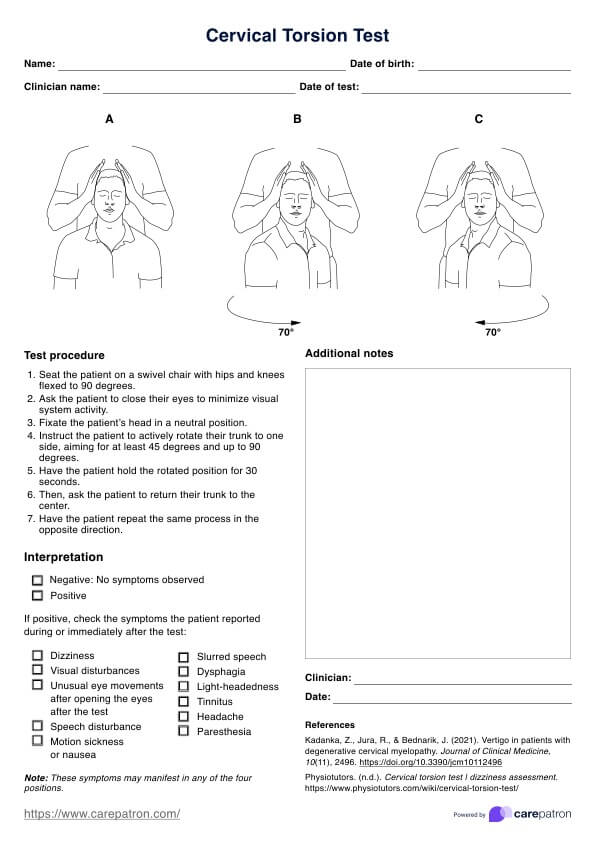
Durin the test, the examiner asks the patient to sit on a swivel chair with their hips and knees flexed at 90 degrees. The patient is then instructed to close their eyes in order to reduce visual system activity. Next, the examiner stabilizes the patient's head in a neutral position and asks them to actively rotate their trunk to one side, aiming for a minimum of 45 degrees and up to 90 degrees. After holding the rotated position for 30 seconds, the patient returns their trunk back to center before repeating the same process on the opposite side.
The test is considered positive if the patient's dizziness symptoms are reproduced or exacerbated by the head's rotation. This outcome suggests that the cervical spine may be the source of the dizziness, helping differentiate cervicogenic dizziness from other types, such as vestibular or inner ear-related dizziness.
How to use our Cervical Torsion Test template
The Cervical Torsion Test is a valuable diagnostic tool for evaluating the cervical spine's mobility and pain response. This is not to be mistaken for the Head-Neck Differentiation Test. To ensure consistent and reliable results, follow these streamlined steps along with the provided template:
Step 1: Prepare the template and gather patient information
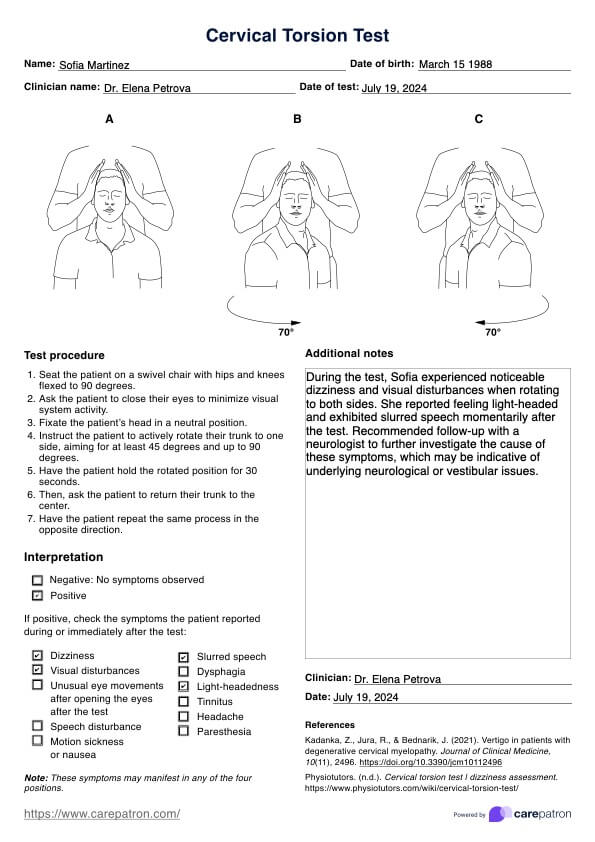
Download and print the Cervical Torsion Test template. Then, fill in the patient's details, including name, date of birth, date of the test, and the clinician's name.
Step 2: Explain the procedure to the patient
Before beginning the test, clearly explain the procedure to the patient. This helps minimize anxiety and ensures the patient remains relaxed, which is crucial for accurate results.
Step 3: Conduct the test
Position the patient comfortably with their head in a neutral position. Use the instructions on the template to perform the test.
Step 4: Record the results
Document the result by picking between positive and negative in the Interpretation section. If the test is positive, select the symptoms that the patient reported. Use the Additional notes section to better explain your findings.
What are the next steps?
After conducting the cervical torsion test and interpreting the results suggested clinical tests, the following steps are recommended:
Step 1: Perform additional tests
Further diagnostic tests should be considered to confirm the diagnosis or rule out other potential issues. These clinical tests might include imaging studies like MRI or CT scans, which provide detailed views of the cervical spine structures. Other functional tests may also be conducted to assess nerve function and spinal health.
Step 2: Consultation with specialists
Consultation with a neurologist or an orthopedic specialist may be necessary, depending on the results. These specialists can offer more advanced management strategies for cervical spine disorders.
Step 3: Plan treatment options
Treatment may include physical therapy, medication for pain and inflammation, or in some cases, surgical interventions. Physical therapy techniques could involve exercises to improve neck strength and flexibility, postural correction, and manual therapy.
Benefits of using our template
Using a Cervical Torsion Test template in clinical practice offers numerous advantages for both healthcare providers and patients. This template standardizes the assessment process, ensuring consistency and accuracy in diagnosing clinical Cervical Torsion Test and spine issues. Here are some key benefits:
- Improved diagnostic accuracy: The Cervical Torsion Test template provides a structured approach to assessing the cervical spine's range of motion and pain response. By standardizing the evaluation, clinicians can more accurately identify issues related to cervical vertebrae and muscle function, leading to more precise diagnoses.
- Enhanced patient management: Healthcare providers can track patient progress over time with a clear and consistent testing format. This is particularly useful for monitoring the effectiveness of treatments and making informed decisions about changes to therapy or interventions.
- Efficient clinical workflow: Using a template streamlines the assessment process, saving time and reducing potential errors. This efficiency allows clinicians to focus more on patient interaction and less on testing mechanics.
Treatment of cervicogenic dizziness
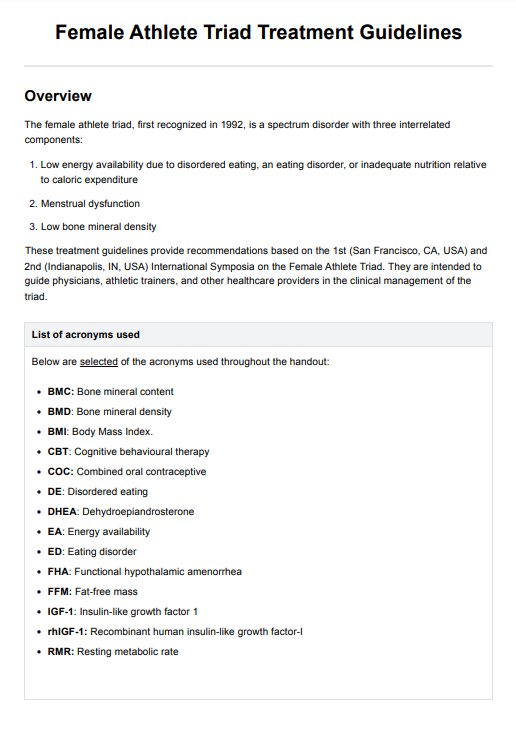
Treating cervicogenic dizziness involves addressing the underlying neck issues contributing to the condition. A multidisciplinary approach is often most effective, incorporating physical therapy, medication, and sometimes manual therapies. Here’s a breakdown of the typical treatment modalities:
Physical therapy
Physical therapy is central to treating cervicogenic dizziness. Therapists use specific exercises to improve neck posture, strengthen neck muscles, and enhance the range of eye movement control and motion. Techniques such as cervical spine mobilization and stabilization exercises can help reduce symptoms by restoring proper function and reducing strain on the cervical spine.
Manual therapy
Chiropractic care or osteopathy may include manual adjustments and manipulations of the neck to reduce joint restrictions or misalignments in the cervical spine. These techniques aim to enhance joint mobility and alleviate the stress on cervical soft tissues, thereby reducing dizziness.
Vestibular rehabilitation
Although vestibular rehabilitation exercises are primarily used for vestibular dysfunction and causes of dizziness, they can also benefit those with cervicogenic dizziness. These exercises help retrain the brain to compensate for changes in the balance system, often improving symptoms when combined with treatments that target neck disorders.
Medications
While medication is not a primary treatment for cervicogenic dizziness, it can be used to manage symptoms. Pain relievers and anti-inflammatory drugs can help alleviate neck pain and inflammation that may contribute to dizziness. In some cases, muscle relaxants are also prescribed to reduce muscle tension in the cervical region.
Lifestyle adjustments
Modifying daily activities to avoid movements that exacerbate symptoms is often recommended. Patients may be advised on ergonomic changes, especially regarding workstations and sleeping positions, to support proper neck alignment and reduce strain.
Interventional treatments
In cases where conventional therapies do not relieve symptoms, more interventional approaches may be considered. This includes pain relief injections or surgical interventions if significant structural abnormalities are identified.
Commonly asked questions
The most common cause of cervicogenic dizziness is a dysfunction in the cervical spine, which may stem from whiplash, cervical spondylosis, or other forms of neck injury or disorder that affect the joints, muscles, or nerves.
The cervical neck torsion test for cervicogenic dizziness involves the examiner passively rotating the patient's head to full range. In contrast, the patient is seated upright to determine if this movement provokes dizziness, indicating a cervical origin of the symptoms.
The duration for cervical vertigo to resolve can vary widely; it might take a few weeks to several months, depending on the underlying cause, the effectiveness of the treatment, and the patient's adherence to a rehabilitation program.