To write effective physical therapy notes, organize your documentation in a structured format that captures all relevant information. Use clear, concise language, avoiding jargon to facilitate understanding among healthcare providers. Finally, ensure accuracy and timeliness in your notes, adhering to professional standards and maintaining patient confidentiality.
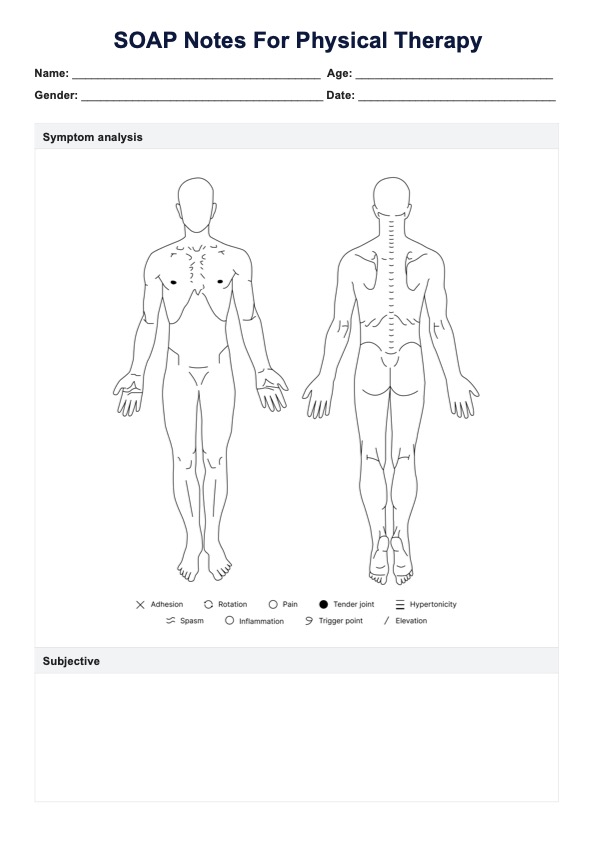
SOAP Notes For Physical Therapy Template
An intuitive SOAP note template for physical therapists will help your practice improve its documentation, all while saving valuable time.
SOAP Notes For Physical Therapy Template Template
Commonly asked questions
While this depends on the type of physical therapy session that you have had with your patient, a good rule of thumb is around 1-2 pages. SOAP notes should be clear and concise, and you should try not to repeat yourself or use overly wordy sentences.
Because SOAP notes are legal documents, you must ensure that everything you include is appropriate and professional. Any observations you make about a patient's behavior or affect need to be supported by evidence. You should also avoid any kind of judgemental or offensive language and keep abbreviations to a minimum.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











