Effective SOAP notes in occupational therapy should be concise, objective, and focused on the patient's progress and functional outcomes. The note should clearly document the patient's subjective report, the occupational therapist's objective observations, the therapist's clinical assessment, and the plan for ongoing treatment.
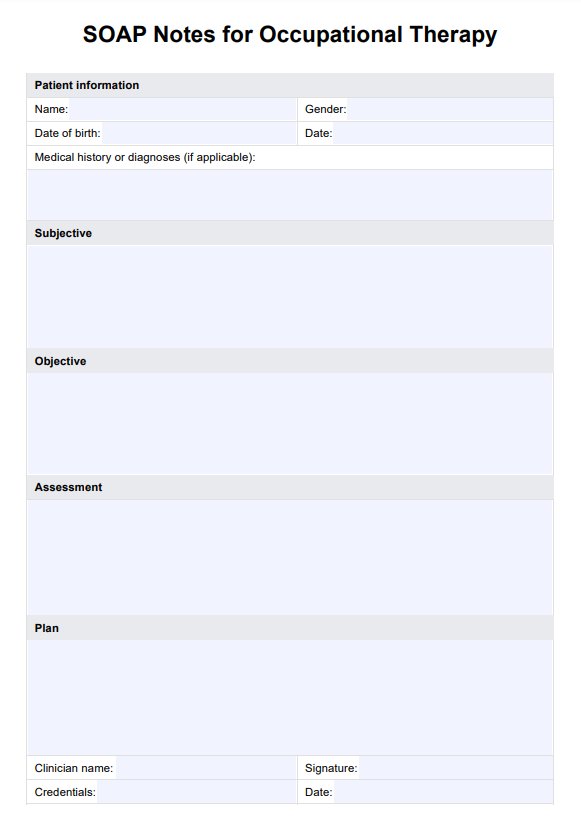
SOAP Notes For Occupational Therapy Template
Download our template for occupational therapy SOAP notes to improve your clinical documentation process.
SOAP Notes For Occupational Therapy Template Template
Commonly asked questions
Using SOAP notes in occupational therapy can help improve communication among healthcare providers, enhance patient care, and facilitate information sharing. They also provide a structured format for documenting patient progress and treatment outcomes, which can help with billing and reimbursement.
A SOAP note in occupational therapy typically includes the following components: Subjective (patient's report), Objective (therapist's observations), Assessment (therapist's clinical assessment), and Plan (plan for ongoing treatment).
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments