Physical Mobility Scale
Learn about the Physical Mobility Scale and use our template to assess older adults and their ability to perform certain movements!


What is the Physical Mobility Scale?
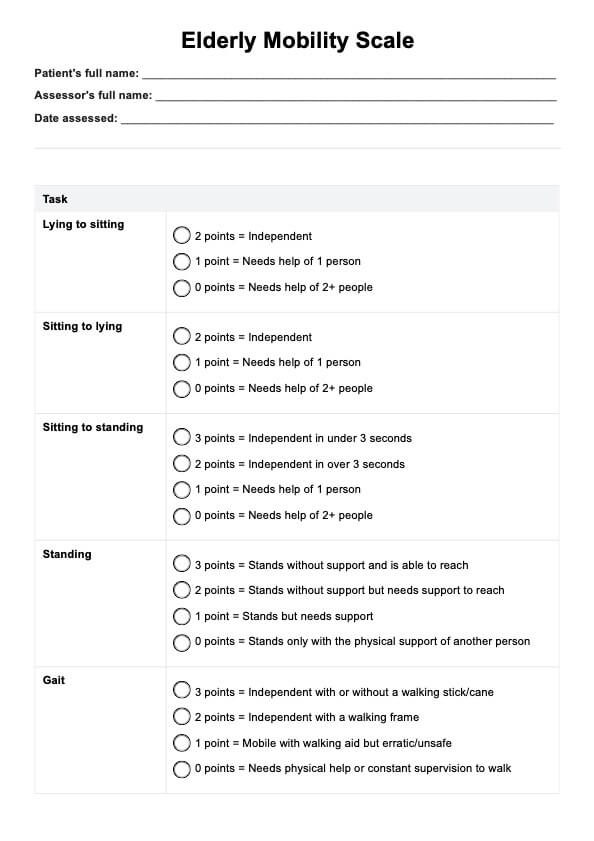
The Physical Mobility Scale is a physical assessment tool developed by physical therapists to aid them in assessing geriatric patients' mobility. Like the elderly mobility scale, this resource helps care providers identify any physical impairments elderly patients may be experiencing.
It is also useful as a functional independence measure, highlighting any difficulty patients may be experiencing in completing tasks essential for daily living. In some cases, it can also be a powerful tool for assessing people of all ages with an injury or disease that affects their mobility, including an acquired or traumatic brain injury. Conducting a physical assessment of an individual's movement ability allows physical therapists to evaluate their independence comprehensively.
By gauging such patients' functional ability, therapists can develop specific treatment plans focusing on rehabilitation, recovery, or maintenance of their mobility. This assessment tool can also be useful in tracking treatment progress as a patient regains mobility, for example, following an acquired brain injury such as a stroke.
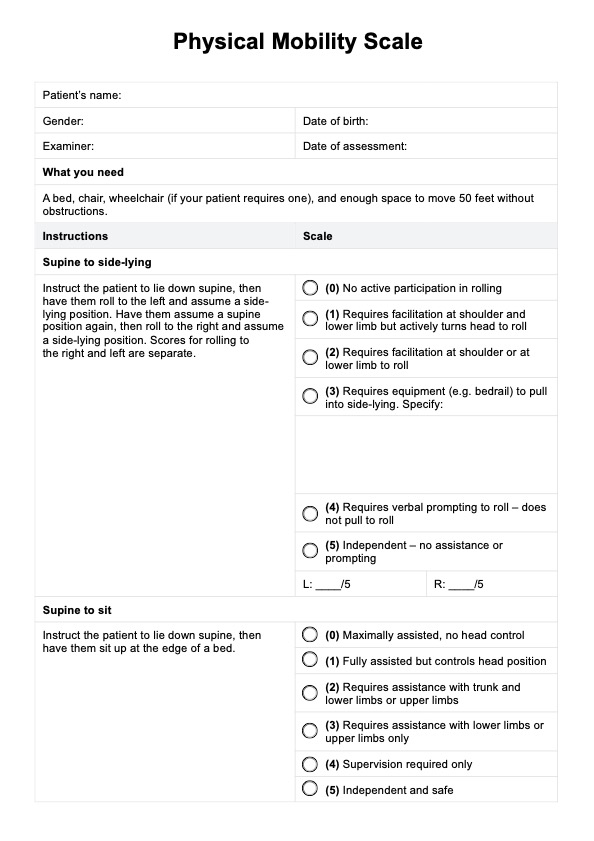
Physical Mobility Scale Template
Physical Mobility Scale Example
How to use the Physical Mobility Scale
Here's how you can incorporate this template into your practice:
Step 1: Download the template
This page offers free access to the Physical Mobility Scale PDF template. To download the PDF version, click the Download button on this guide. If you have a Carepatron account, you can access the template by clicking on the Use Template.
Step 2: Explain the assessment and prepare what you need
Explain to the patient the purpose of the assessment and how it may benefit them. Prepare all necessary equipment in advance, and take time to answer any questions the patient may have before starting.
Step 3: Conduct the test
To conduct an assessment using the Physical Mobility Scale, prepare a space with enough room to walk around without obstructions. This room should also have a bed, chair, and wheelchair (if the patient being assessed cannot walk). These also need to be present if the assessment is conducted during a house call.
Next, have the patient perform several movements, including:
- Supine to side-lying: Instruct the patient to lie down supine, then have them roll to the left and assume a side-lying position. Have them assume a supine position again, then roll to the right and assume a side-lying position. The ability to roll to the left and to the right is scored separately.
- Supine to sitting: Instruct the patient to lie down supine, then have them sit up at the edge of a bed.
- Sitting balance: Instruct the patient to sit on the edge of a bed and plant their feet on the floor. Tell them to turn and look over their shoulder (must be done on both sides), then have them reach down and touch the floor. They must maintain balance while doing both actions.
- Sitting to standing: Instruct the patient to sit on the edge of a bed and then stand up without using their hands for support.
- Standing to sitting: Instruct the patient to stand next to the edge of a bed, then have them sit down without using their hands for support.
- Standing balance: Instruct the patient to stand up and stay standing up with or without support. Have them turn and look over their shoulder (this must be done on both sides), put an object (anything works), and have them pick it up. Then, have them stand on their left or right leg for as long as they can.
- Transfers: Instruct the patient to sit on the edge of the bed, then have them stand up and transfer themselves to a wheelchair (if they require wheelchairs to move) or a chair (if they can walk).
- Ambulation: Instruct the patient to stand up (if they can walk) or have them sit in a wheelchair (if they require wheelchairs). Have them walk or push their wheelchair for a while. Make sure they move at least 50 feet.
While patients are performing each type of movement, the healthcare professional should observe them carefully and score them accordingly on the printable Physical Mobility Scale template.
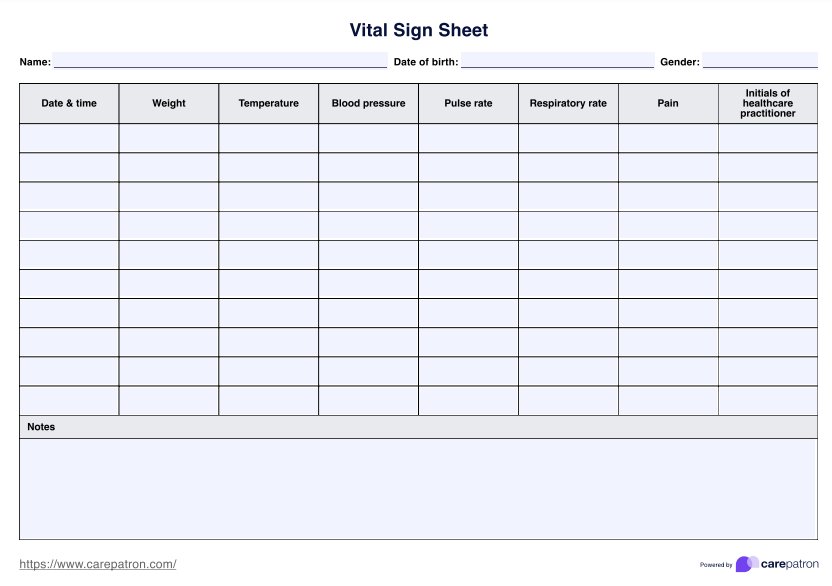
Step 4: Record results and store for future reference
Document the results carefully and keep them securely for future reference. This allows easy access to the information later, which can be helpful for tracking progress or making comparisons over time.
Physical Mobility Scale scoring and interpretation
In Physical Mobility Scale scoring, each action has six possible observations. Healthcare professionals simply need to select the appropriate answer based on their observations. The action is coded from 0 to 5 according to the patient's corresponding ability to perform it. Once all actions have been scored, add up all the scores. The total score can range from 0 to 45, with 45 signifying full independent mobility and 0 indicating minimal mobility.
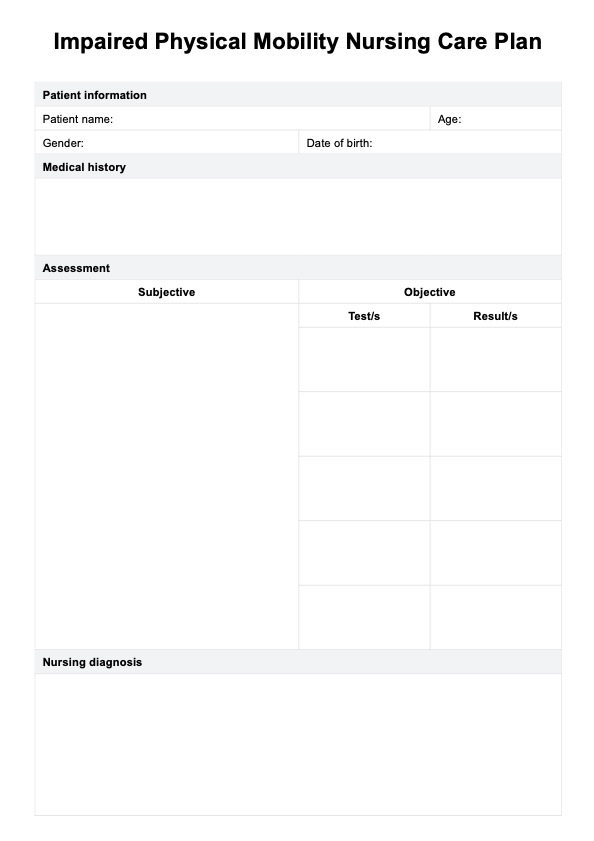
After the results have been recorded, the next step should be determining what goes into a patient's physical therapy plan. It should be based on the results. Physical therapists may also conduct other tests to assess a patient's risk of falling.
When can you use the Physical Mobility Scale template?
Here are some instances or situations when you can use this template:
During house calls
Physical therapists may have patients who are unable to bring themselves to the clinic or hospital, necessitating house calls. This is a great time to conduct an assessment using the Physical Mobility Scale because it can help physical therapists and geriatricians determine the challenges their patients face at home due to impaired mobility. These will be taken into account when they create or adjust care plans.
In long-term care facilities
Those who work in long-term care facilities that house geriatrics can benefit from using the Physical Mobility Scale. This tool can help them identify their patients' existing mobility problems and provide personalized care based on the results. It can also help determine potential problems that may arise down the line, allowing professionals to establish interventions and precautions to lower those risks.
For monitoring patients
Physical therapists in clinical settings may wish to use the Physical Mobility Scale to monitor a patient's progress. This can help determine if a treatment plan implemented is effective. If a patient's Physical Mobility Scale score is higher than their previous assessment, this indicates they are improving.
Commonly asked questions
This will depend on the patient you’re assessing, but it’s possible to accomplish the assessment within 20 minutes. Don’t be surprised if it takes longer, though.
Yes. For consistency, it would be best to conduct additional balance tests.
It would be best to conduct this every time a patient returns for a check-up or if it’s time for a scheduled house call. This isn’t a one-time, big-time assessment. As we mentioned earlier, this is an effective monitoring tool, so using it routinely will ensure you are on top of your geriatric patient’s mobility status.