Modified Barthel Index
Explore the Modified Barthel Index by Shah and colleagues. Measure your patients' functional independence with our free PDF template.


What is a Modified Barthel Index?
The Barthel Index is a well-regarded tool in physical and rehabilitation medicine, particularly for assessing functional independence in individuals, including stroke patients (Sulter et al., 1999). This index has two modified versions, developed in the 1960s by Dr. Florence Mahoney and Dorothea W. Barthel.
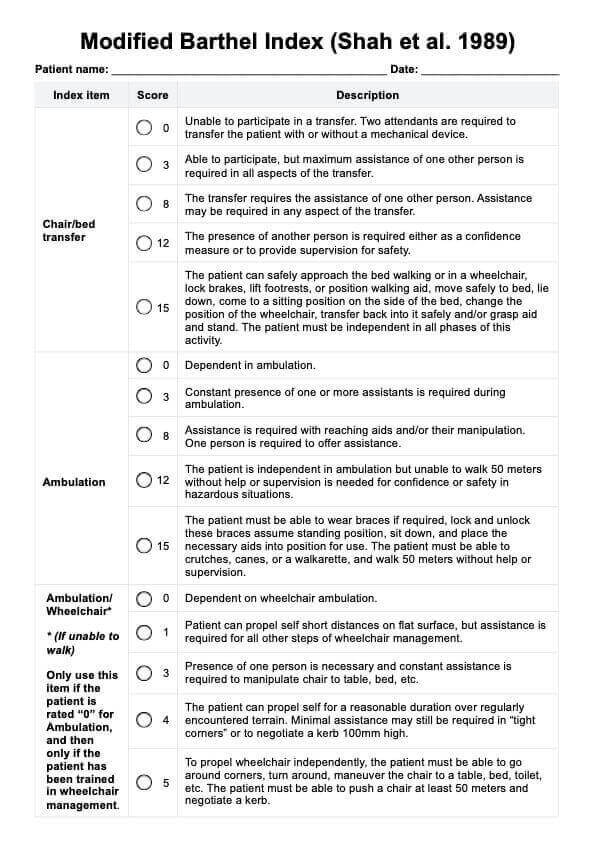
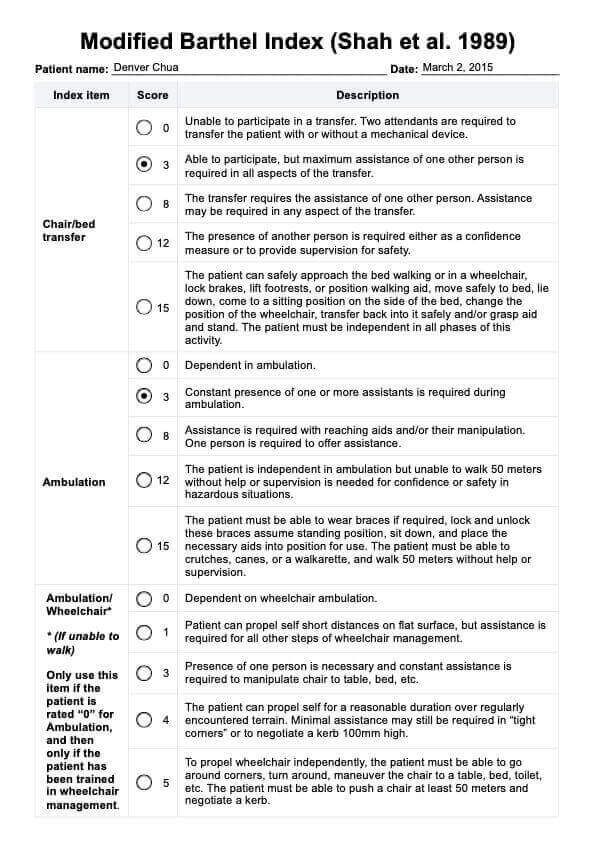
In 1988, Collin et al. revised the scoring system of the index to utilize 1-point increments, resulting in a total score that ranges from 0 to 20. This adjustment was made to address the “disproportionate impression of accuracy” (Collin et al., 1988). Subsequently, in 1989, Shah et al. further refined the index to enhance its sensitivity and reliability in assessing stroke rehabilitation outcomes, including inpatient rehabilitation. The Shah Modified Barthel Index retains the original scoring range of 0-100, but it introduced a five-point rating scale to improve both reliability and sensitivity in detecting changes.
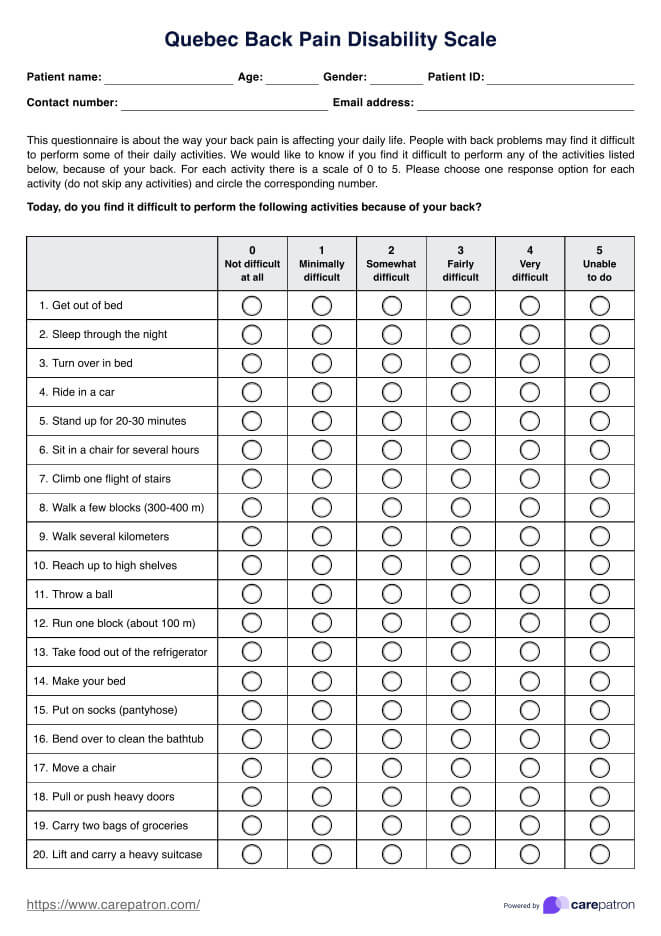
Carepatron has created a template based on the Shah et al. version. This Modified Barthel Index (MBI) is a comprehensive instrument for measuring an individual's capacity to perform essential activities of daily living (ADLs). The assessment is especially valuable for evaluating the functional status of patients recovering from strokes or other brain injuries.
The Modified Barthel Index by Shah and colleagues, along with the Functional Independence Measure, is one of the most widely used tools for assessing functional independence in individuals with disabilities. While the original Barthel Index effectively captures significant changes in activities of daily living, it may overlook smaller yet meaningful incremental improvements.
For patients demonstrating substantial progress, both indices show similar responsiveness. However, the Modified Barthel Index (Shah version) is specifically tailored to identify more subtle changes in a patient's ADL performance, making it particularly advantageous in rehabilitation settings where gradual improvements are common (Wang et al., 2022).
Modified Barthel Index Template
Modified Barthel Index Example
How to use the Modified Barthel Index template
To maximize this tool in your clinical practice, follow these steps:
Step 1: Download the free MBI template
To use the Modified Barthel Index (Shah version) template in the Carepatron app, just click the "Use Template" button. If you prefer, you can also click the "Download" button to get a PDF copy.
Step 2: Familiarize yourself with the index
Before assessing your patient, it is essential to understand the different components of the Modified Barthel Index and how they are scored. Familiarize yourself with the scale and scoring methods to ensure accurate and consistent evaluations.
Step 3: Conduct a comprehensive assessment
When conducting an MBI assessment, it is crucial to observe your patient's performance in each activity instead of relying solely on their self-report. This approach can provide more reliable results and better reflect a patient's functional status.
Step 4: Document any changes in performance
As mentioned earlier, the Modified Barthel Index (Shah version) is particularly useful for detecting subtle improvements in ADL performance. Therefore, accurately documenting any changes observed during subsequent assessments is important. These changes can also help inform treatment plans and track progress over time.
Step 5: Use the MBI in conjunction with other assessment tools
While the Modified Barthel Index is a valuable tool, it should not be used as the sole measure to evaluate a patient's functional status. Use it in conjunction with other clinical assessments and observations to gain a comprehensive understanding of a patient's overall functioning.
Step 6: Review and update regularly
As a patient's condition can change over time, it is essential to review and update their MBI score regularly. This ensures that their treatment plan and care needs are continuously reassessed and adjusted accordingly.
Scoring and interpretation
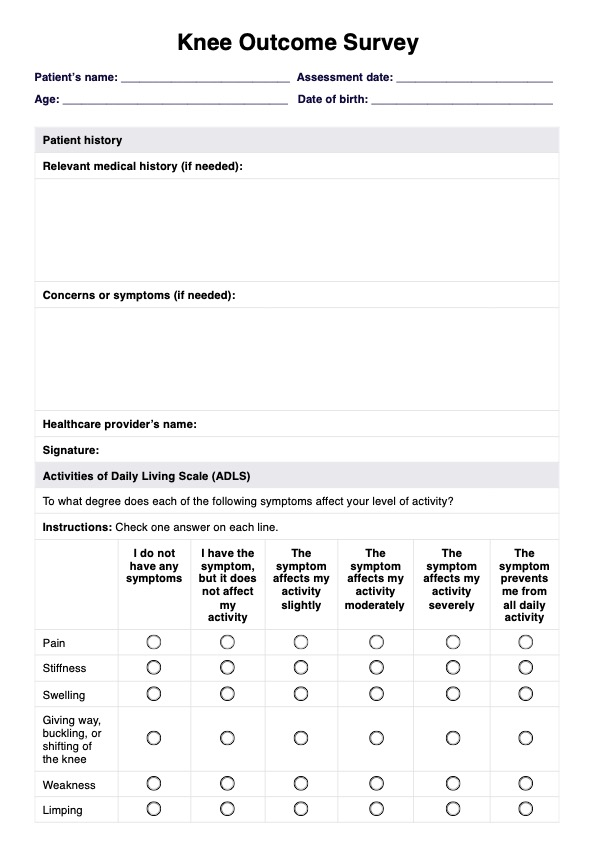
The Modified Barthel Index developed by Shah et al. (1989) includes specific items that evaluate various forms of assistance needed by individuals. These items cover assistance required for ambulation, feeding, bathing, personal hygiene, and dressing. Additionally, it assesses the presence or absence of fecal and urinary incontinence and the support required for transfers, walking, and climbing stairs.
The sum scores in the MBI are calculated by summing the individual item scores, with a maximum possible score of 100, indicating complete functional independence. The interpretation of the total final score is typically based on the following guidelines:
- 91–99: Slight dependency
- 61–90: Moderate dependency
- 21–60: Severe dependency
- 0–20: Total dependency
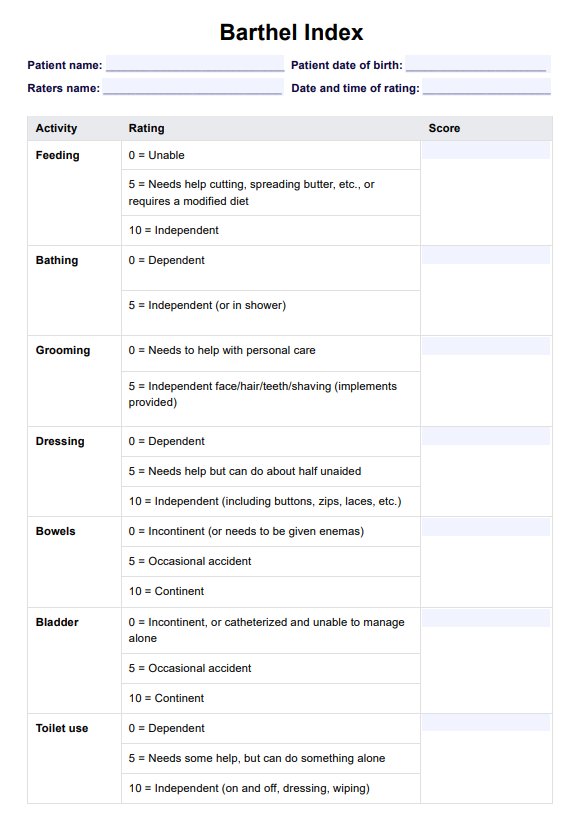
How is this different from the regular index?
The original index was designed as a three-item ordinal rating scale, with certain items utilizing a four-item scale. It includes ten items evaluated based on an individual's ability to perform a task or activity independently, with assistance, or with complete dependence.
According to Sinoff and Ore (1997), the scoring on the Barthel Index (BI) can be interpreted as follows:
- A score of 80-100 indicates independence
- A score of 60-79 suggests minimal assistance is needed with activities of daily living
- A score of 40-59 reflects partial dependence
- A score of 20-39 signifies high dependence
This version by Shah et al. (1989) also has 10 items (with two items combined for ambulation) and varying rating options based on the item assessed. For example, for feeding, instead of using the simple scoring system, this version's rating options are as follows:
- 0: Dependent in all aspects and needs to be fed, nasogastric needs to be administered.
- 2: Can manipulate an eating device, usually a spoon, but someone must provide active assistance during the meal.
- 5: Able to feed self with supervision. Assistance is required with associated tasks such as putting milk/sugar into tea, salt, pepper, spreading butter, turning a plate or other “set up” activities.
- 8: Independence in feeding with prepared tray, except may need meat cut, milk carton opened or jar lid etc. The presence of another person is not required.
- 10: The patient can feed self from a tray or table when someone puts the food within reach. The patient must put on an assistive device if needed, cut food, and if desired use salt and pepper, spread butter, etc.
When would you typically use a Modified Barthel Index?
The MBI (Shah version) is a valuable tool for assessing functional independence and ensuring a favorable patient recovery outcome. Here are the common instances when to use MBI:
Stroke recovery in rehabilitation settings
Clinical assessment tools like the MBI are frequently employed in rehabilitation settings, especially for stroke survivors undergoing physical therapy. As a reliable assessment tool, the MBI measures motor abilities crucial for daily living tasks. In the aftermath of an ischemic stroke, healthcare professionals use the MBI to evaluate the patient's functional independence and tailor rehabilitation plans accordingly.
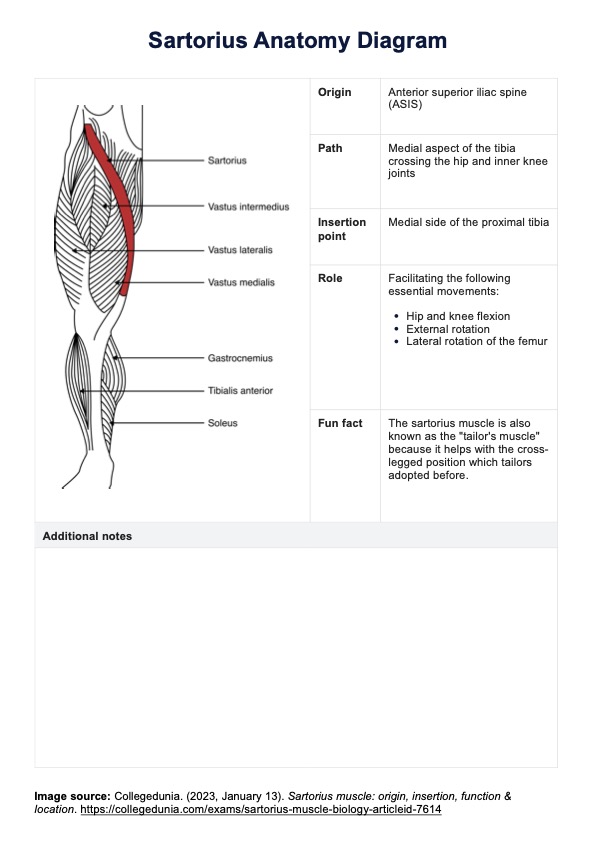
Orthopedic pathologies and musculoskeletal disorders
The MBI proves valuable in clinical practice in orthopedic diseases or musculoskeletal disorders. It assesses the patient's ability to perform activities like ambulation, transferring from chair to bed, and dressing, aiding orthopedic specialists and physical therapists in gauging the impact of these pathologies on daily functioning.
Elderly population and long-term care
With a growing aging population, evaluating functional independence is crucial for providing appropriate care and support to older adults. The MBI assesses independent living skills, enabling healthcare professionals to identify areas of weakness and develop personalized care plans. It also aids in evaluating the effectiveness of long-term care interventions in maintaining or enhancing functional ability.
Evaluating patients with severe disability
The Modified Barthel Index is also particularly useful for assessing patients with severe disabilities, as it can accurately reflect their level of functional independence in ADLs. In such cases, the scoring may demonstrate a lower capacity for independent performance across various tasks, such as mobility and personal care.
Clinical research studies
The Modified Barthel Index can be used to measure functional outcomes in various rehabilitation research studies, including those evaluating treatment effectiveness or comparing different interventions. Its widespread use and validated scoring system make it a reliable tool for measuring changes in functional ability over time.
References
Collin, C., Wade, D. T., Davies, S., & Horne, V. (1988). The Barthel ADL index: A reliability study. International Disability Studies, 10(2), 61–63. https://doi.org/10.3109/09638288809164103
Physiopedia. (2019). Barthel Index. https://www.physio-pedia.com/Barthel_Index
Shah, S., Vanclay, F., & Cooper, B. (1989). Improving the sensitivity of the barthel index for stroke rehabilitation. Journal of Clinical Epidemiology, 42(8), 703–709. https://doi.org/10.1016/0895-4356(89)90065-6
Sinoff, G., & Ore, L. (1997). The barthel activities of daily living index: Self-Reporting versus actual performance in the old-old (≥ 75 years). Journal of the American Geriatrics Society, 45(7), 832–836. https://doi.org/10.1111/j.1532-5415.1997.tb01510.x
Sulter, G., Steen, C., & Jacques De Keyser. (1999). Use of the Barthel index and modified Rankin scale in acute stroke trials. Stroke, 30(8), 1538–1541. https://doi.org/10.1161/01.str.30.8.1538
Wang, Y.-C., Chang, P.-F., Chen, Y.-M., Lee, Y.-C., Huang, S.-L., Chen, M.-H., & Hsieh, C.-L. (2022). Comparison of responsiveness of the barthel index and modified barthel index in patients with stroke. Disability and Rehabilitation, 45(6), 1–6. https://doi.org/10.1080/09638288.2022.2055166
Commonly asked questions
The Modified Barthel Index (MBI) measures an individual's functional independence in performing ADLs. It assesses the ability to carry out mobility, personal hygiene, and feeding tasks, among others, providing a comprehensive evaluation of the patient's functional outcome.
Scoring the Modified Barthel Index (MBI) involves assigning a numerical value to the patient's level of independence in specific activities or their need for physical assistance. This allows for consistent scoring by different raters, as evidenced by good reliability measures. Healthcare professionals evaluate the patient's performance in tasks such as transferring, ambulation, and personal hygiene, deriving an overall score that reflects their functional abilities.
The time required to administer the Modified Barthel Index (MBI) varies based on the patient's condition and the complexity of their activities of daily living (ADLs). Generally, it takes around 10 to 15 minutes to assess and score the patient's functional independence using the MBI. The duration may be influenced by factors such as the patient's cooperation, whether or not the patient requires supervision, and the thoroughness of the assessment.