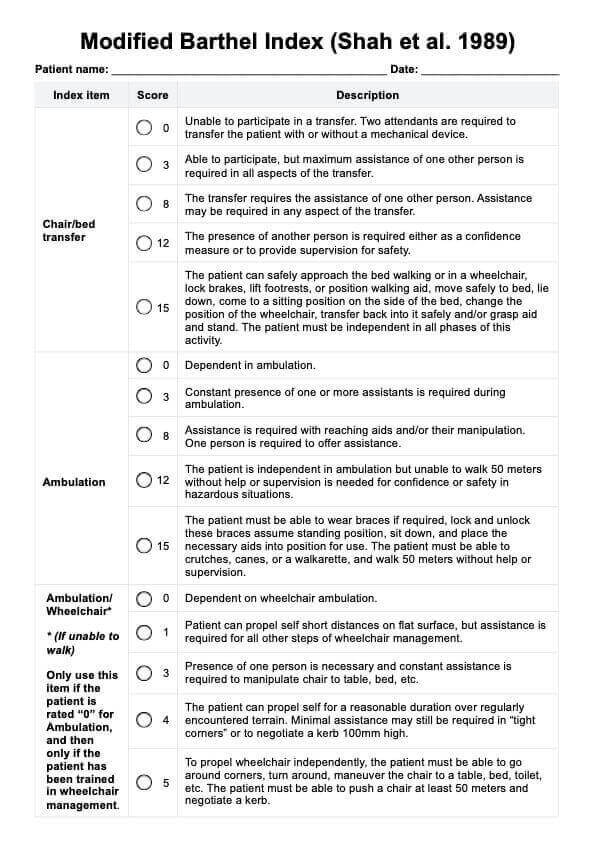
Barthel Index
Use the Barthel Index to determine functional independence to inform the treatment plan of patients struggling with ADLs


What is the Barthel Index?
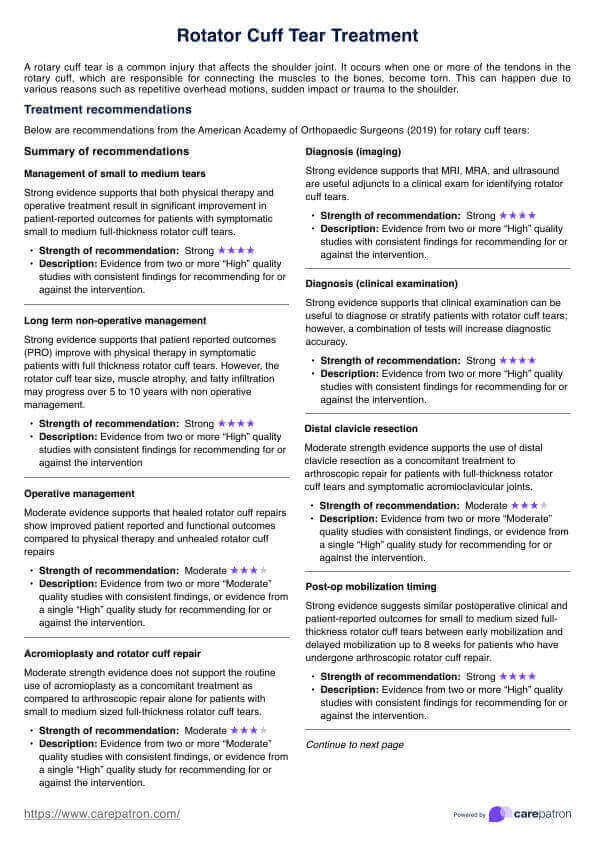
The Barthel Index (BI) is a widely used functional evaluation measure that assesses a person's ability to perform activities of daily living (ADLs). Developed by Mahoney and Barthel (1965), it was initially created to measure functional and physical disability in stroke survivors. However, its usefulness has extended to a broader range of conditions, including:
- Musculoskeletal disorders
- Neuromuscular or musculoskeletal disorder
- Brain injury
- Mental disorders
- Multiple sclerosis
- Hospital discharge planning
- Nursing home care
- Stroke and post-stroke care
The BI, a widely used functional outcomes measure, is a ranked scale with ten items, each focusing on a specific ADL. These include:
- Feeding
- Bathing
- Grooming
- Dressing
- Bowel control
- Bladder control
- Toilet use
- Transfer (moving between sitting and standing)
- Mobility (on level surfaces)
- Stair climbing
The core concept behind the Barthel Index is functional independence. This refers to a person's ability to manage daily tasks without assistance. The Barthel Index measures a patient's progress in functional recovery, which is regaining independence after an illness or injury.
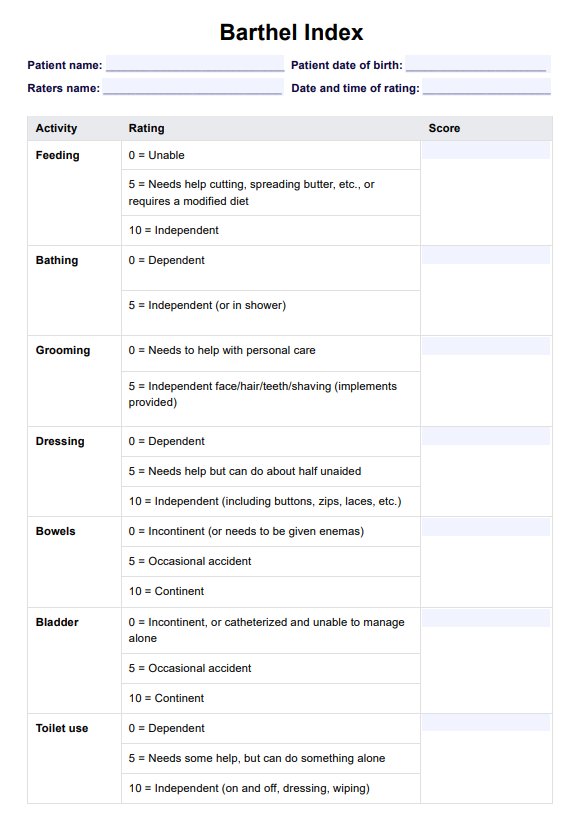
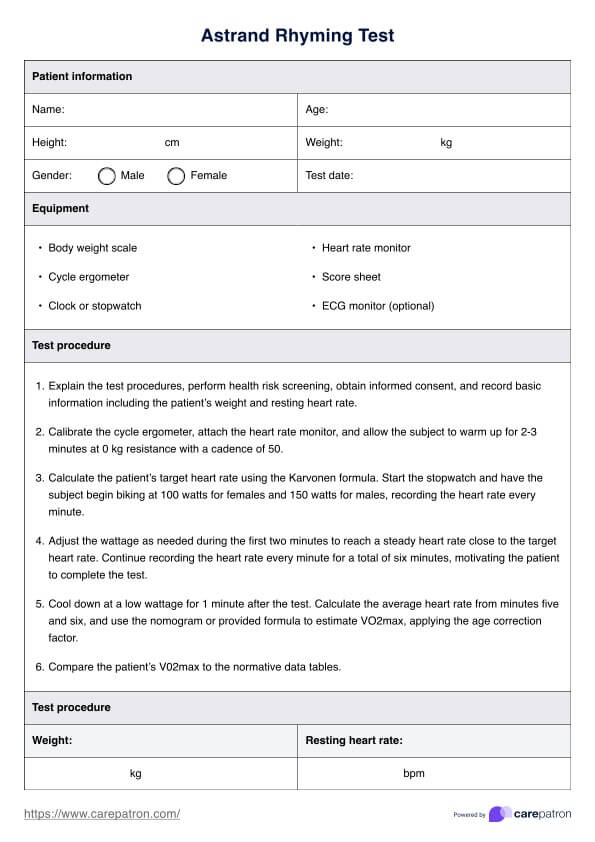
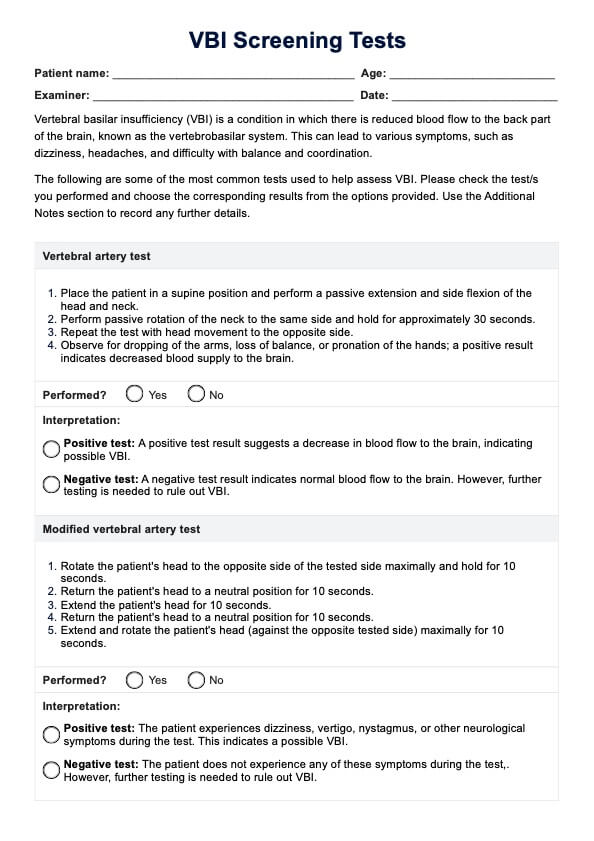
Barthel Index Template
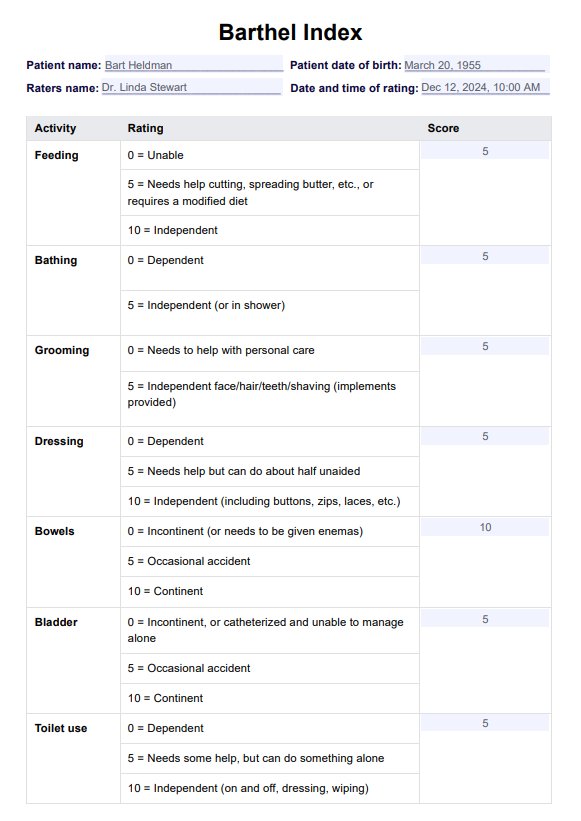
Barthel Index Example
How to use the Barthel Index
The Barthel ADL Index is a helpful tool to assess a person's physical function and ability to manage daily activities without assistance. It can even be used as a self-report measure, but the interpretation and clinical decisions still have to be made by a specialist. The following are the steps on how you can maximize this resource:
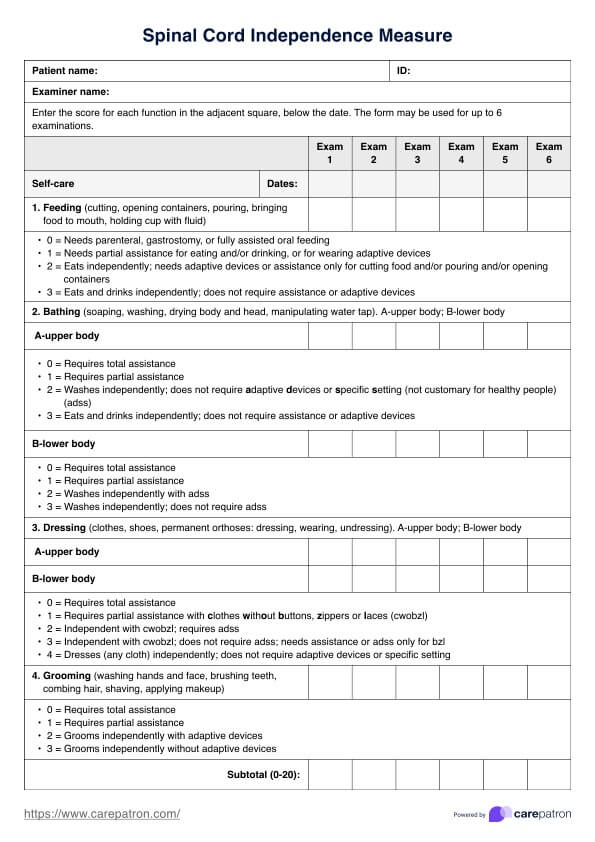
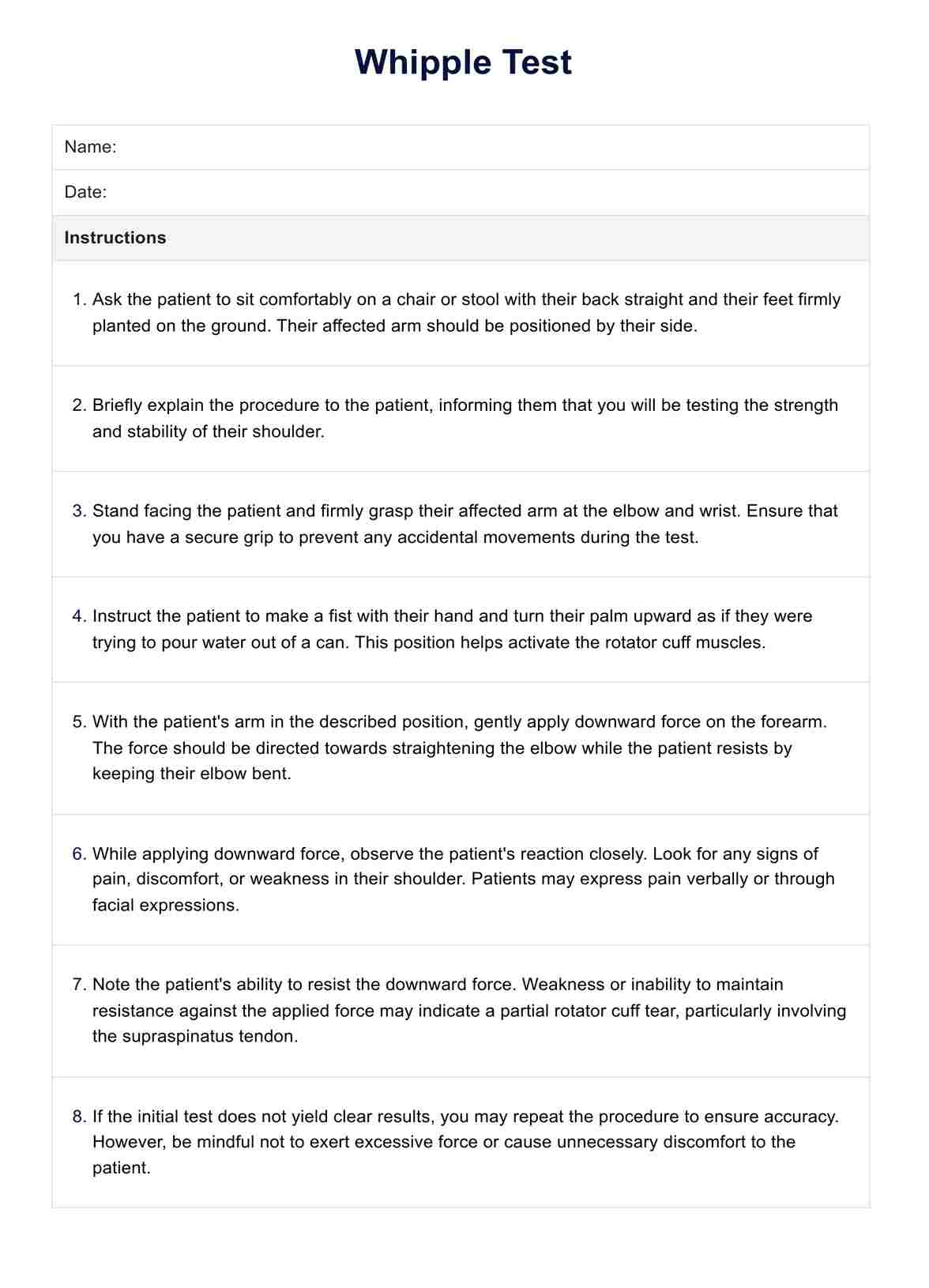
Step 1: Understand the purpose and components
The Barthel Index is widely used to measure disability and assess functional independence in ADLs. It consists of 10 items: personal hygiene, bathing, feeding, toilet use, dressing, bowel control, bladder control, transfers, mobility on level surfaces, and stair climbing.
Step 2: Prepare for assessment
Download the Barthel Index template from Carepatron by clicking the "Use template" button. This allows you to customize our Barthel Index template for your practice. For a PDF copy, you can also click "Download." Next, gather other necessary materials, such as a pen or pencil and any assistive devices the patient typically uses. Ensure the assessment takes place in a quiet and comfortable environment. Introduce the purpose of the assessment to the patient and obtain their consent for the direct observation process.
Step 3: Conduct the assessment
Observe the patient performing each ADL task or rely on self-report or caregiver input if direct testing is impossible. It's also important to note the activities that the patient can accomplish while carrying aid to assist them. When scoring each item, this ordinal scale typically ranges from 0 to 10, with some items having a maximum score of 15. The scoring criteria should be followed accurately to ensure consistency in assessment.
Step 4: Calculate the total score
Add up each item's scores to obtain the total BI score. The maximum score is 100, indicating complete functional independence. Lower scores indicate varying degrees of dependence.
Step 5: Interpret and document the results
Interpret the total BI composite score based on established guidelines included in the template. Document the outcome measures in the patient's medical record, including the total scores range, individual item scores, and any relevant observations or comments. Use the BI score and other clinical assessments to guide care planning, discharge planning, and treatment decisions, especially in stroke recovery.
Scoring and interpretation
The Barthel Index's scoring system is designed to evaluate the patient's functional abilities objectively. As mentioned, the BI consists of 10 items, each scored on a scale ranging from 0 to either 10 or 15 points, depending on the specific task. The scoring criteria for each item are as follows:
- Feeding: 0 (unable), 5 (needs help), 10 (independent)
- Bathing: 0 (dependent), 5 (independent)
- Grooming: 0 (needs to help with personal care), 5 (independent)
- Dressing: 0 (dependent), 5 (needs help), 10 (independent)
- Bowel control: 0 (incontinent), 5 (occasional accident), 10 (continent)
- Bladder control: 0 (incontinent), 5 (occasional accident), 10 (continent)
- Toilet use: 0 (dependent), 5 (needs some help), 10 (independent)
- Transfers (bed to chair and back): 0 (unable, no sitting balance), 5 (major help), 10 (minor help), 15 (independent)
- Mobility (on level surfaces): 0 (immobile), 5 (wheelchair independent), 10 (walks with the help of one person), 15 (independent)
- Stairs: 0 (unable), 5 (needs help), 10 (independent)
The total BI score is calculated by summing the individual item scores, with a maximum possible score of 100, indicating complete independence in ADLs.
When would you typically use a Barthel Index?
The Barthel Index is a great choice when it comes to understanding a patient's ability to manage ADLs. Here are some common scenarios where the BI becomes a crucial and valuable tool:
Assessing stroke recovery
Initially designed for stroke patients, the BI provides a clear picture of functional independence after a stroke. This helps guide therapy plans and track progress in regaining daily living skills.
Evaluating functional decline
The BI can be used for people with various conditions that might affect their ability to perform ADLs. This includes brain injuries, musculoskeletal disorders, or multiple sclerosis.
Planning hospital discharge
Knowing a patient's functional independence level helps determine if they require additional physical assistance at home or in a rehabilitation facility after discharge.
Monitoring progress in rehabilitation
The BI's simple scoring system allows for regular assessments, making tracking a patient's progress easy and adjusting rehabilitation strategies as needed.
References
Mahoney, F. I., & Barthel, D. W. (1965). Functional evaluation: The Barthel Index. Maryland State Medical Journal, 14, 61–65.
Commonly asked questions
Yes, the Barthel Index (BI) scoring can be considered relatively objective. The BI uses a standardized scoring system with clear criteria for each item, ranging from 0 (completely dependent) to 10 or 15 (completely independent). However, it is essential to note that the assessment still requires some subjective judgment, especially when observing the patient's performance or relying on self-report or caregiver input.
The Barthel Index is widely used to assess functional independence in activities of daily living (ADLs) across a variety of clinical settings and patient populations, including stroke patients, patients with musculoskeletal disorders, brain injuries, mental disorders, and multiple sclerosis. This can also be helpful in hospital discharge planning and nursing home care.
Functional assessment tools like the Barthel Index (BI) are commonly used to monitor functional status in patients, especially those with chronic stroke. It is typically administered multiple times, such as at admission, during treatment, and at discharge, to track changes in functional abilities and determine the level of assistance required. Repeated use of the BI is reliable and responsive to changes in functional status, making it an effective tool for assessing progress over time. While a single administration of the BI can provide valuable insights, it is generally recommended to use it regularly to accurately monitor the patient's functional trajectory and guide treatment decisions.