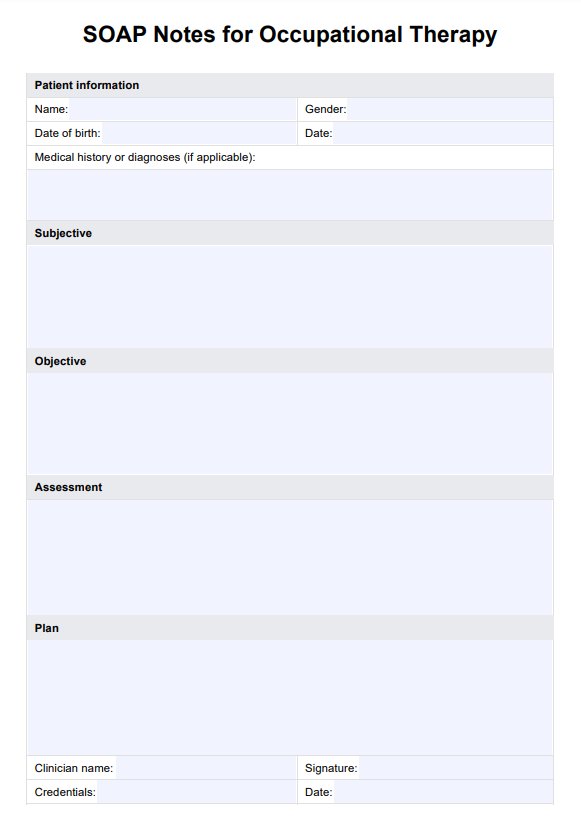
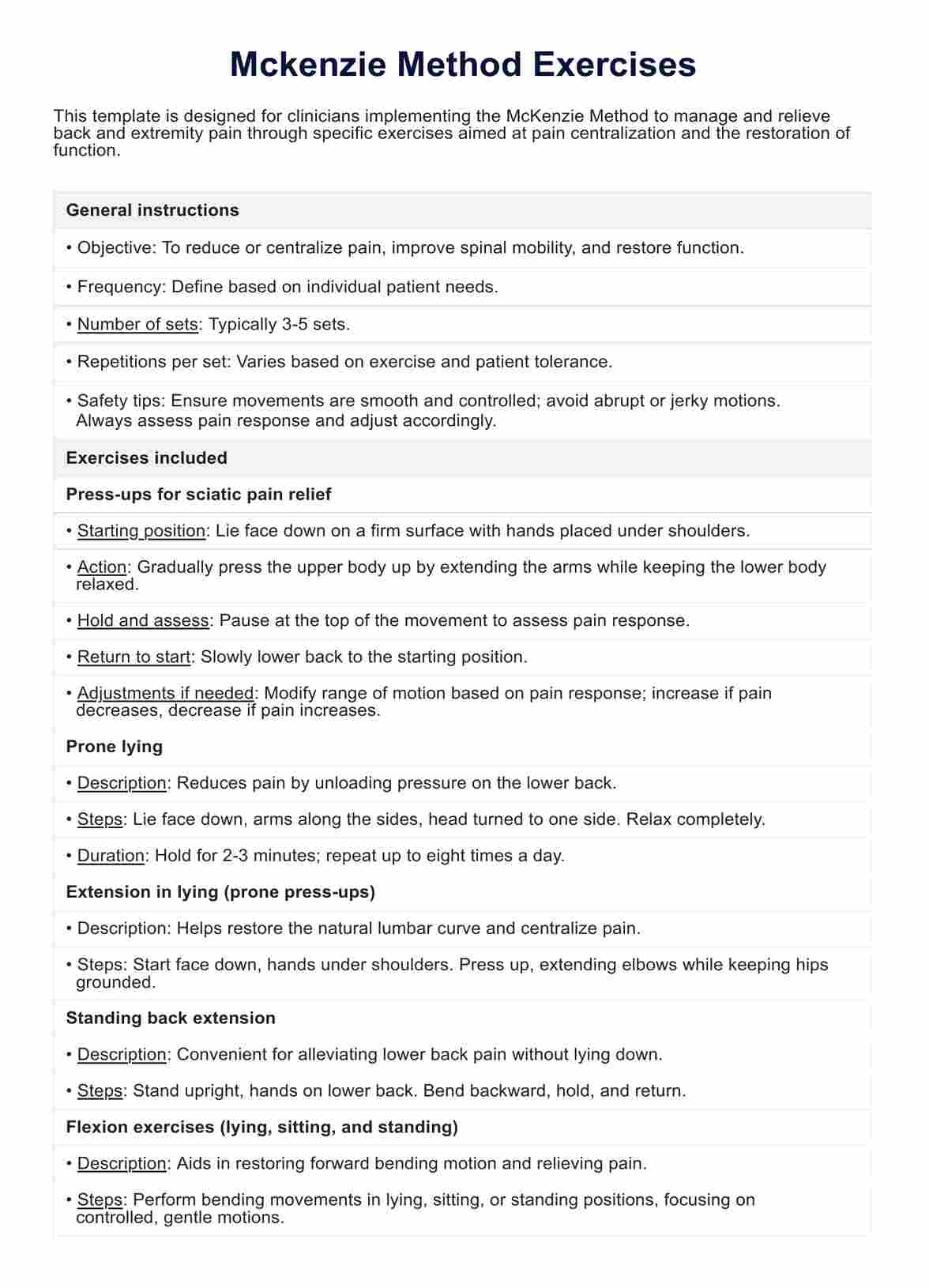
SOAP Notes For Occupational Therapy Template
A simple, downloadable PDF template for taking SOAP Notes in occupational therapy.



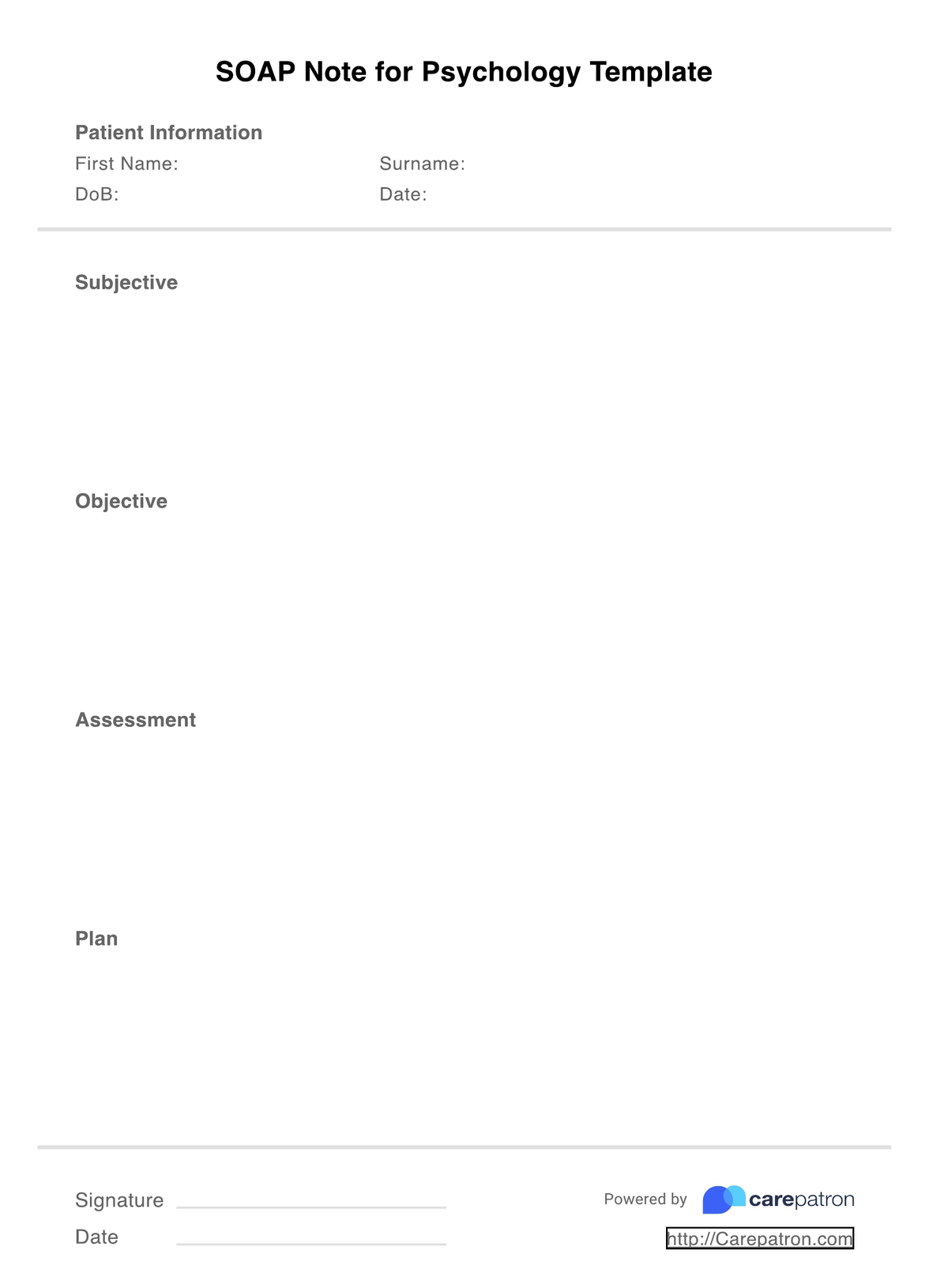
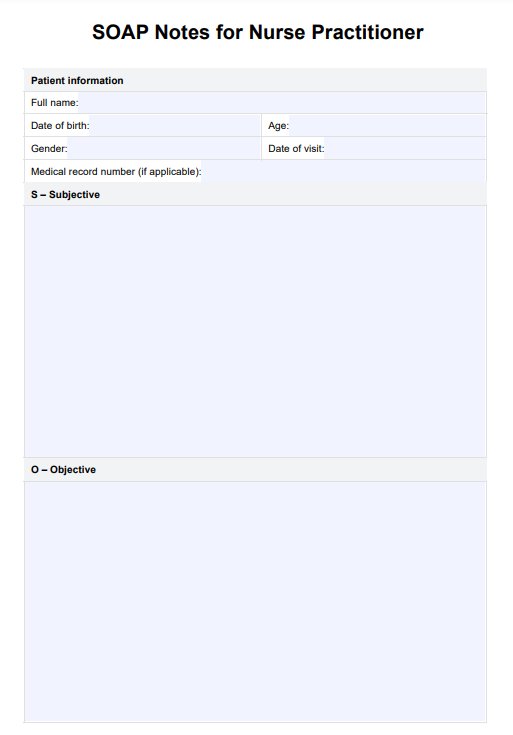
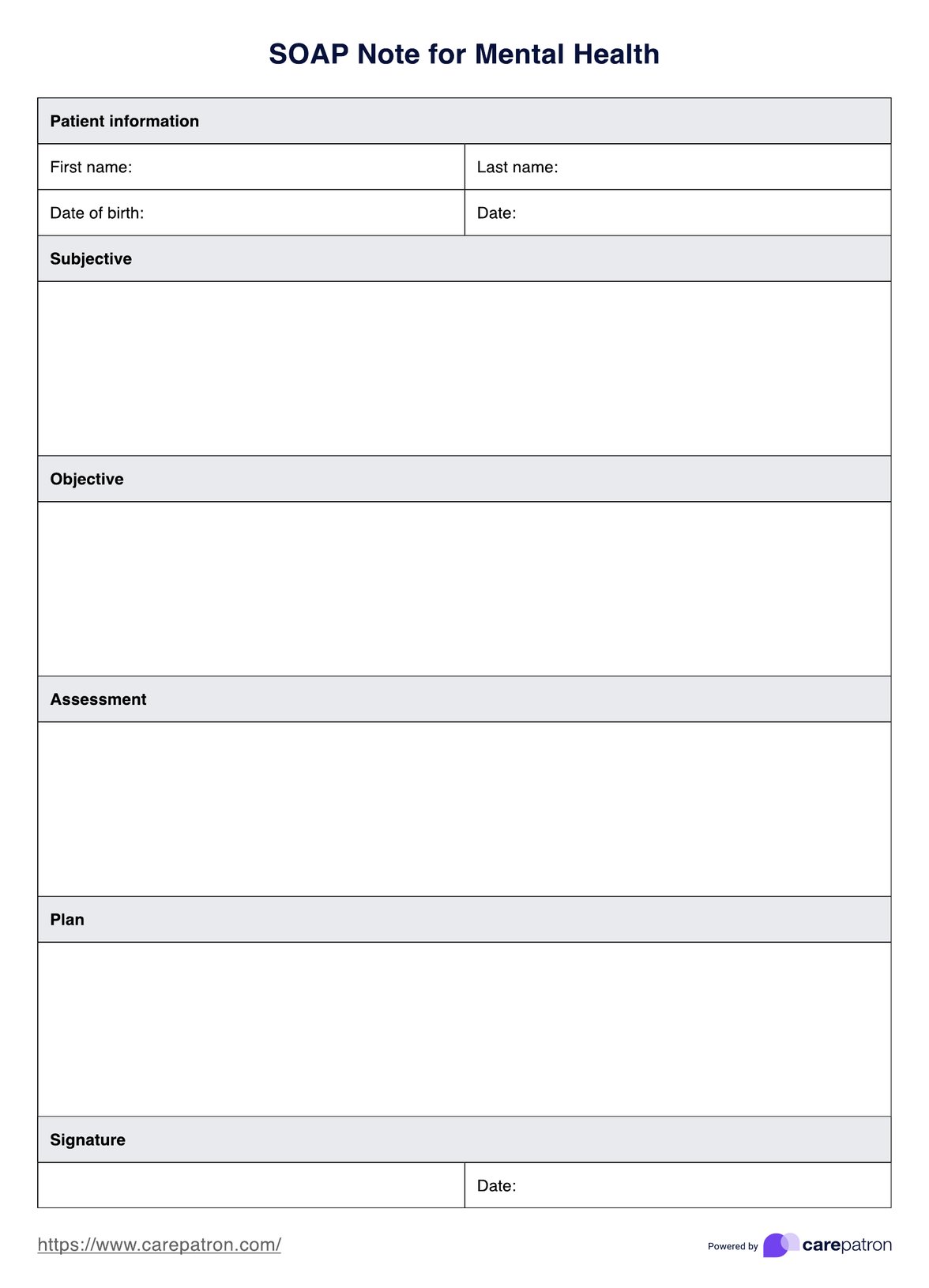
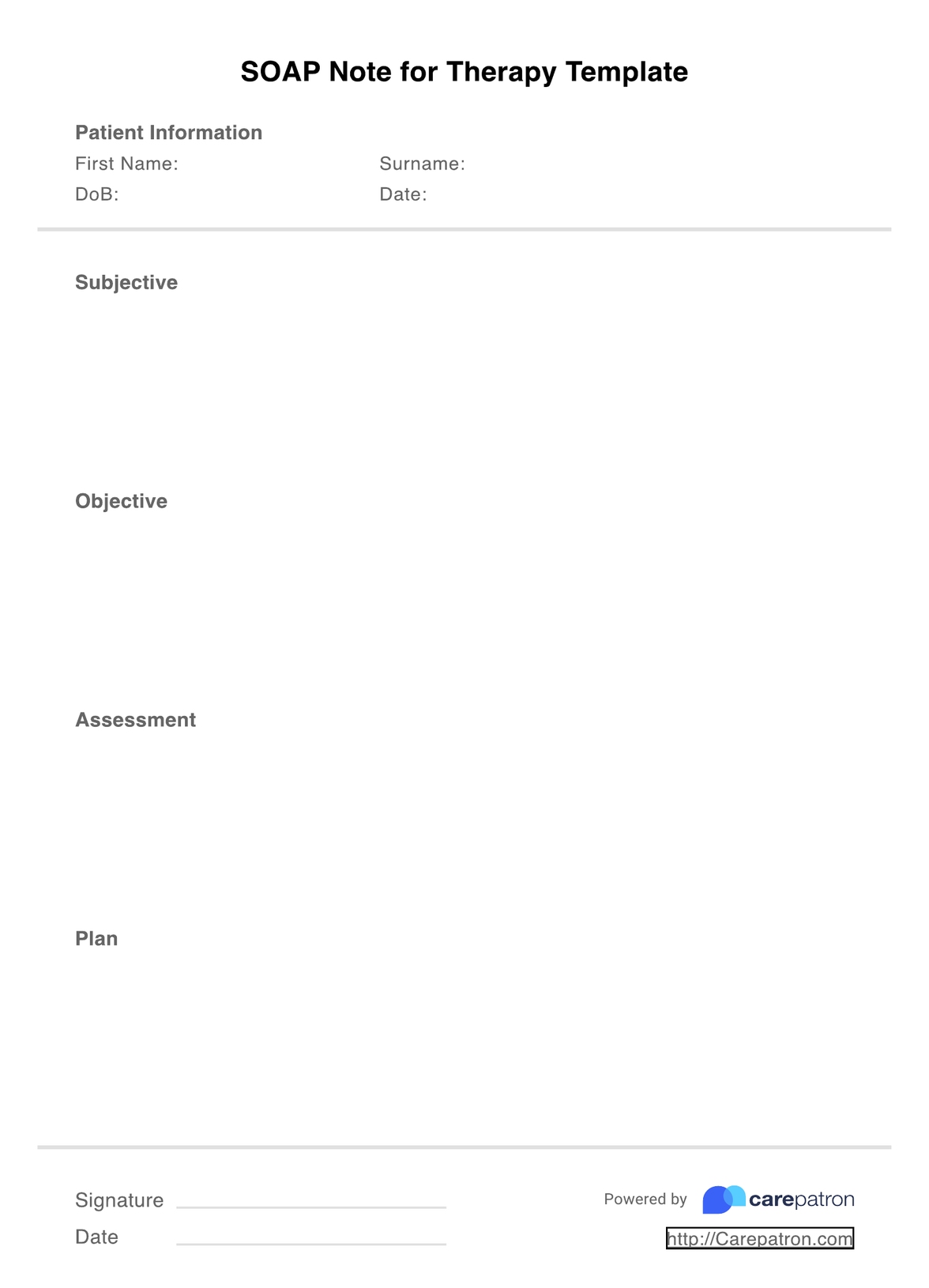
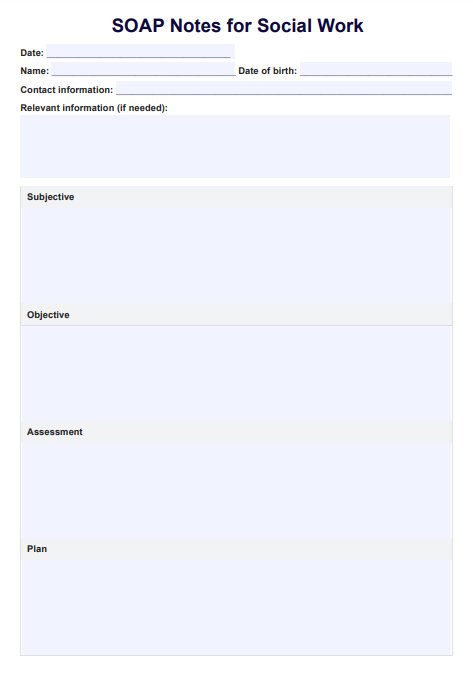
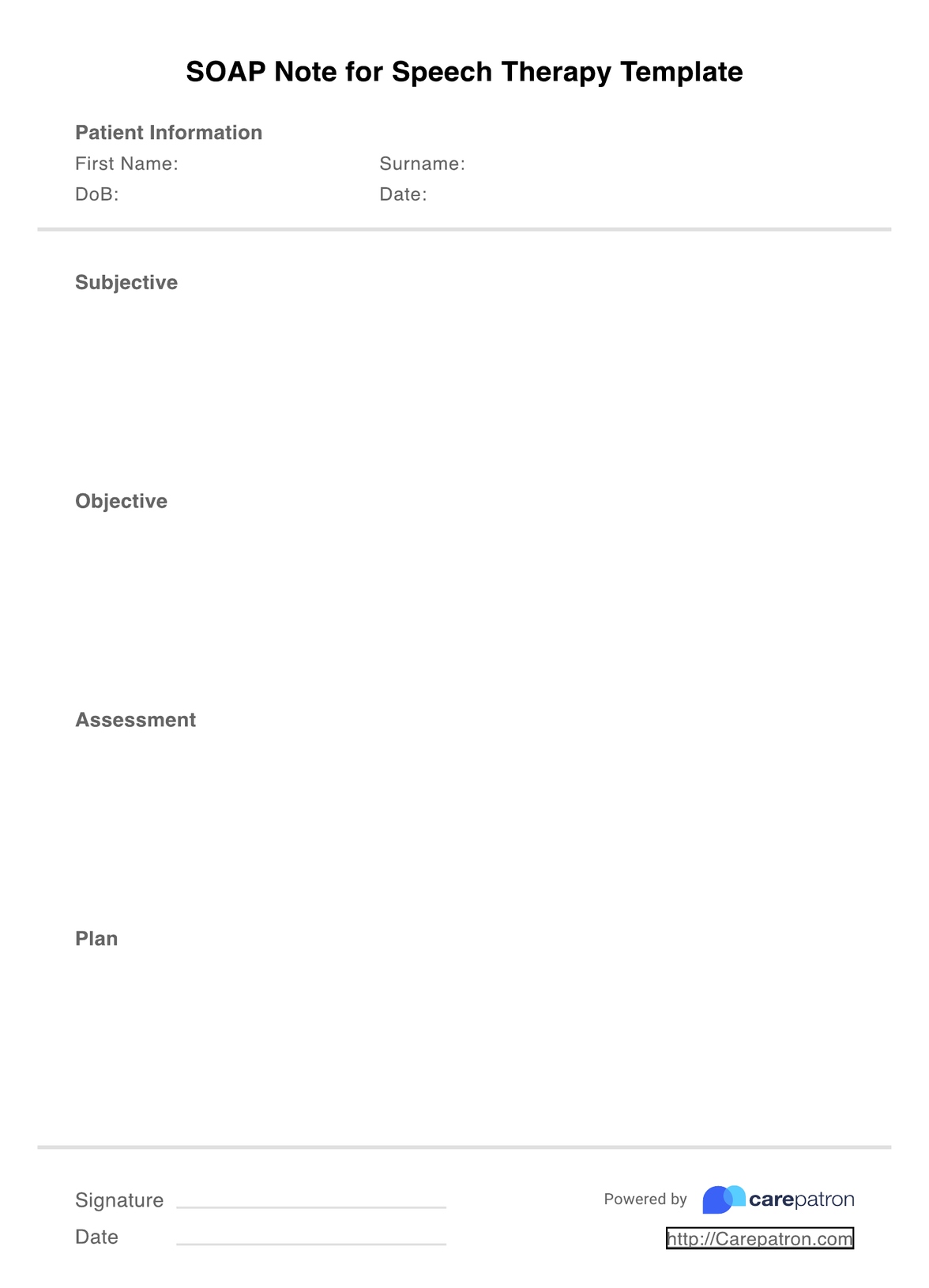
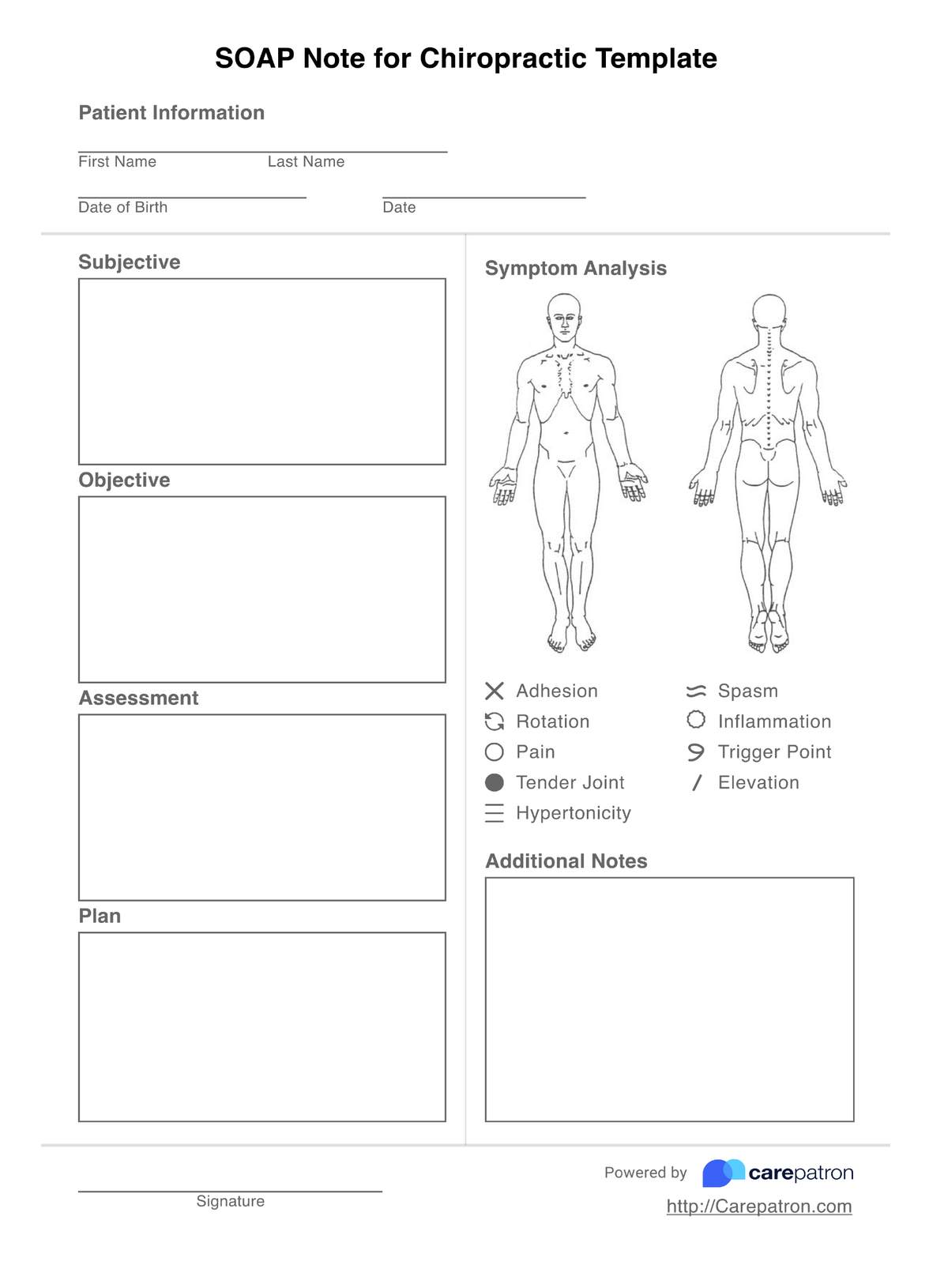
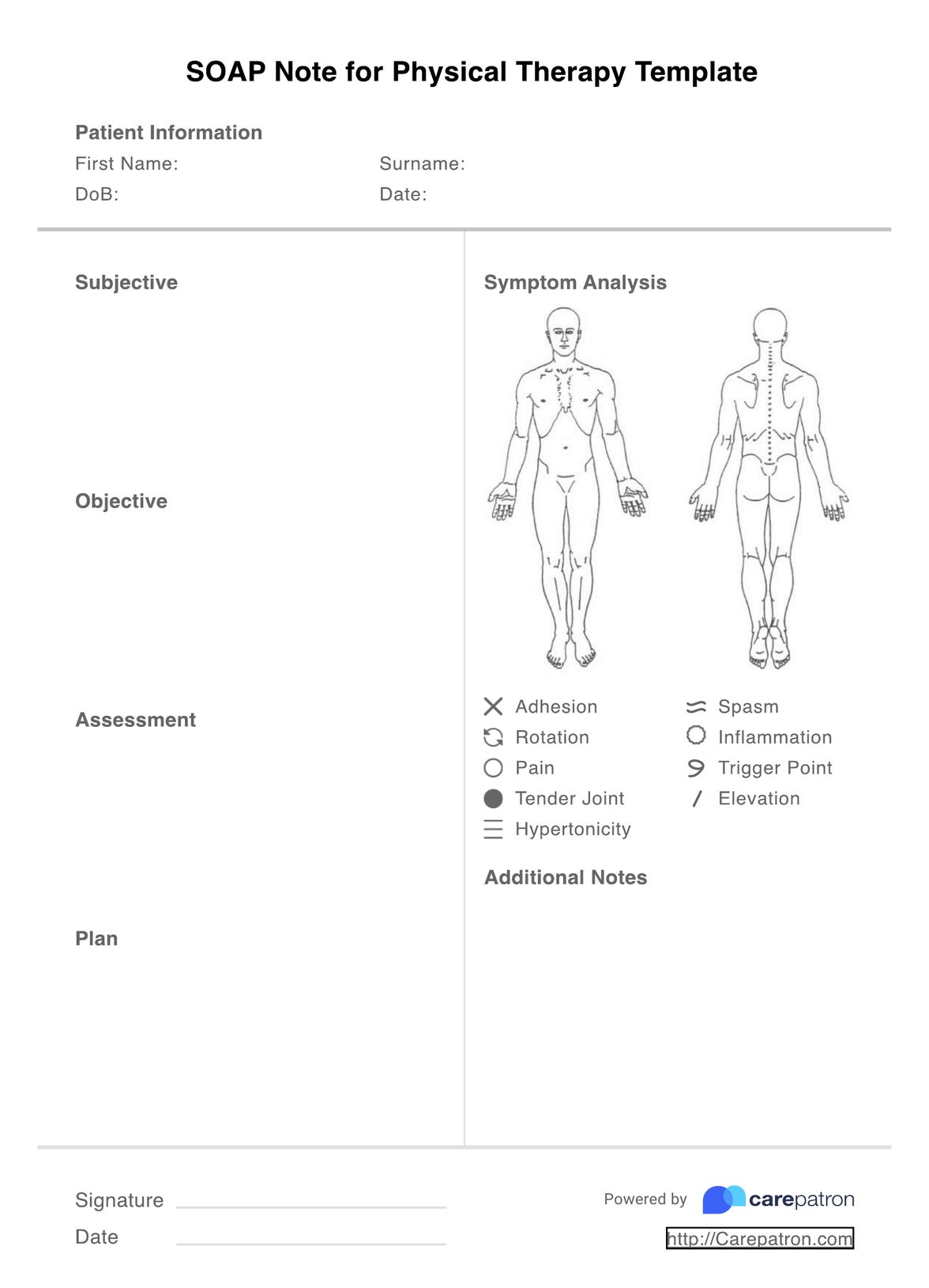
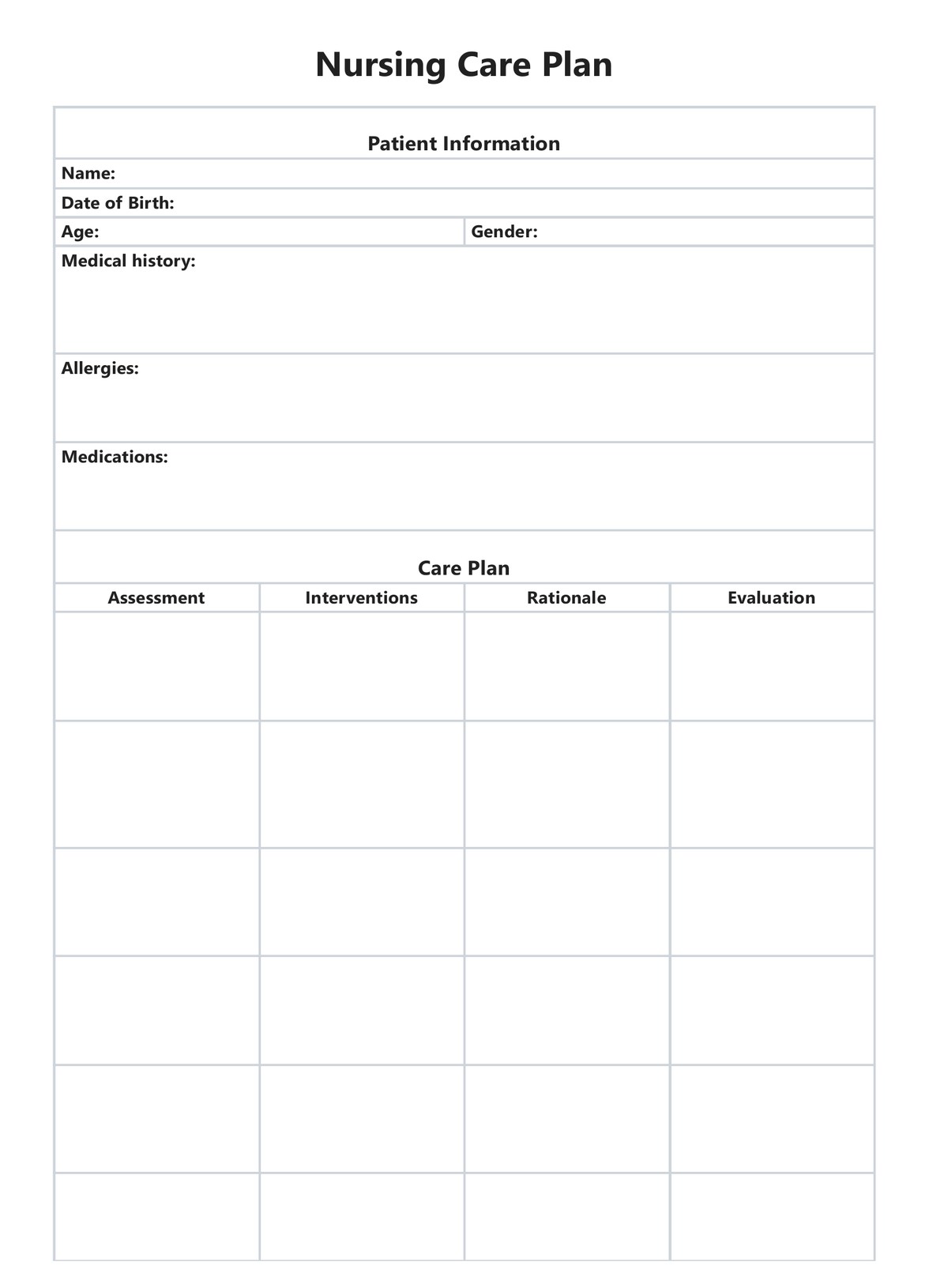
The SOAP note format is well-known worldwide and used in many healthcare settings. SOAP stands for subjective, objective, assessment, and plan. This format helps organize information systematically, ensuring a comprehensive and clear documentation process.
An occupational therapy (OT) SOAP notes template is designed to help take comprehensive and well-structured notes during client sessions.
PDF Template
Download PDF TemplateExample PDF
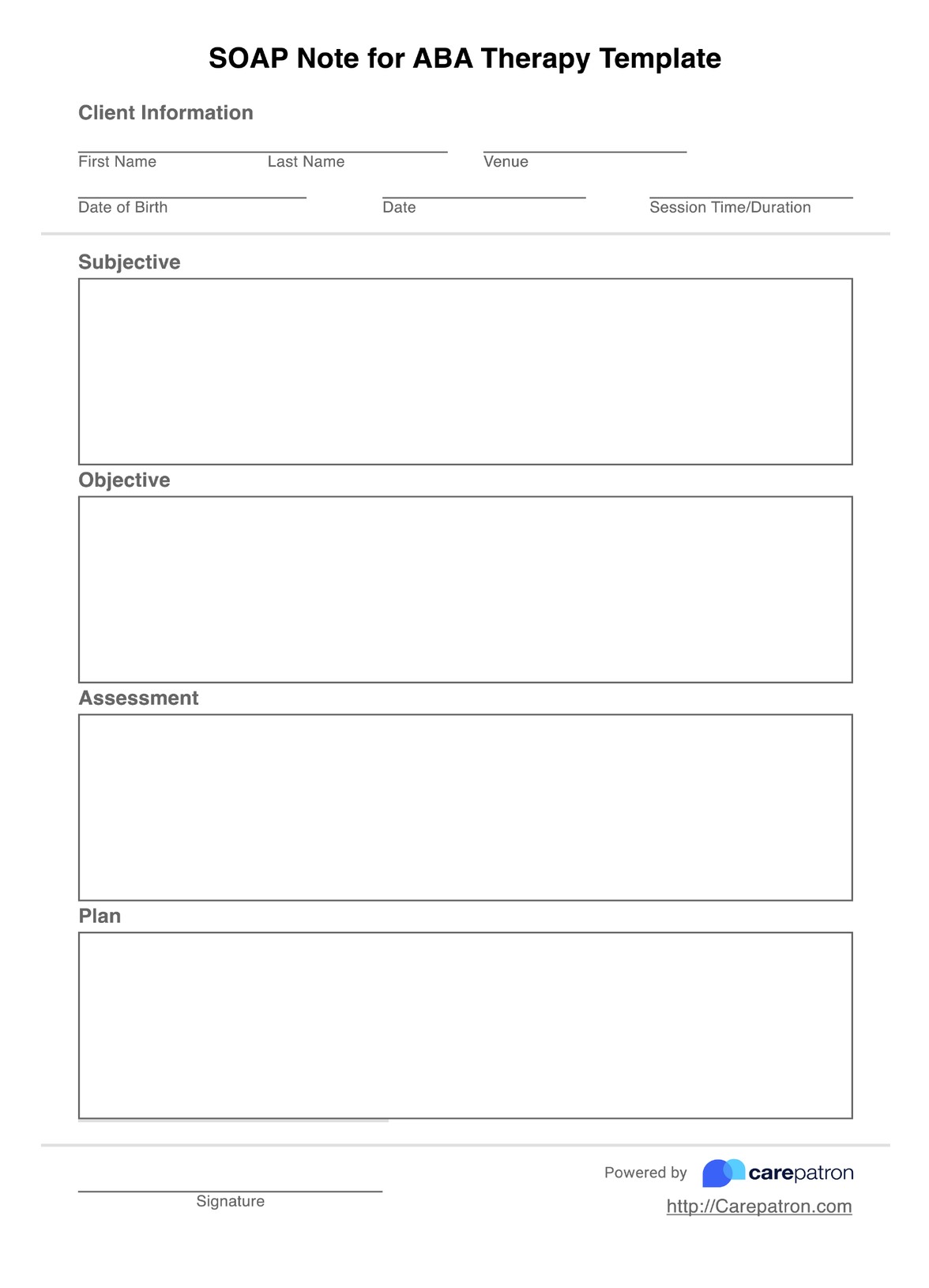
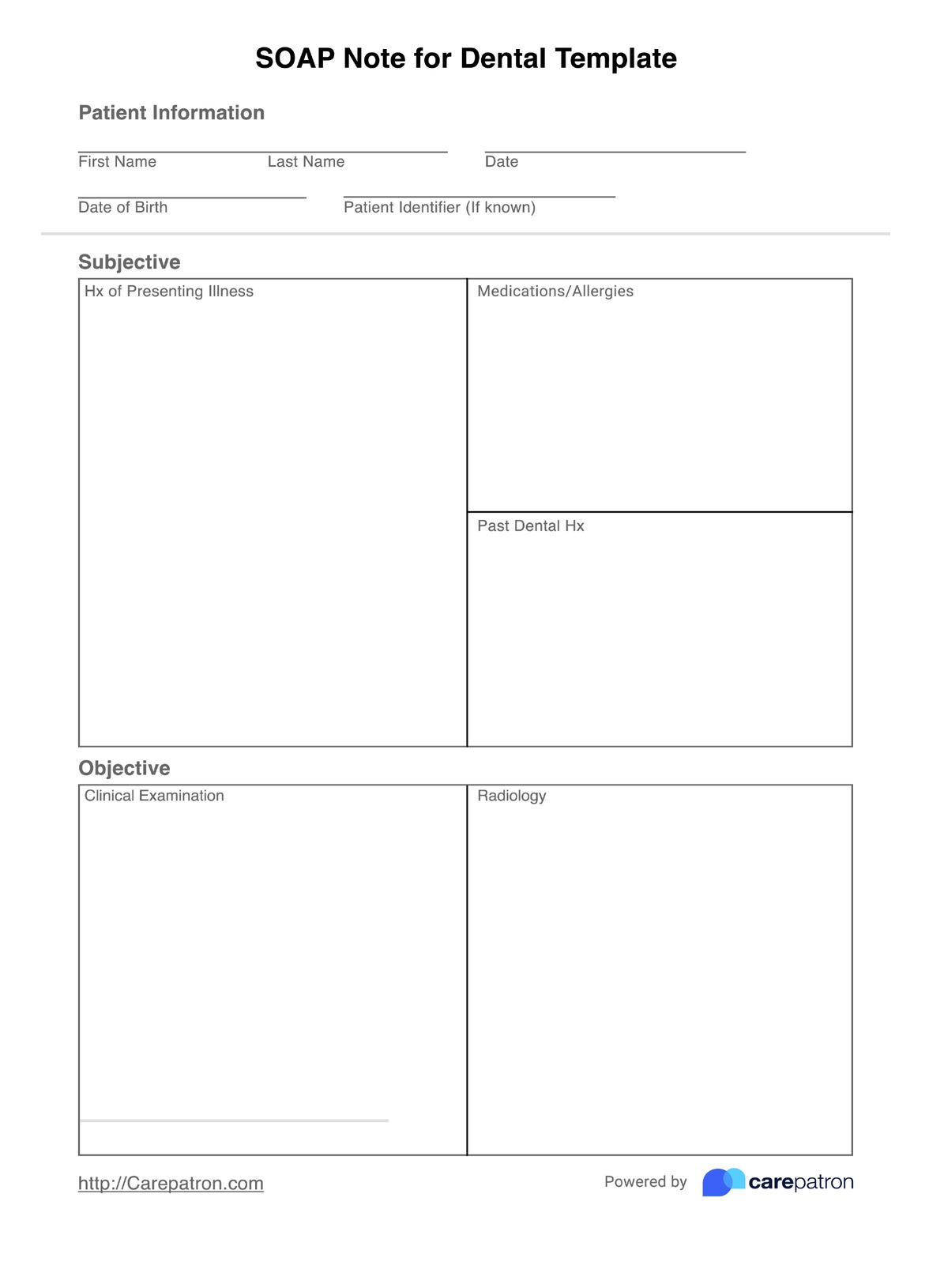
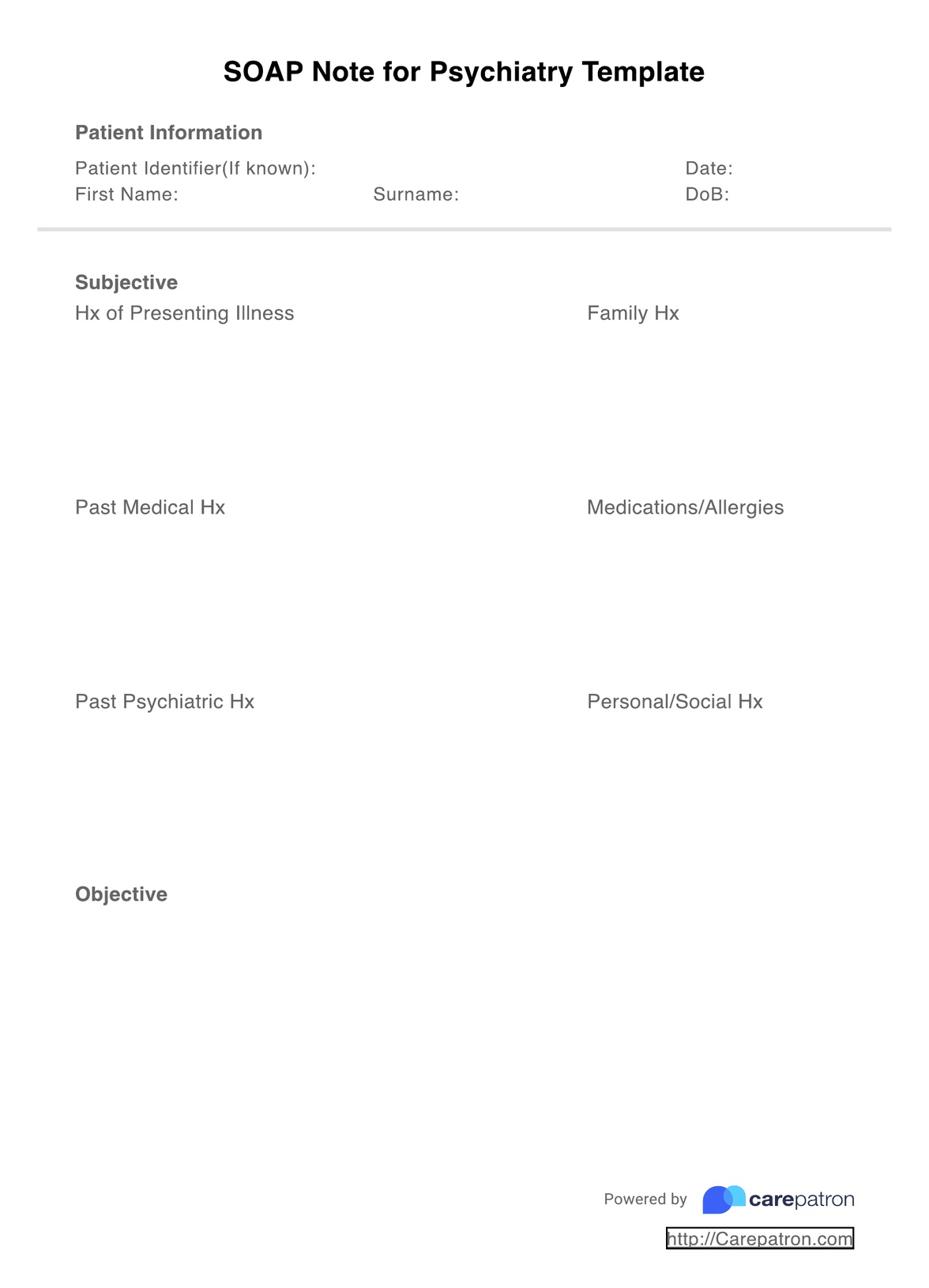
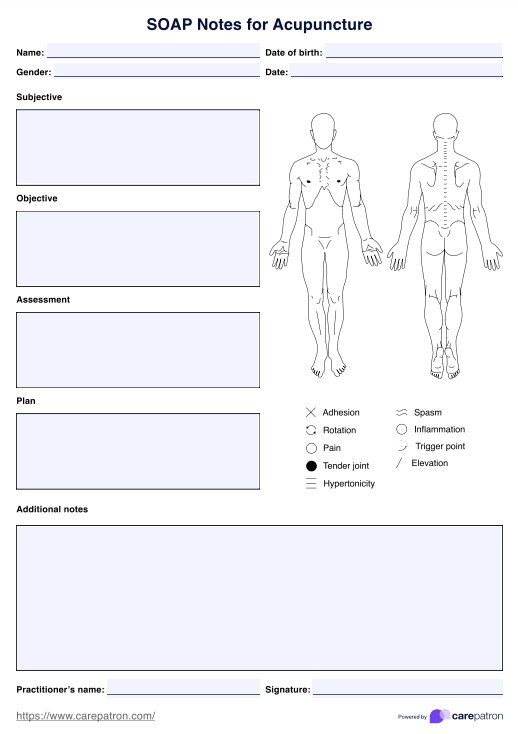
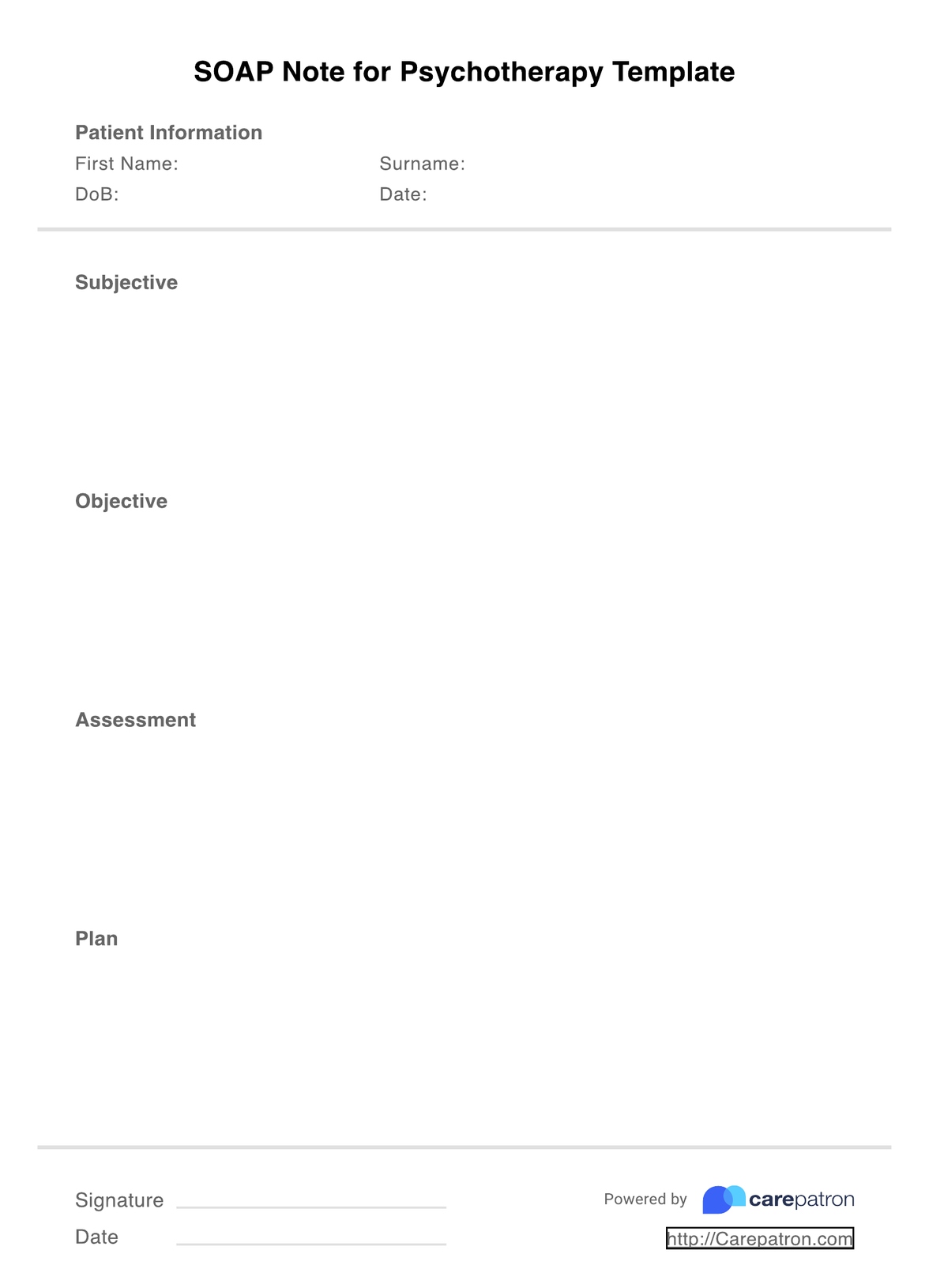
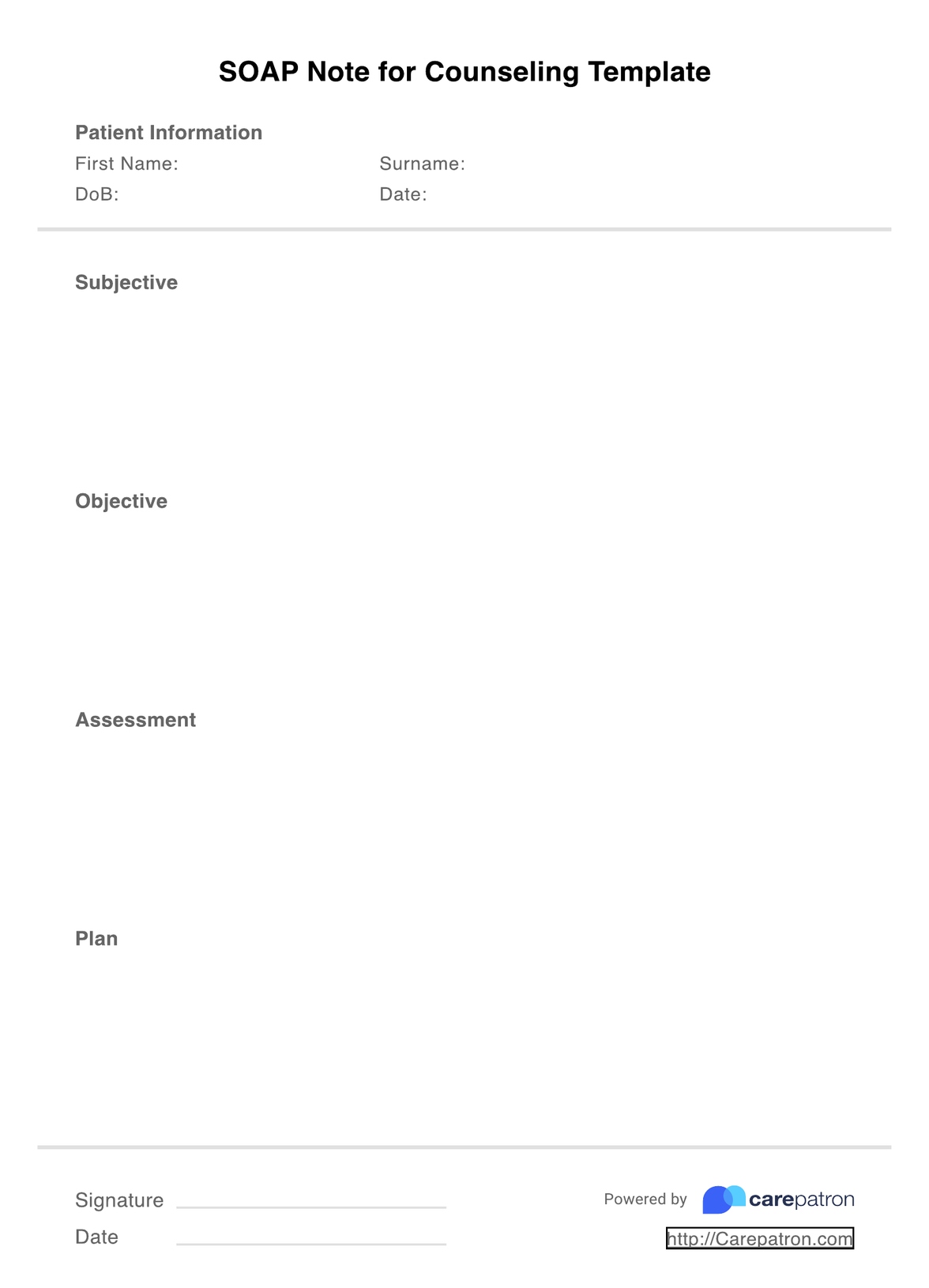
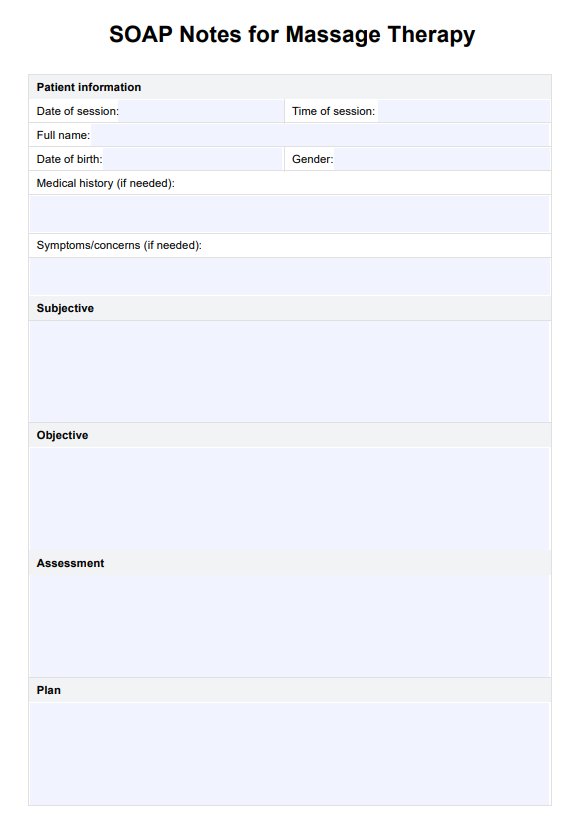
Download Example PDFOccupational Therapy SOAP Notes Templates
Check out these free SOAP Notes For Occupational Therapy Templates to help simplify your clinical notes.
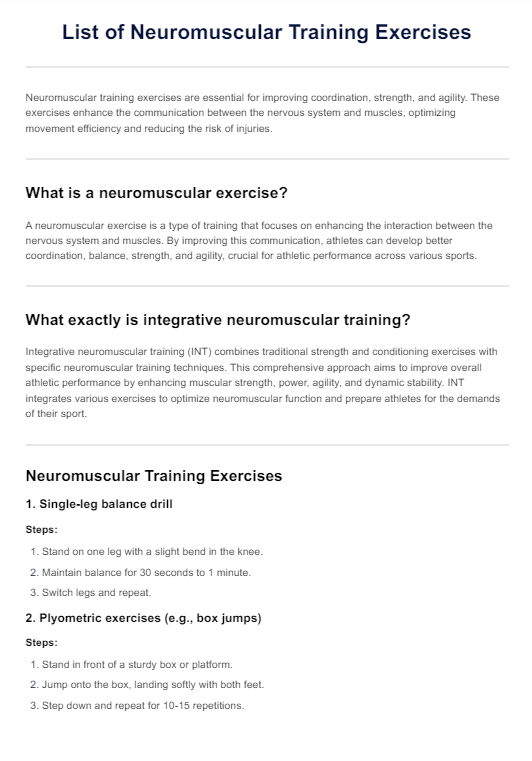
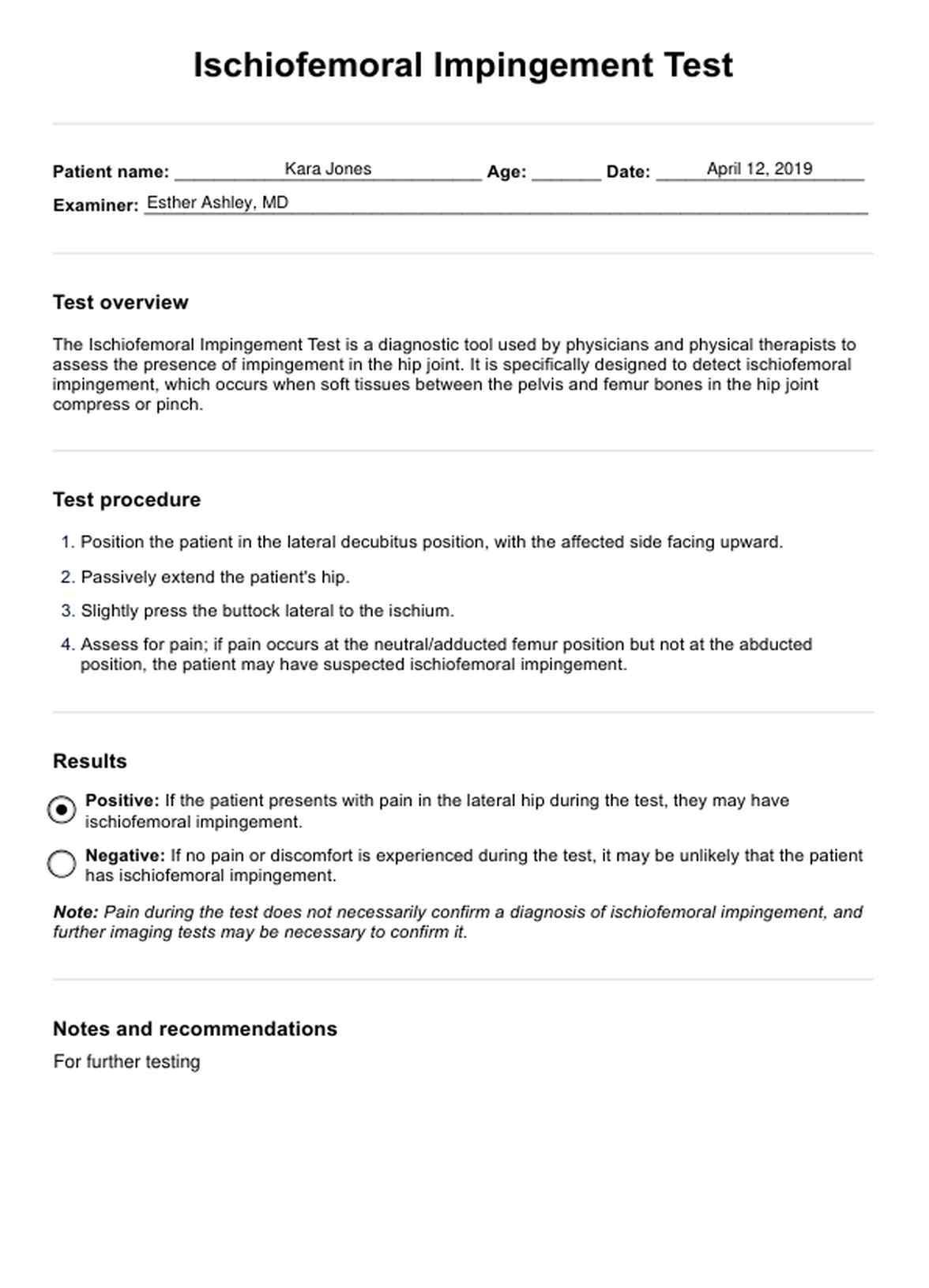
What should be included in an occupational therapy SOAP note?
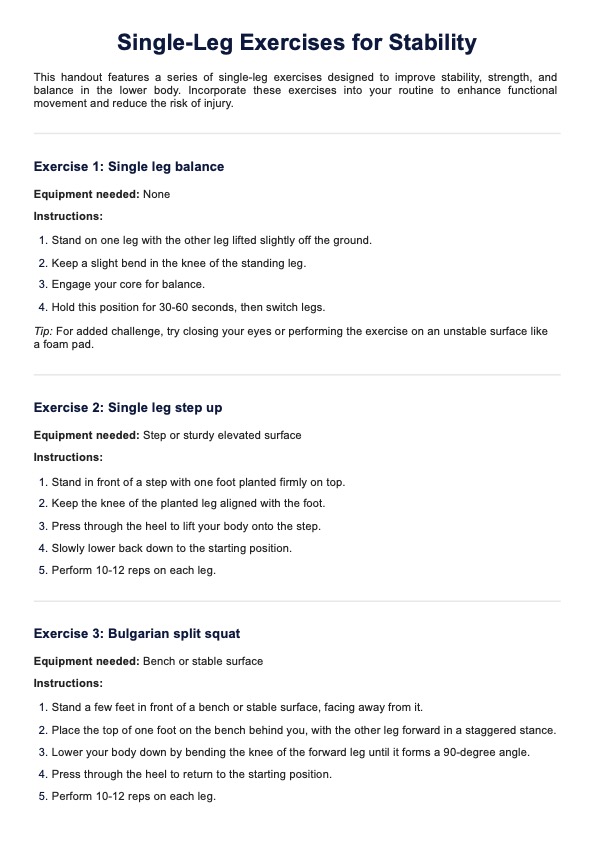
The following are included when writing SOAP notes for your occupational therapy practice:
Subjective
This is where you will write down information specific to your client, including their feelings, pain level, mood, and any new or progressing symptoms. Their priorities and goals for the session may also be relevant to this section and will help guide your session. Suppose this is your first session with your patient. In that case, you may record a more comprehensive history of your client, including why they are seeking occupational therapy services, present symptoms, medications, allergies, and past treatments.
Objective
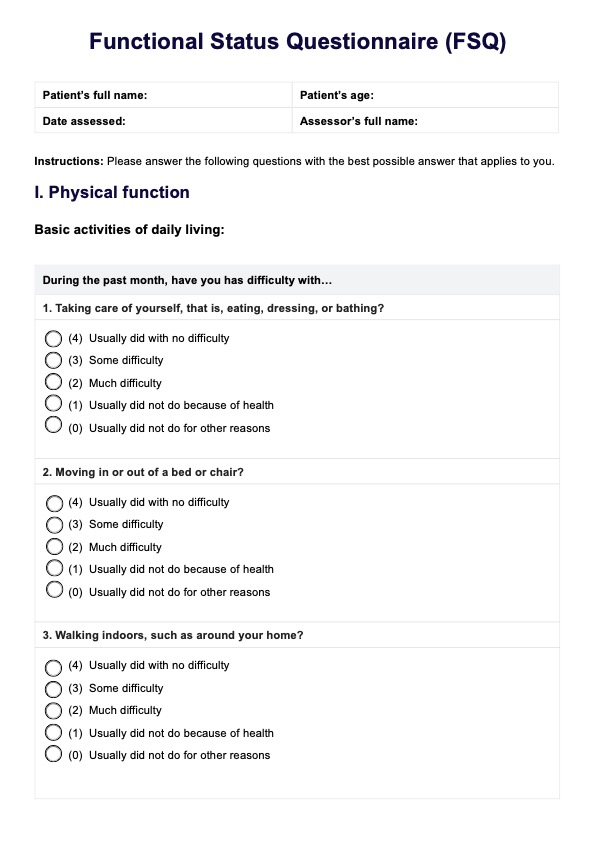
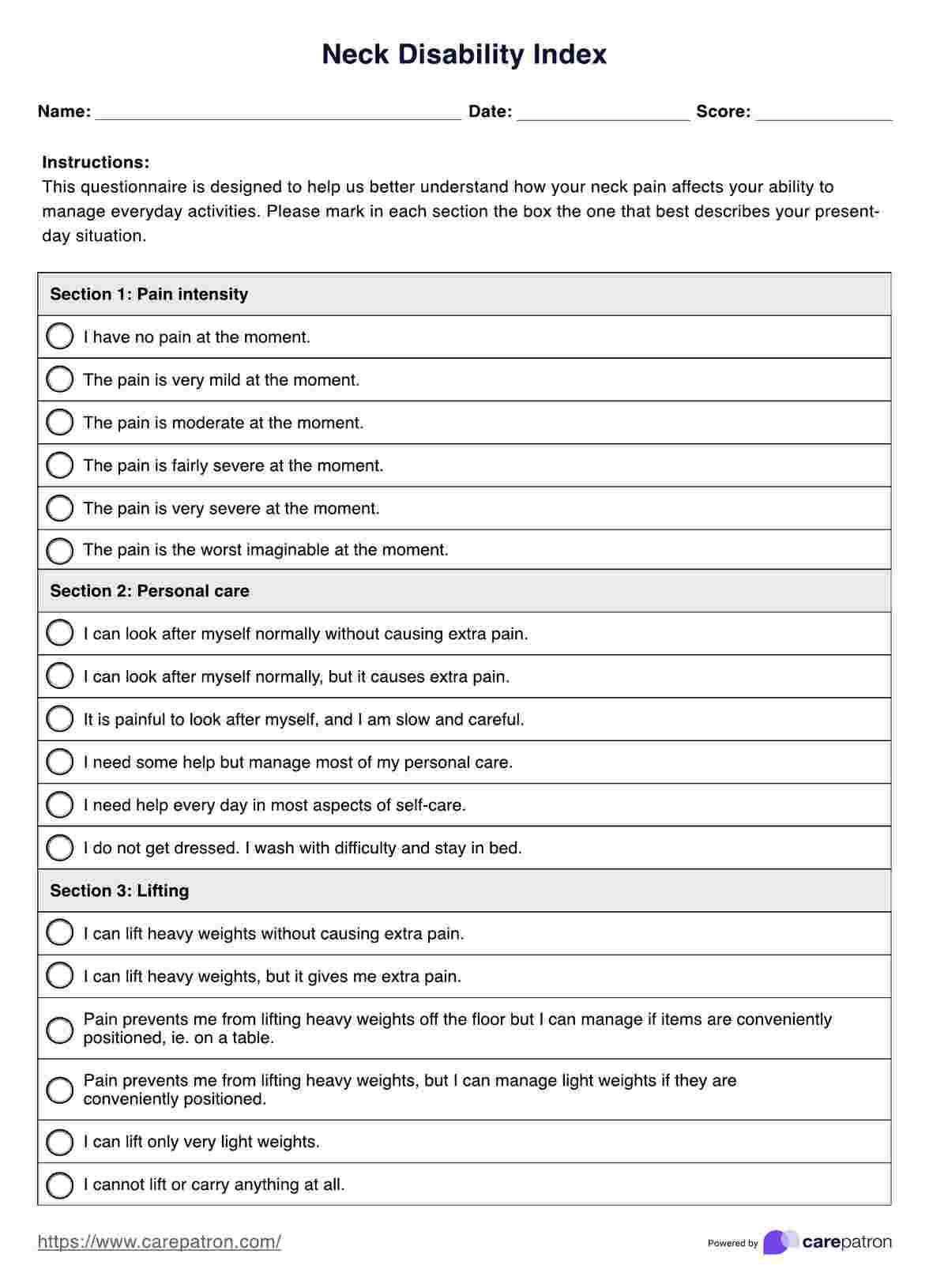
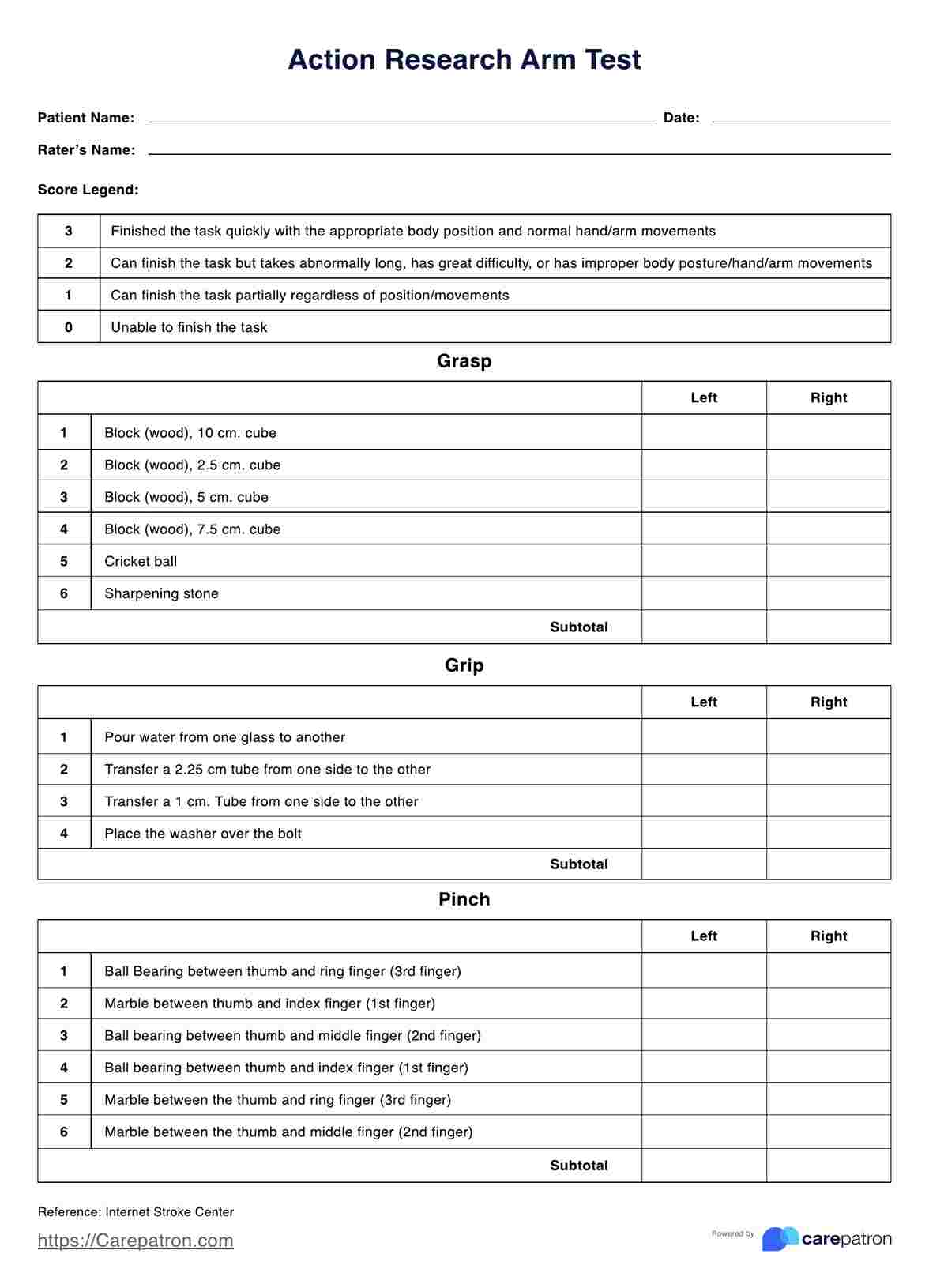
The objective section is for measurable or observable facts. Your client's response to a given task, their ability to complete a given task with or without assistance, results of a physical exam, or details you observe of their functioning may all be relevant here.
Assessment
In the assessment section, you can write down your professional opinion as an occupational therapist of the patient's current ability or performance in relevant tasks. This summary will be based on the subjective and objective information you gathered in the first two sections.
Plan
What are the next steps for your client? Include specific details like any resources you provided, any exercises or tasks you left them to practice between sessions, or anything you will be focusing on in particular in your client's following sessions.
How to use our OT SOAP note template
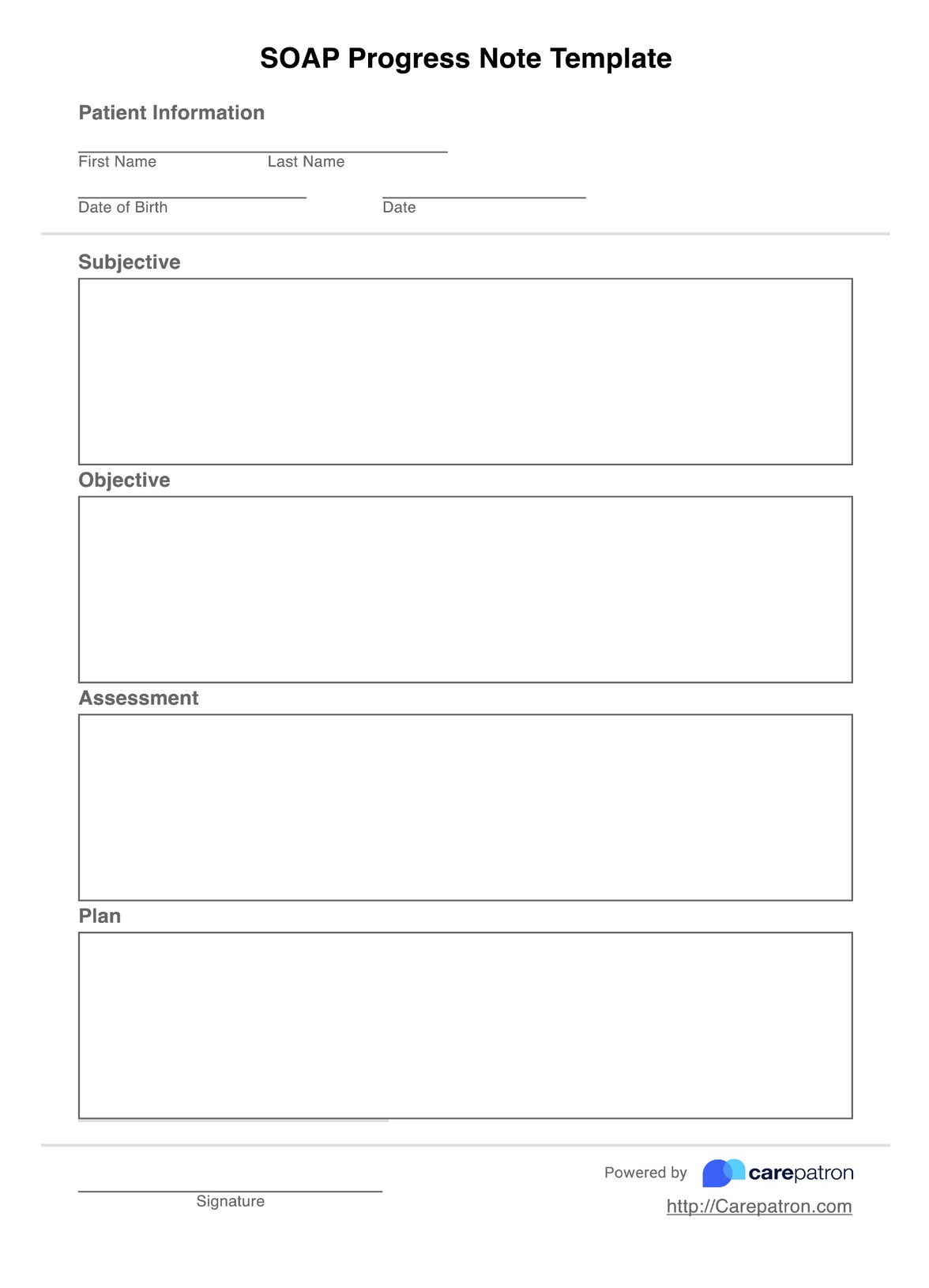
Our Occupational Therapy SOAP note template is designed to help practitioners in creating SOAP notes. Here's a step-by-step guide on how to use this resource in your practice:
Step 1: Access and customize the template
You can access the SOAP note template through your preferred digital platform or as a printable document. Take a moment to familiarize yourself with the layout and sections.
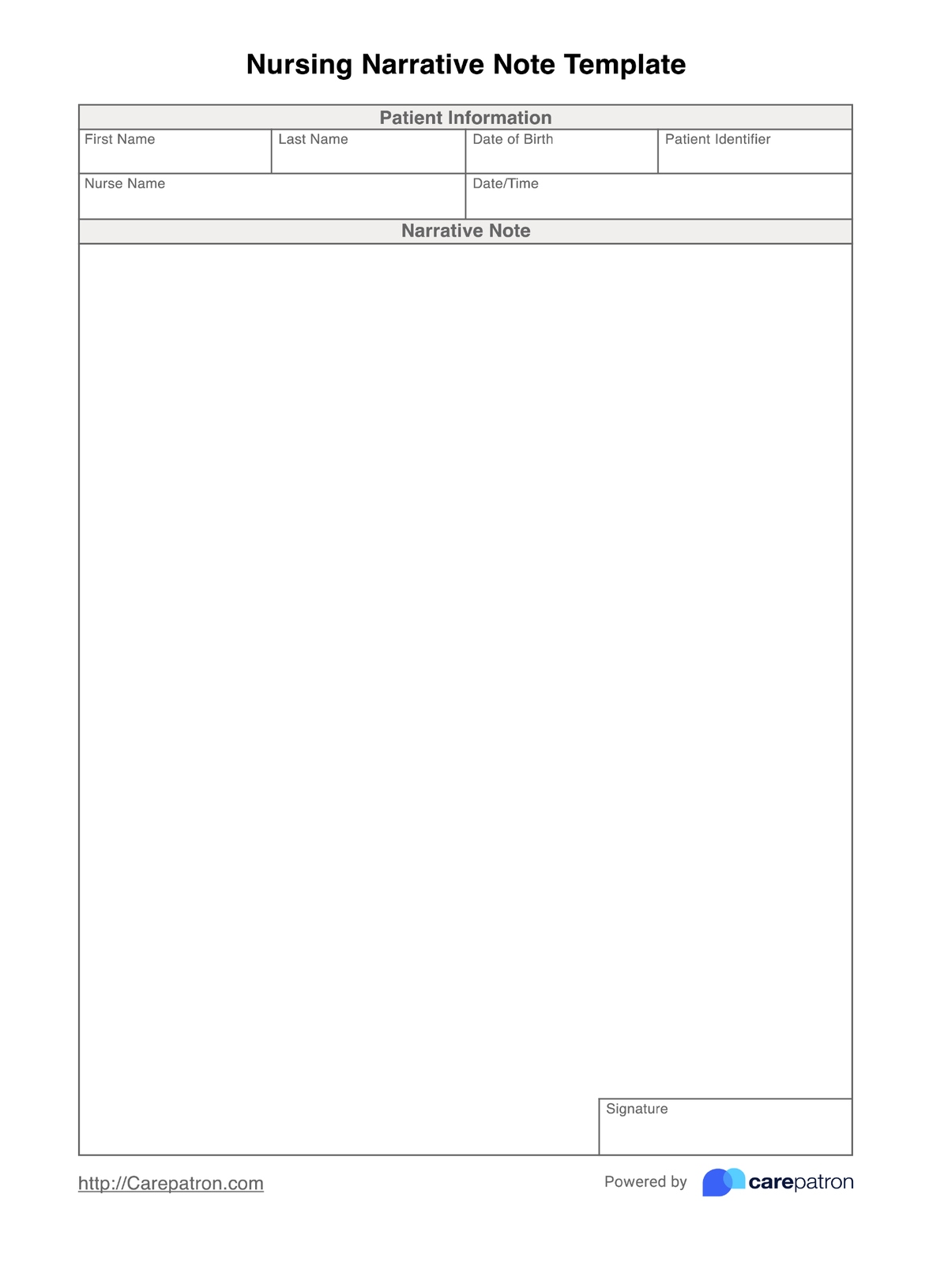
Step 2: Fill in the information
At the top of the template, input essential patient information such as name, date of birth, and medical record number. Include the date of the session, your name as the treating therapist, and any other relevant administrative details. This ensures easy identification and organization of notes.
Step 3: Complete each section
Work through each section of the SOAP note, filling in relevant information for the subjective and objective data, as well as the assessment and plan sections. Use clear, concise language and include specific, measurable data where possible.
Step 4: Review and refine
Before finalizing your note-taking process, review it for completeness, accuracy, and clarity. Ensure that you've included all necessary information and that your documentation aligns with your clinical reasoning and treatment goals. Make any necessary edits or additions to provide a comprehensive picture of the session and patient progress.
Step 5: Save and share if needed
Once you're satisfied with the note, save it securely in the patient's electronic health record or file it appropriately if using paper documentation. Share the information with relevant team members as needed, always adhering to privacy and confidentiality guidelines.
SOAP note example occupational therapy
Want to see what this specific SOAP Notes template looks like once it's completed? We've got you covered. This OT SOAP Notes example is a filled-out fictional occupational therapy SOAP note to serve as a guide in writing effective SOAP notes for occupational therapy sessions.
Download the sample occupational therapy SOAP Note template here.

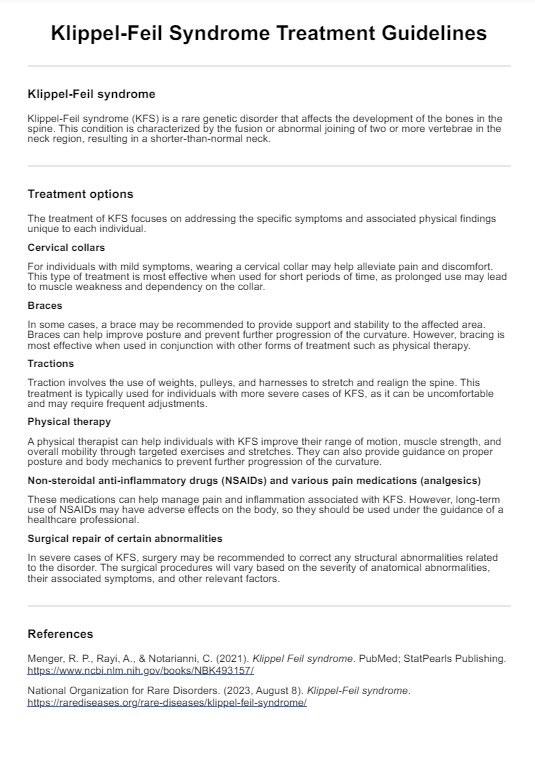
Who can use this OT SOAP note template?
This template is designed to help occupational therapists write therapy SOAP notes, but this would also be useful for occupational therapist assistants or other healthcare providers.
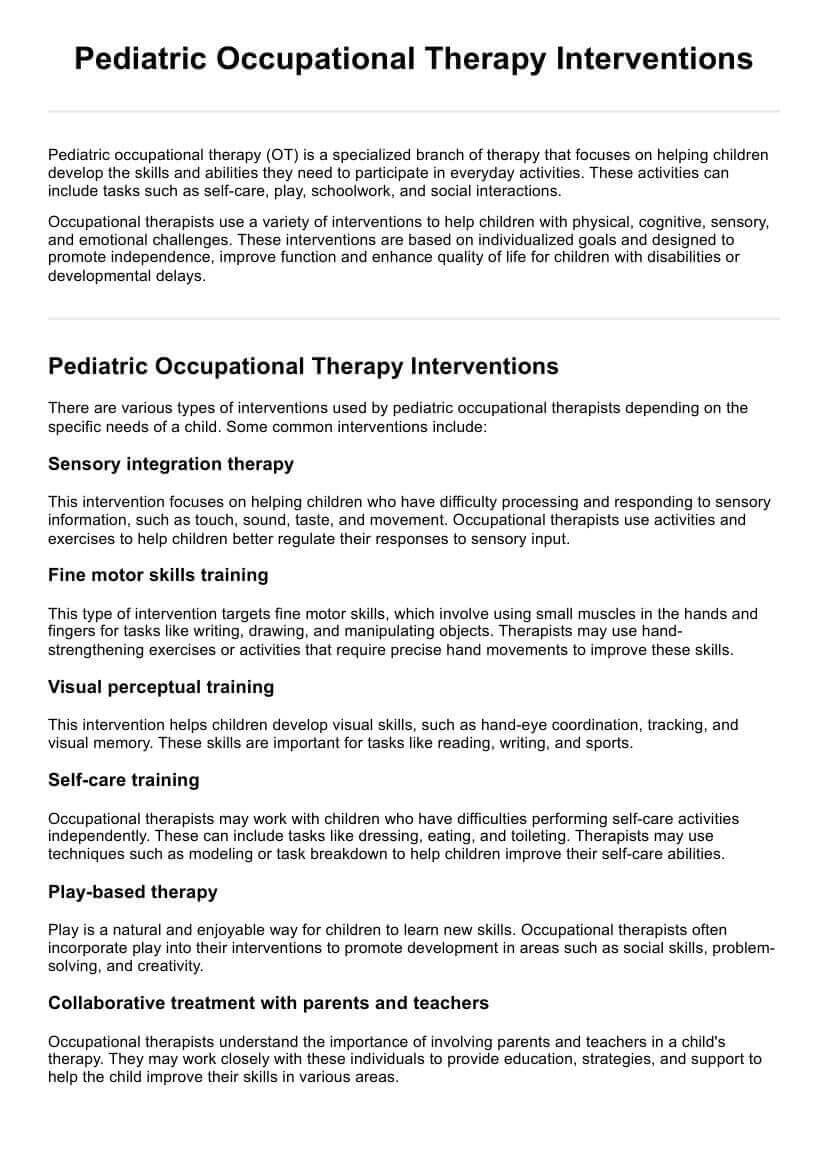
The field of occupational therapy is very broad, and we have designed our template to be used in general occupational therapy documentation. Occupational therapists who use this occupational therapy SOAP Notes template may specialize in the following:
- Brain injury occupational therapy
- Pediatric occupational therapy
- Hand therapy
- Physical rehabilitation following injury
- Stroke rehabilitation
- Skilled nursing facility procedures
Benefits of using the SOAP Notes For Occupational Therapy Template
The Occupational Therapy SOAP note template offers numerous advantages for practitioners, enhancing both the quality of documentation and overall patient care. Here are the key benefits of incorporating this template into clinical practice:
Standardization and consistency
Using a standardized template ensures that all essential elements of patient care are consistently documented. This uniformity makes it easier for other healthcare providers to quickly locate and understand important information, improving communication and continuity of care.
Time efficiency
A well-designed template streamlines the documentation process, allowing therapists to complete notes more quickly and efficiently. By providing a clear structure, the template reduces the time spent organizing thoughts and deciding what information to include.
Improved clinical reasoning
The SOAP format encourages a logical progression of thought, from gathering information (Subjective and Objective) to analysis (Assessment) and action (Plan). This structure supports clinical reasoning by prompting therapists to systematically consider all aspects of patient care. It helps identify patterns, track progress, and make informed decisions about treatment adjustments.
Enhanced goal tracking
The template facilitates consistent documentation of progress toward treatment goals. Therapists can easily track and update short-term and long-term goals by having a dedicated space for assessment and planning. This ongoing evaluation ensures that treatment remains focused and effective, promoting better patient outcomes.
Legal and ethical compliance
Comprehensive and accurate documentation is crucial for legal and ethical reasons. The SOAP note template helps ensure that all necessary elements are included in each note, reducing the risk of omitting important information. This thoroughness can be invaluable in case of audits, legal inquiries, or insurance reviews.
Why use Carepatron for occupational therapy SOAP notes?
Carepatron is a fully online practice managemsment software that makes it easy for you to access your patient's information on the go, whether that is at a client's home or from your home office!
Carepatron provides HIPAA-compliant electronic patient record software for you to store your patients' records, such as their occupational therapy SOAP Notes, as well as a whole suite of smart ways to save you time. Schedule your clients' occupational therapy appointments, manage payments and billing, and see your week at a glance—all from within Carepatron.
Our voice-to-text feature, client list system, integrated video call management, and customizable tag system give you greater control over managing your occupational therapy practice.
Experience these features and more when you choose Carepatron as your private practice partner. Sign up for a free trial!

Commonly asked questions
Effective SOAP notes in occupational therapy should be concise, objective, and focused on the patient's progress and functional outcomes. The note should clearly document the patient's subjective report, the occupational therapist's objective observations, the therapist's clinical assessment, and the plan for ongoing treatment.
Using SOAP notes in occupational therapy can help improve communication among healthcare providers, enhance patient care, and facilitate information sharing. They also provide a structured format for documenting patient progress and treatment outcomes, which can help with billing and reimbursement.
A SOAP note in occupational therapy typically includes the following components: Subjective (patient's report), Objective (therapist's observations), Assessment (therapist's clinical assessment), and Plan (plan for ongoing treatment).