Morley Test
Download Carepatron's free PDF of the Morley Test along with an example to practice and improve your skills. Learn more about this widely used test.


What is thoracic outlet syndrome?
Thoracic outlet syndrome (TOS) is a condition characterized by the compression of the nerves, arteries, or veins in the passageway from the lower neck to the armpit. This area, known as the thoracic outlet, houses critical structures, including the brachial plexus, which can be affected by this syndrome. When the brachial plexus is compressed, it often leads to symptoms such as arm pain, typical localized paresthesia, and weakness in the upper extremity. Clinical tests like the Eden's Test, Adsons Test, and Wright Test are commonly used to diagnose TOS.
The causes of TOS can range from physical trauma, repetitive movements, anatomical defects, or even a palpable hard mass. The syndrome is often associated with other conditions, such as cervical radiculopathy, where nerve roots in the cervical spine are compressed, leading to similar symptoms. The brachial plexus compression test and Morley's compression test are instrumental in identifying the presence of a true structural lesion that might be causing the symptoms.
TOS can affect the median nerve, ulnar nerve, and ulnar nerves, leading to numbness and tingling in the hands and fingers. These symptoms can sometimes be confused with other conditions, but thorough clinical evaluation and appropriate diagnostic tests help in distinguishing TOS from other potential issues.
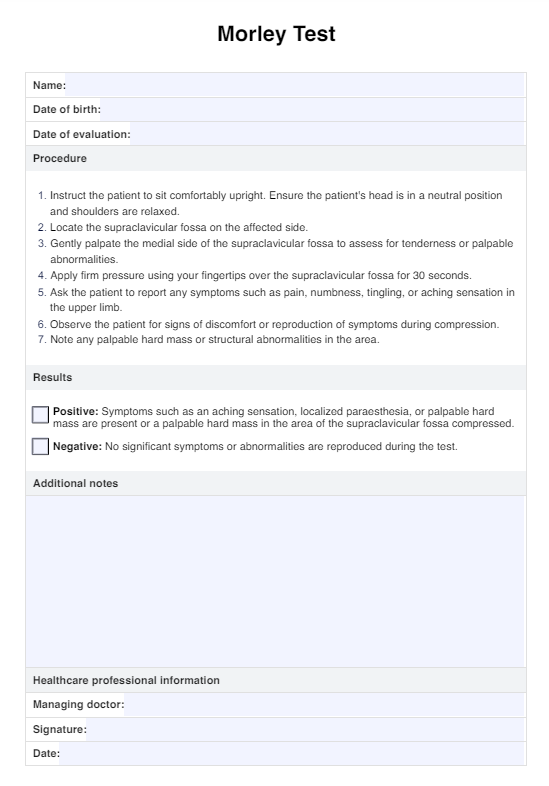
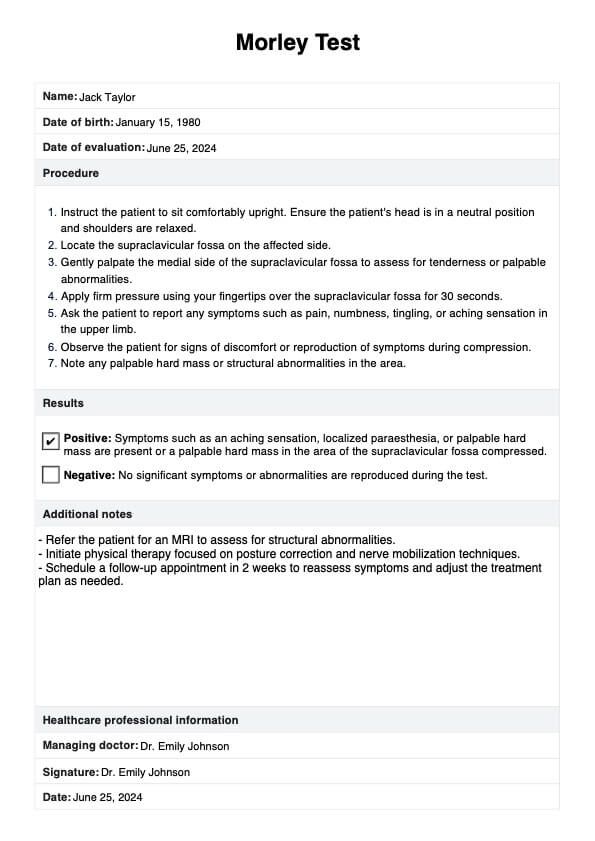
Morley Test Template
Morley Test Example
What is the Morley Test?
The Morley Test, also known as Morley's compression test, is a clinical assessment used to diagnose thoracic outlet syndrome. It specifically evaluates for compression of the brachial plexus, which can lead to symptoms such as aching sensations and numbness in the upper limb.
This test is performed alongside other evaluations like the brachial plexus tension test, upper limb tension test, and brachial plexus compression test.
The goal is to identify a true structural lesion, such as a palpable hard mass, that may be compressing nerves like the ulnar nerve and median nerve. It helps differentiate thoracic outlet syndrome from conditions like cervical radiculopathy.
How to perform the Morley Test?
Below are the steps to perform the Morley Test, which should be conducted carefully to ensure accurate results and patient comfort.
Step 1: Position the patient
Have the patient sit or stand in a comfortable position. Ensure their upper limb is relaxed and that they are at ease to avoid any involuntary muscle tension that could affect the results.
Step 2: Palpate the supraclavicular fossa
Locate the supraclavicular fossa, which is the depression above the clavicle. Gently palpate this area to identify any tenderness or a palpable hard mass that might indicate compression of the neurovascular bundle, including the brachial plexus and subclavian vessels.
Step 3: Apply pressure
Using your fingers, apply firm but gentle pressure on the medial side of the supraclavicular fossa for about 30 seconds. This is where the brachial plexus compression test comes into play. Monitor the patient for any signs of discomfort or an aching sensation.
Step 4: Observe symptoms
Ask the patient to describe any symptoms they experience during the test. Pay close attention to signs of pain, numbness, or tingling in the upper limb, which could indicate compression of the brachial plexus, median nerve, or other structures.
Step 5: Assess for nerve compression
Evaluate the responses and symptoms to determine if there is evidence of nerve compression. Compare findings with other tests, such as the brachial plexus compression and tension tests, to confirm the diagnosis.
Results and Interpretations of the Morley Test
The Morley Test is a clinical assessment used to diagnose thoracic outlet syndrome (TOS) by evaluating compression of the brachial plexus and neurovascular structures within the supraclavicular fossa.
- Positive result: A positive result occurs when the patient experiences symptoms such as an aching sensation, typical localized paraesthesia, or the presence of a palpable hard mass in the supraclavicular fossa upon applying pressure to the medial side.
- Negative result: A negative result suggests the absence of significant compression or tenderness in the supraclavicular region at that time. However, it's important to note that a negative result does not completely rule out TOS, as symptoms can be intermittent or may require further diagnostic evaluation with additional tests like the brachial plexus compression test to confirm or refute the diagnosis.
Treatment of thoracic outlet syndrome
Initially, conservative approaches are typically recommended, which may include physical therapy focused on stretching and strengthening exercises to improve posture and alleviate compression of the brachial plexus and subclavian vessels. Lifestyle modifications, such as avoiding activities that exacerbate symptoms or improving ergonomics, can also be beneficial.
In cases where conservative measures do not provide sufficient relief, more invasive treatments may be considered. This could involve corticosteroid injections to reduce inflammation around compressed nerves, or surgical intervention to release the compression. Surgical options range from removing a portion of the first rib (thoracic outlet decompression) to addressing any anatomical abnormalities contributing to nerve compression.
Commonly asked questions
The best test to assess thoracic outlet syndrome (TOS) is typically a combination of clinical maneuvers, including the Adson's test, Wright's test, and Roos test, which evaluate for compression of the brachial plexus and subclavian vessels.
Electromyography (EMG) and nerve conduction studies (NCS) are commonly used to confirm brachial plexus injuries by assessing nerve function and detecting abnormalities in electrical activity along the nerve pathways.
To test for thoracic outlet syndrome, perform clinical maneuvers such as Adson's test, Wright's test, and Roos test. These assess for compression of the brachial plexus and subclavian vessels in the supraclavicular region, typically reproducing symptoms like pain, numbness, or tingling in the upper limb.