Reverse Lachman Test
Discover how to perform and interpret the Reverse Lachman Test to diagnose PCL tears. Download our free template and enhance your physical therapy practice today!


What is a posterior cruciate ligament tear?
A posterior cruciate ligament (PCL) tear is an injury to one of the critical knee ligaments stabilizing the knee joint. The PCL is located at the back of the knee and connects the thigh bone (femur) to the shin bone (tibia). It prevents the tibia from moving too far backward relative to the femur, which is crucial in maintaining knee stability. PCL tears are less common than anterior cruciate ligament (ACL) tears and typically occur due to a direct blow to the front of the knee, often during sports or motor vehicle accidents.
Symptoms of PCL tears
Symptoms of a PCL tear can vary depending on the severity of the injury. Common signs include:
- Immediate pain at the time of injury, often localized to the back of the knee. The pain may be mild initially but can worsen over time.
- Swelling in the knee that develops within a few hours of the injury. This swelling may be accompanied by stiffness.
- A feeling of instability or "giving way" in the knee, particularly when walking or bearing weight. This is due to the compromised function of the PCL in stabilizing the knee.
- Difficulty in fully extending or bending the knee. The knee may feel stiff and restricted in movement.
- Bruising around the knee area may appear a few days after the injury.
- Tenderness at the back of the knee, where the PCL is located, is often noted during a physical examination.
Causes of PCL tears
A forceful impact or trauma to the knee typically causes PCL tears. Common causes of rupture include:
- A strong impact to the front of the knee, such as hitting the dashboard in a car accident or falling onto a bent knee, can push the tibia backward and tear the PCL.
- Contact sports like football, soccer, and rugby often involve collisions and falls that can result in PCL injuries. Athletes who perform actions like landing awkwardly or hyperextending the knee are at higher risk.
- Falling directly onto a bent knee can generate enough force to tear the PCL. This is common in activities with a risk of falling, such as skiing or gymnastics.
- Hyperextending the knee, where it is forced to bend backward beyond its normal range, can stretch and tear the PCL.
- A severe knee twist, especially when the foot is planted and the body rotates, can also lead to a PCL tear.
A PCL tear can result in a PCL-deficient knee, which becomes unstable and may lead to recurrent disability and reduced activity effectiveness, especially in athletes.
Reverse Lachman Test Template
Reverse Lachman Test Example
What is the Reverse Lachman Test?
The Reverse Lachman Test is a clinical examination used to assess the integrity of the PCL in the knee. It is one of several clinical tests that are beneficial when patients experience discomfort during knee flexion, making other tests, such as the Posterior Drawer Test and anterior drawer sign test, challenging to perform. The test helps diagnose PCL tears by evaluating the posterior translation of the tibia relative to the femur when the knee is slightly flexed.
How is this test conducted?
To perform the Reverse Lachman Test , the patient lies supine on an examination table with the knee flexed approximately 30 degrees. The examiner can stabilize this position by placing the patient's knee under the patient’s knee, ensuring it remains in the correct flexed position.
Next, the examiner places one hand on the femur from the lateral side and the other on the tibia from the medial side, close to the joint line. This hand placement is crucial to avoid angulation and ensure proper translation during the test. The tibia must be anatomically reduced, meaning it is positioned correctly relative to the femur, with neutral rotation to avoid recruiting secondary stabilizers that could affect the test's accuracy.
Finally, the examiner applies a posteriorly directed force to the tibia while feeling for the end feel and the degree of posterior translation. A soft or absent end feel and increased posterior translation compared to the unaffected side typically indicate a positive result, suggesting a PCL tear. This systematic approach ensures an accurate assessment of the PCL, aiding in the diagnosis and subsequent treatment planning for knee injuries.
How are the results interpreted?
Interpreting the results of the Reverse Lachman Test involves assessing the end feel and the degree of anterior translation compared to the unaffected side, as well as the posterior translation of the leg at the tibia:
Positive test
A soft or absent end feel and an increased posterior translation of the tibia compared to the unaffected side indicate a PCL tear.
Grading the injury
The severity of a PCL tear is categorized into three grades based on the amount of posterior tibial translation observed during the test:
- Grade 1: 0-5 mm of posterior translation, with the tibial plateau remaining anterior to the femoral condyle.
- Grade 2: 6-10 mm of posterior translation, with the tibial plateau being flush with the femoral condyle.
- Grade 3: More than 10 mm of posterior translation, with the tibial plateau translating posteriorly to the femoral condyle.
If the increased translation is noticed with the Reverse Lachman Test but not with the Posterior Drawer Test, it might indicate an injury to the posterior lateral corner (PLC). The Dial Test can be performed to differentiate between PLC and PCL injuries. The grading of PCL injuries can be compared to assessing an ACL-deficient knee, where tests like the Lachman test and instruments such as the KT-1000 are used to measure anterior tibial translation.
Next steps after conducting this test
After performing the Reverse Lachman Test and interpreting the results, several steps should follow to ensure accurate diagnosis and appropriate treatment:
- Confirmatory imaging: If a PCL tear is suspected, further imaging studies such as MRI should be ordered to confirm the diagnosis and assess the extent of the injury.
- Evaluate for additional injuries: Check for associated injuries, such as damage to the posterior lateral corner, anterior cruciate ligament injury, or other ligaments, which might influence the treatment plan.
- Develop a treatment plan: Based on the severity of the PCL tear and any associated injuries, develop a treatment plan. For minor tears, non-surgical management such as physical therapy, bracing, and activity modification may be sufficient. Severe or complex injuries may require surgical repair or reconstruction of the PCL and any associated damaged structures.
- Rehabilitation: Implement a rehabilitation program to restore knee stability, strength, and range of motion. Physical therapy plays a crucial role in recovery.
- Follow-up: Schedule follow-up appointments to monitor the patient’s progress, adjust the treatment plan as necessary, and ensure proper healing and return to function.
How to use our Reverse Lachman Test template
The Reverse Lachman Test template is designed to help healthcare professionals assess and manage patients with suspected PCL tears. To use the template effectively, follow these steps.
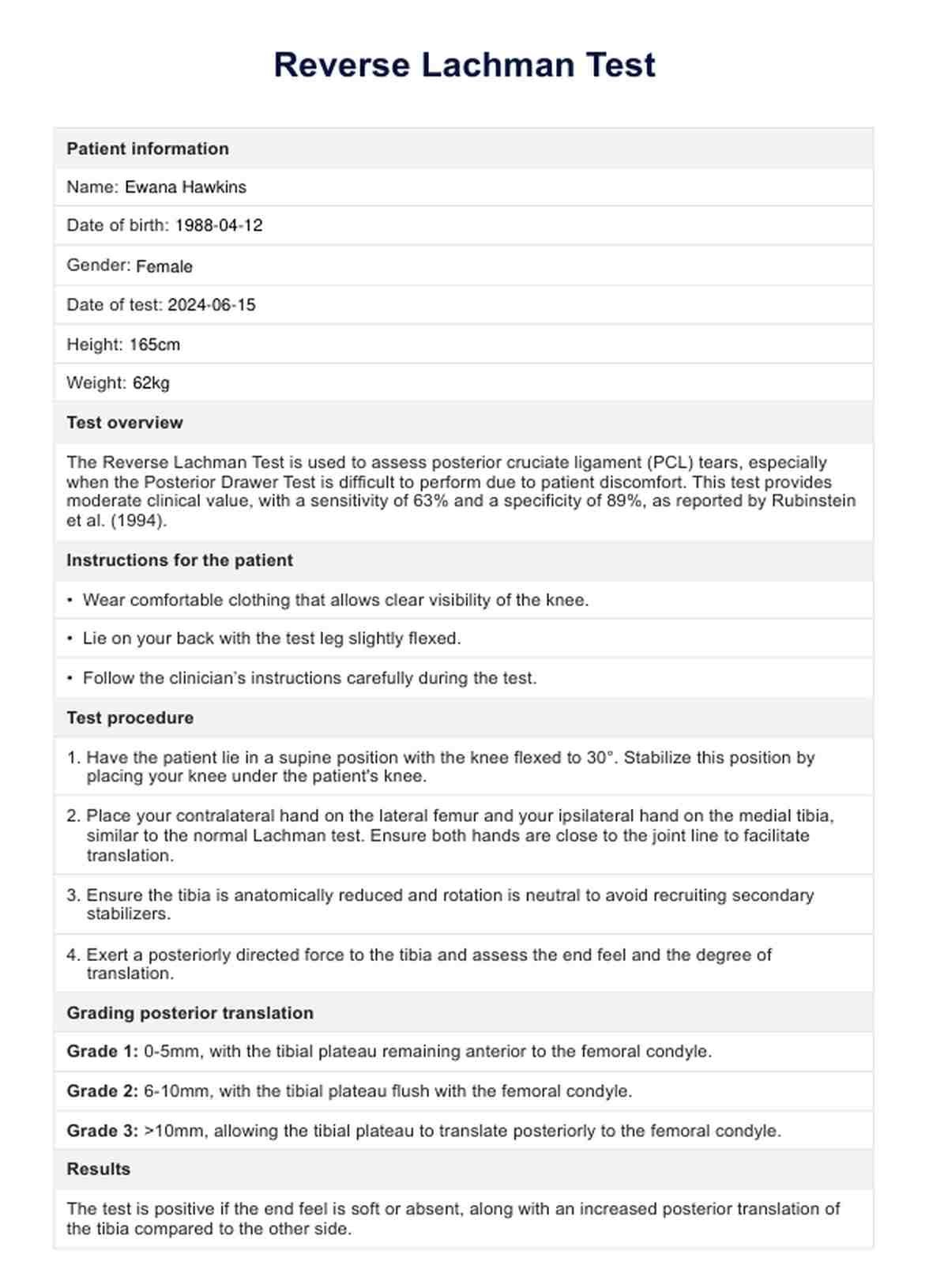
Step 1: Gather patient information and explain the test
Begin by collecting the patient's information, including name, date of birth, gender, date of test, height, and weight. Provide a brief overview of the Reverse Lachman Test, explaining its purpose and what the patient can expect during the procedure.
Step 2: Prepare and position the patient
Instruct the patient to wear comfortable clothing that allows clear visibility of the knee. Have the patient lie in a supine position with the knee flexed to 30 degrees, stabilizing this position by placing your knee under the knee.
Step 3: Perform the test and record observations
Place your contralateral hand on the lateral femur and your ipsilateral hand on the medial tibia, close to the joint line. Ensure the tibia is anatomically reduced and rotation is neutral. Exert a posteriorly directed force to the tibia, assessing the end feel and degree of anterior translation. Record these observations in the template, noting whether the end feel is soft, absent, or firm and the degree of posterior translation.
Step 4: Interpret results and document measurements
Determine the grade of posterior translation based on your observations. If there is increased translation with the Reverse Lachman Test but not with the Posterior Drawer Test, consider the possibility of a posterior lateral corner injury and perform the Dial Test if necessary. Document these measurements and interpretations in the template. Additionally, the possibility of a torn ACL should be considered when interpreting results.
Step 5: Complete the healthcare practitioner’s notes and sign the template
Include additional details, observations, patient feedback, and recommendations or follow-up plans in the healthcare practitioner’s notes section. Ensure the healthcare practitioner fills out their name, signs the template, and dates it.
By following these steps, healthcare professionals can effectively use the Reverse Lachman Test template to assess and manage patients with suspected PCL tears, ensuring accurate diagnosis and appropriate treatment.
Commonly asked questions
The Reverse Lachman Test is used to assess the integrity of the posterior cruciate ligament in the knee. It helps diagnose PCL tears by evaluating the posterior translation of the tibia relative to the femur when the knee is slightly flexed.
The Reverse Lachman Test assesses the PCL, while the standard Lachman Test primarily evaluates the anterior cruciate ligament. The positioning and direction of force applied during the tests differ to target these specific ligaments.
A positive Reverse Lachman Test indicates a potential tear in the posterior cruciate ligament. This is identified by a soft or absent end feel and increased posterior translation of the tibia compared to the unaffected side.