Exercises for Gluteal Tendinopathy Handout
Help your patients alleviate pain around the hips and buttocks, and improve strength and mobility. Use our Gluteal Tendinopathy Exercises PDF today.


What is gluteal tendinopathy?
Gluteal tendinopathy, often referred to as greater trochanteric pain syndrome, is a common cause of lateral hip pain. It primarily affects the gluteal tendons, which are the thick bands of tissue that connect the gluteal muscles (gluteus maximus, gluteus medius, and gluteus minimus) to the thigh bone. This condition typically manifests as pain and tenderness around the greater trochanter, the bony prominence outside the hip. The gluteus medius muscle, in particular, is often implicated in this condition, as it plays a crucial role in stabilizing the pelvis during single-leg activities.
Gluteal tendinopathy often develops due to repetitive stress on the gluteal tendons, particularly during activities such as running, stair climbing, or cycling. Muscle imbalances or weakness in the hip and pelvic muscles, especially the gluteus medius, can increase strain on the tendons, leading to injury. Additionally, poor biomechanics, direct trauma, or changes in gait patterns due to aging or pregnancy can contribute to the development of this condition.
Gluteal tendinopathy typically presents with lateral hip pain localized around the greater trochanter. This pain, often described as a deep ache, tends to worsen with activities involving the hip abductors, such as walking, stair climbing, or lying on the affected side. Other symptoms include stiffness, a limited range of motion, and occasional swelling around the hip joint. These symptoms often develop gradually and may progress with repetitive activities or prolonged physical exertion.
Exercises for Gluteal Tendinopathy Handout Template
Exercises for Gluteal Tendinopathy Handout Example
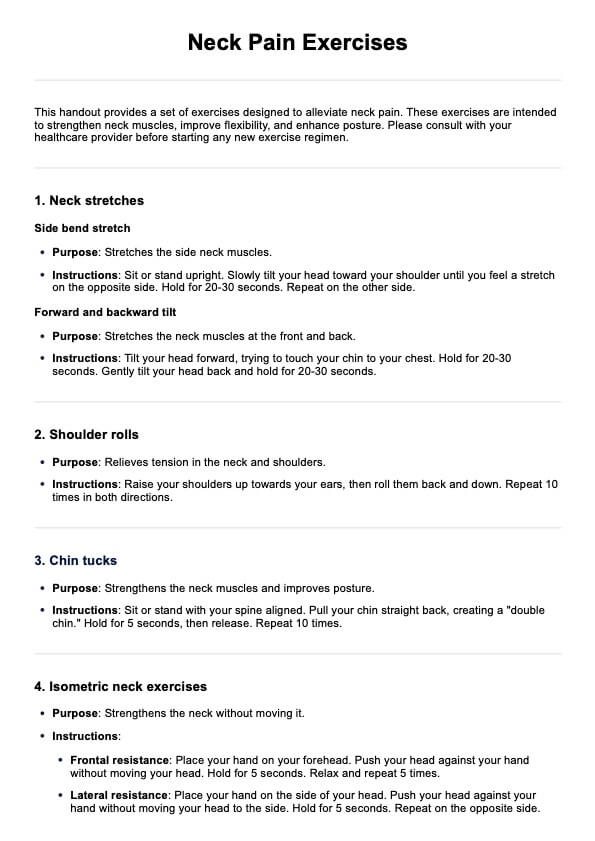
How to use our Exercises for Gluteal Tendinopathy Handout
Our Exercises for Gluteal Tendinopathy Handout provides clear instructions and visuals to guide healthcare professionals and patients through exercises that target the affected muscles. Here’s how you can integrate it effectively into your practice:
Step 1: Access the template
Click the "Use template" button to access a customizable version that allows you to modify, print, and fill out the handout. Alternatively, click the "Download" button to save a fillable and printable PDF version.
Step 2: Distribute the handout
Introduce the handout to your patient, explaining its purpose and the benefits of consistent exercise. You can either give it to them as part of an in-person consultation or share it digitally for remote access.
Step 3: Guide the patient through the exercises
Demonstrate each exercise, ensuring proper form and technique. Teach the patient how to adjust intensity and repetitions according to their progress. Use this opportunity to empower the patient to use the handout independently, fostering engagement in their recovery.
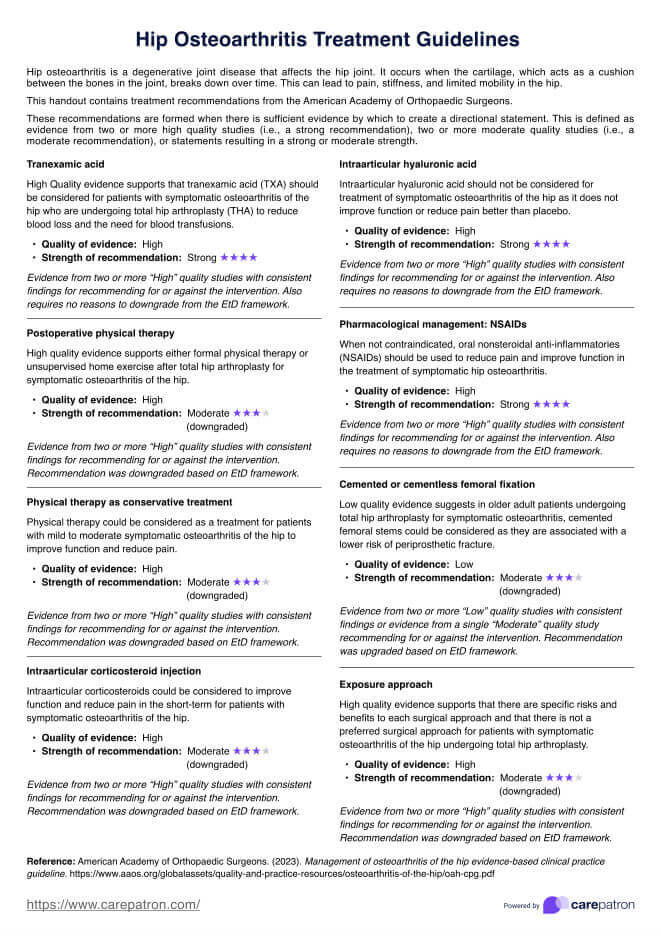
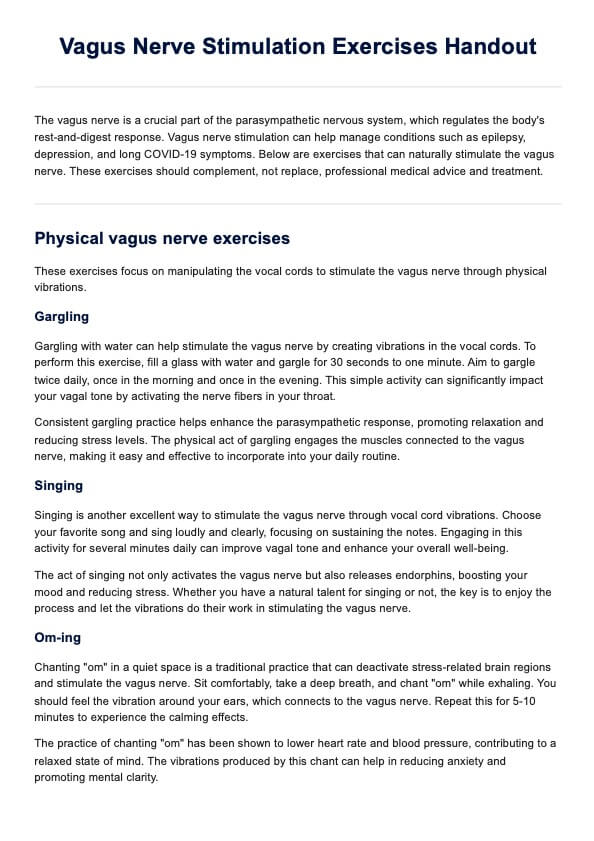
Exercises for Gluteal Tendinopathy
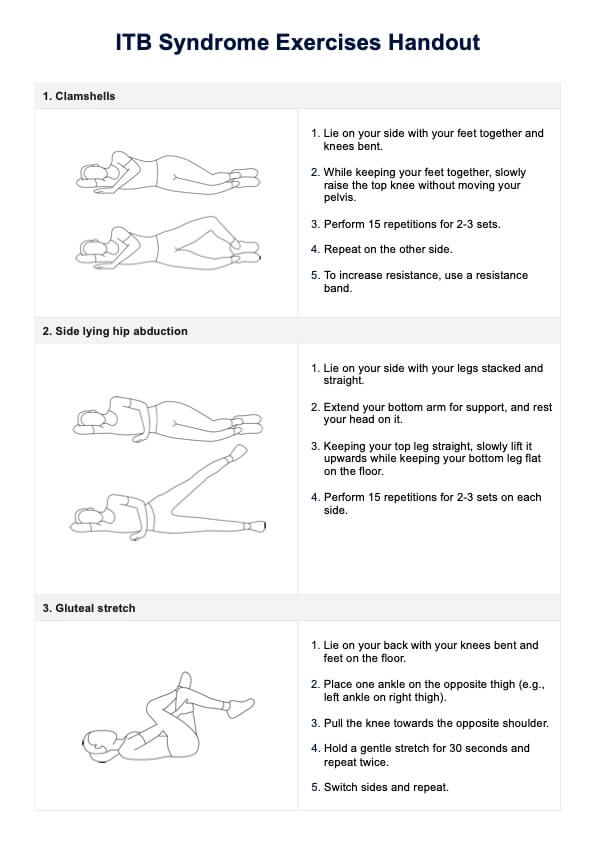
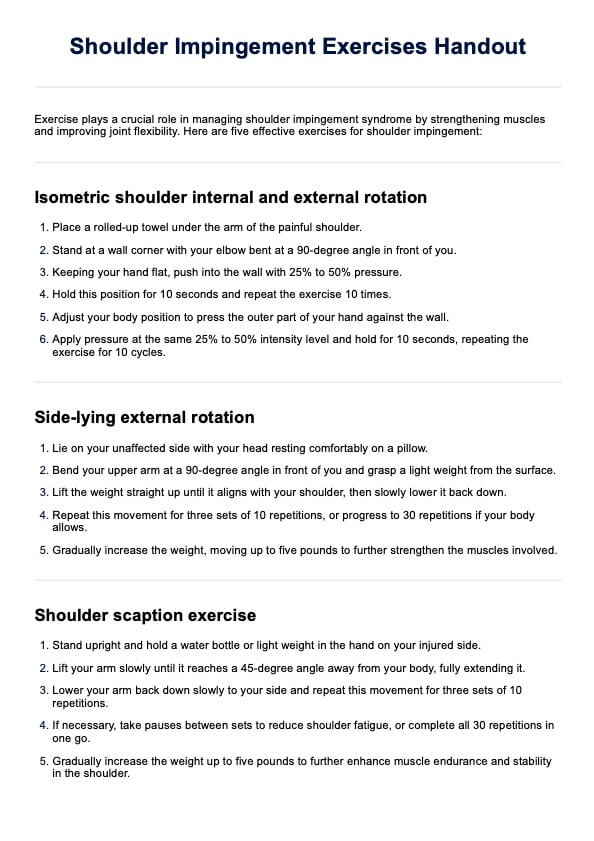
These targeted exercises aim to strengthen the hip muscles and improve mobility, particularly in cases of gluteus medius tendinopathy. Each exercise addresses a specific aspect of hip function to promote recovery and enhance stability. Here's how to teach your patients to do each exercise:
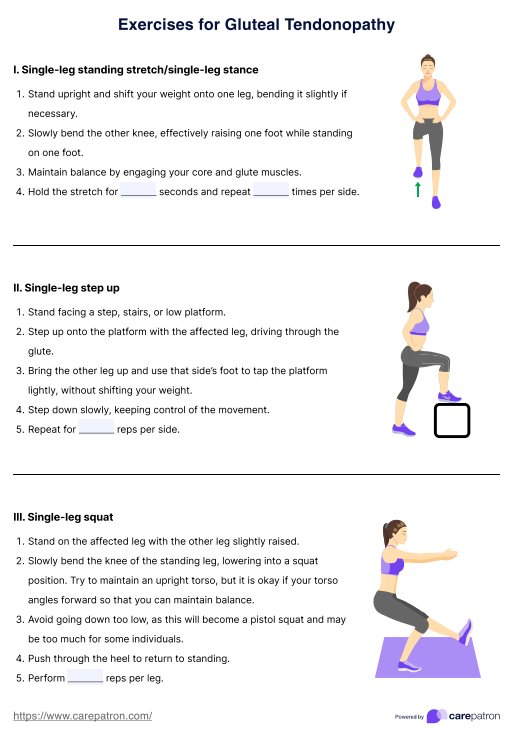
1. Single-leg standing stretch / single-leg stance
The single-leg standing stretch focuses on improving balance and engaging the hip muscles. To perform this exercise, stand upright and shift your weight onto one leg. You may find this easier with a slightly bent leg. Raise the opposite leg by bending the knee while activating your core and glute muscles to maintain stability. This exercise enhances coordination and balance by training the muscles needed to support single-leg activities.
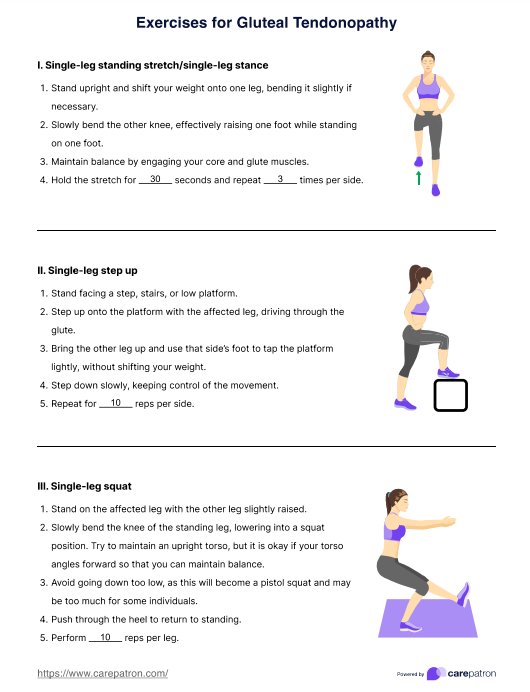
2. Single-leg step up
The single-leg step up strengthens the hip abductors and enhances stability. Begin by standing in front of an elevated surface, such as a step or platform. Step onto the platform with the affected leg, engaging the glute muscles to power the movement. Use the opposite foot to lightly tap the platform without shifting weight onto it, then step down slowly and with control. This exercise targets the muscles responsible for lateral stability and improves balance during movement.
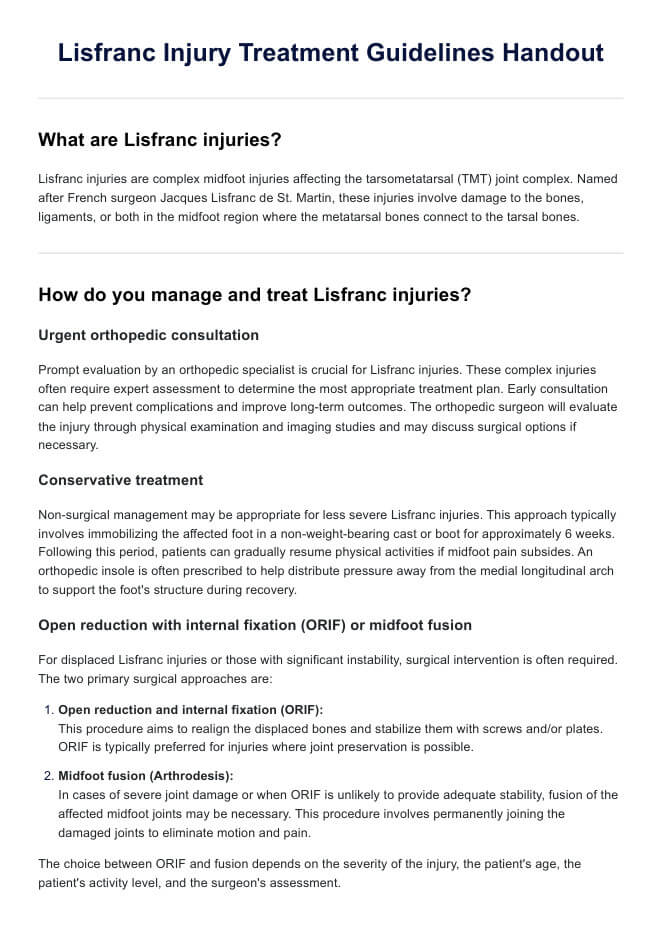
3. Single-leg squats
The single-leg squat is a functional exercise that strengthens the hip muscles while enhancing mobility. Stand on the affected leg and raise the opposite leg slightly off the ground. Lower yourself into a squat by bending the standing leg, and you might find it unavoidable that your torso angles forward for balance. Push through the heel of the standing leg to return to an upright position. This exercise mimics real-life movements and improves lower limb strength, essential for activities such as walking and climbing.
4. Leg lifts
Leg lifts target the gluteal muscles and improve hip extension strength. To perform this exercise, lie on your front with both legs extended. Lift one leg behind you, keeping it straight, and lower it in a controlled manner. This movement activates the hip extensors and contributes to better muscle endurance, helping relieve discomfort caused by gluteal tendinopathy.
5. Side leg lift exercise
The side leg lift exercise strengthens the gluteus medius, a critical muscle involved in stabilizing the pelvis. Start by lying on your side with your body aligned. Lift the upper leg without bending the knee, then lower it slowly. This exercise addresses weakness in the hip abductors and plays a key role in managing gluteus medius tendinopathy by enhancing hip stability during movement.
6. Standing leg raise
The standing leg raise is designed to enhance hip flexion strength while activating core stabilizers. Stand upright, using a stable surface for support if necessary. Slowly raise one leg in front of you while keeping that knee straight, then lower it back to the starting position with control. This exercise targets the muscles responsible for hip flexion, improving the ability to lift and control the leg during everyday activities.
Treatment options for gluteal tendinopathy
Gluteal tendinopathy can be managed through various commonly prescribed interventions aimed at reducing pain, restoring function, and preventing future injury. Below are standard treatment approaches:
- Manual therapy: Hands-on techniques, such as soft tissue and joint mobilization, to relieve tension and improve mobility.
- Biomechanical corrections: Addressing posture, gait abnormalities, and movement patterns to reduce tendon stress.
- Pain management: Includes non-steroidal anti-inflammatory drugs (NSAIDs) and ice or heat therapy for symptom relief.
- Corticosteroid injections: Temporary relief of inflammation and pain, especially in cases not responding to conservative care.
- Exercise therapy: Strengthening and flexibility exercises, targeting hip abductors, are integral to long-term management and recovery.
Commonly asked questions
Correct diagnosis of gluteal tendinopathy happens through a combination of clinical examination, patient history, and imaging studies. A healthcare professional will assess symptoms, such as lateral hip pain and weakness in the hip abductors and may use ultrasound or MRI to confirm the diagnosis and rule out other conditions.
Individuals with gluteal tendinopathy should avoid activities that place excessive strain on the hip abductors, such as running, prolonged standing, climbing stairs, or sitting with crossed legs. Avoiding repetitive movements or high-impact exercises can help prevent further irritation and promote healing.
The best sitting position involves sitting on a cushioned surface with both feet flat on the ground, ensuring that the hips and knees are aligned at a 90-degree angle. Avoid sitting with crossed legs or leaning to one side, as these positions can exacerbate symptoms by increasing stress on the affected tendons.