SOAP notes are invaluable in dentistry. They provide a structured format for documenting patient care. This system ensures that all relevant information—subjective complaints, objective findings, assessments, and treatment plans—is systematically recorded. This structured approach enhances the accuracy of patient records, aids in creating comprehensive treatment plans, and supports effective communication among dental professionals.
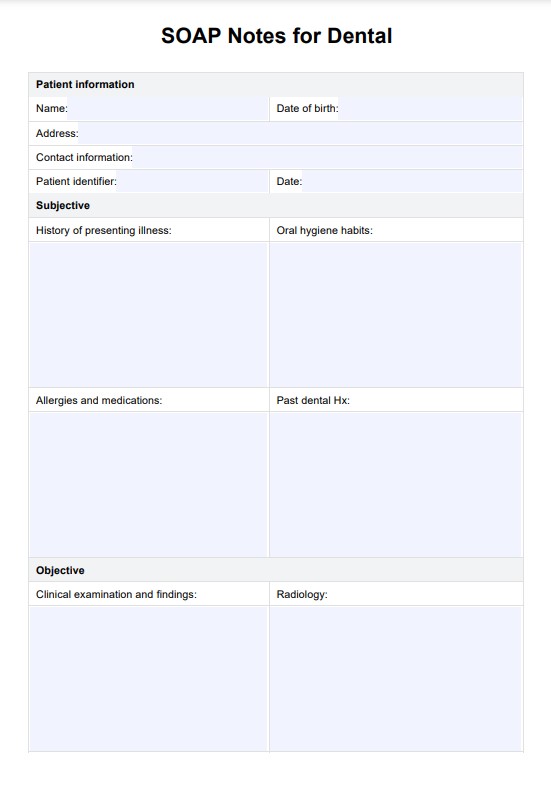
SOAP Notes for Dental Template
A simple PDF dental SOAP Notes template designed for use by dentists, orthodontists, or dental nurses.
SOAP Notes for Dental Template Template
Commonly asked questions
Using a template for dental notes standardizes documentation, enhancing patient record consistency and accuracy. A template ensures that all critical information, such as patient history, clinical findings, and treatment plans, is captured systematically. This reduces the risk of missing important details and improves notetaking efficiency.
Findings from a dental X-ray should be recorded in the "Objective" section of SOAP notes. This section includes all observable data from clinical examinations and diagnostic imaging. Detail the x-ray findings, such as any abnormalities, bone structures, or signs of decay, along with relevant measurements or comparisons.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











