Looking for a way to document your patient's progress in a structured and organized manner? Read our guide to learn about the SOAP method of writing and organizing notes. Then, download our SOAP Progress Notes template to use for documenting your patient/client sessions moving forward.
## **What are SOAP progress notes?**
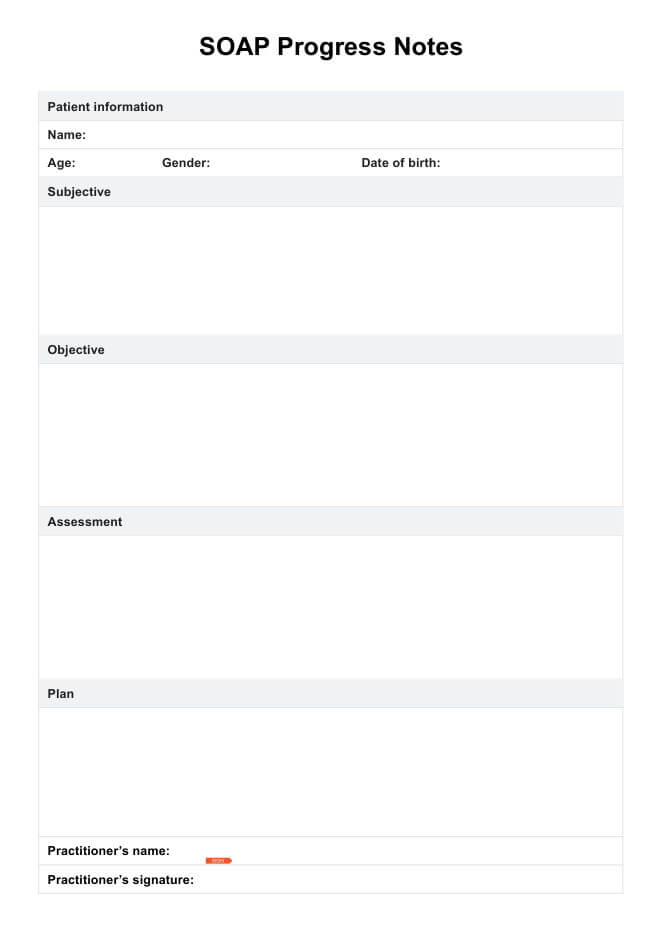
SOAP notes are a specific type of format structure for progress notes. This form of clinical documentation aims to track patient improvement, facilitate better communication among care team members, and provide evidence for insurance providers. A comprehensive SOAP note categorizes information into four relevant sections:
### **Subjective**
This section details the patient's reporting of their chief complaint. Direct quotes from the patient are often included, as well as their symptoms and how the problem impacts their day-to-day life.
### **Objective**
The objective section includes the practitioner's observation of the patient's behavior and affect. It should also include details regarding any tests, examinations, scans, or laboratory screenings completed during the session.
### **Assessment**
The assessment is essentially a synthesis of the subjective and objective sections, where the practitioner evaluates the patient's condition. It is where the practitioner analyzes or interprets the patient's complaint, how they responded to treatment, and whether they are progressing toward their goals. Learn more about how to conduct the assessment part of a SOAP note.
### **Plan**
Finally, the practitioner writes the patient's future treatment details in the plan section. These could include upcoming sessions, referrals, changes to the treatment plan, and any short—or long-term goals.
Writing SOAP notes and using a template offers several benefits for mental health professionals. Among them are:
- Providing a consistent structure, [cognitive framework](https://www.ncbi.nlm.nih.gov/books/NBK482263/), and documentation method ensures all essential information is organized and captured logically, helping with clinical reasoning.
- Pre-formatted templates eliminate the need to create documentation from scratch, saving valuable time for healthcare practitioners.
- SOAP note templates aid with clear and detailed documentation. It prompts practitioners to record both subjective and objective data, including past medical history, assessments, and treatment plans. This reduces the risk of overlooking crucial details and [enhances the effectiveness of communication](https://pmc.ncbi.nlm.nih.gov/articles/PMC12431931/) between healthcare professionals.
- Many SOAP note templates are available in editable SOAP note formats, allowing healthcare practices or individual practitioners to customize the templates to suit their specific needs or specialties. Examples of more personalized SOAP notes include [SOAP Notes for Therapy](https://www.carepatron.com/templates/soap-notes-for-therapy-template/) and [SOAP Notes for Physical Therapy. ](https://www.carepatron.com/templates/soap-notes-for-physical-therapy-template/)
## **How to use our SOAP Progress Notes Template PDF**
Healthcare professionals can follow these steps to use our free SOAP note template for effective medical documentation:
### **Step 1: Access and download the template**
You can access a blank SOAP note template by clicking on the links within this page or by exploring Carepatron's template gallery. You can also check the SOAP note example within this guide as a reference point to make the most out of this resource.
### **Step 2: Fill out details**
The next step is to document patient information, which involves assessing the patient's health status, present illness, medical history, and physical examination findings. You must fill out the SOAP note with the date of your session with the client, their name, and ID (if applicable).
### **Step 3: Write the SOAP sections**
At the heart of SOAP note writing lie its four components: the subjective, objective, assessment, and plan sections. To complete the SOAP note, enter information in each part, listing only critical details concisely. It's okay if some sections are longer than others.
Here's an example to better understand how to write a SOAP note:
- **S (Subjective**): The client reports feeling tired, struggling to go to work, and getting out of bed in the morning. They also often have negative thoughts and experience restless sleep.
- **O (Objective)**: The client was only able to have an online therapy session. Their personal hygiene wasn't intact, which is not typical. However, after taking his new medication, he appears more energized due to his increased appetite.
- **A (Assessment**): The client's behavior and symptoms reflect major depressive disorder. Further tests and observation are needed to determine the severity and duration of symptoms as well as identify any contributing factors.
- **P (Plan)**: Diagnosis is major depressive disorder that's recurrent and severe, as seen by their ongoing symptoms, which impact their daily life. Interventions such as therapy sessions and medication are required and will be taken. In addition, the patient will be asked to do daily physical activity and prepare a safety plan.
### **Step 4: Sign the note**
Include your name and signature for authorization at the bottom of the SOAP note.
### **Step 5: Securely store your SOAP notes**
Once you've completed the entire SOAP note, make sure that you securely store it, ideally within a [practice management software](https://carepatron.com/feature/practice-management-system). Ideally, this software can also have a built-in SOAP notes feature to help you stay compliant and provide a greater protection barrier against data breaches.
## **Best practices in using the SOAP format**
When it comes to effectively using the SOAP format for documenting patient encounters, following best practices can ensure comprehensive, accurate, and efficient documentation. Here are some essential best practices to keep in mind:
- **Be specific and concise**: In each section of the SOAP note, aim to provide relevant and precise details while avoiding ambiguous or subjective statements. Use clear and concise language to communicate the necessary information effectively.
- **Utilize appropriate terminology**: Incorporate standard medical terminology and abbreviations to ensure consistency and clarity within the healthcare team. This practice prevents misunderstandings and facilitates effective professional communication.
- **Document objective data**: In the Objective section, prioritize recording measurable and observable data obtained through physical examinations, vital signs, lab results, and other diagnostic findings. This objective information forms the foundation for accurate assessments and treatment plans.
- **Link assessments to findings**: Ensure that the Assessment section directly correlates with the Subjective and Objective information gathered. Clearly outline the rationale behind the diagnosis or identified condition based on the documented findings and measurable data.
- **Outline a comprehensive plan**: In the Plan section, provide a detailed outline of the proposed treatment plan, including medications, therapies, follow-up appointments, patient education, and any other recommendations based on the assessment. A well-documented plan can improve patient adherence, facilitate continuity of care, and improve coordination with other healthcare providers.
Read our blog article about [how to write SOAP notes](https://carepatron.com/blog/what-is-a-soap-note-how-to-write-them-examples) to learn more.
Following the SOAP structure and best practices helps healthcare providers create efficient and accurate medical records that ultimately improve patient outcomes and quality of care.
## **References**
Hidalgo Tapia, E. C., León Yosa, J., Olalla García, M. H., Clavijo Morocho, N. J., & Sanmartín Calle, Y. A. (2025). Effectiveness of Nursing Documentation Frameworks (SBAR, SOAP, and PIE) in Enhancing Clinical Handoffs and Patient Safety. Cureus. https://doi.org/10.7759/cureus.89957
Vivek Podder, Lew, V., & Sassan Ghassemzadeh. (2023, August 28). SOAP Notes. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482263/