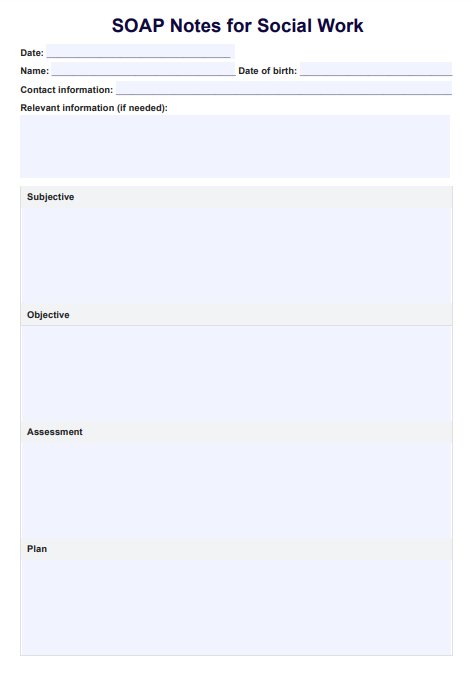
SOAP Notes For Social Work Template
Our SOAP Notes for Social Work Template enhances the quality of your note-taking while streamlining your work.


What is a social work SOAP notes template?
SOAP notes for social work are a highly efficient way to structure and organize notes when assessing clients and their situations. They elevate the quality and standard of care within your workplace and simplify your workflow without compromise. They're also widely used across social work environments and contexts and allow you to keep accurate records of the client's progress and client interactions.
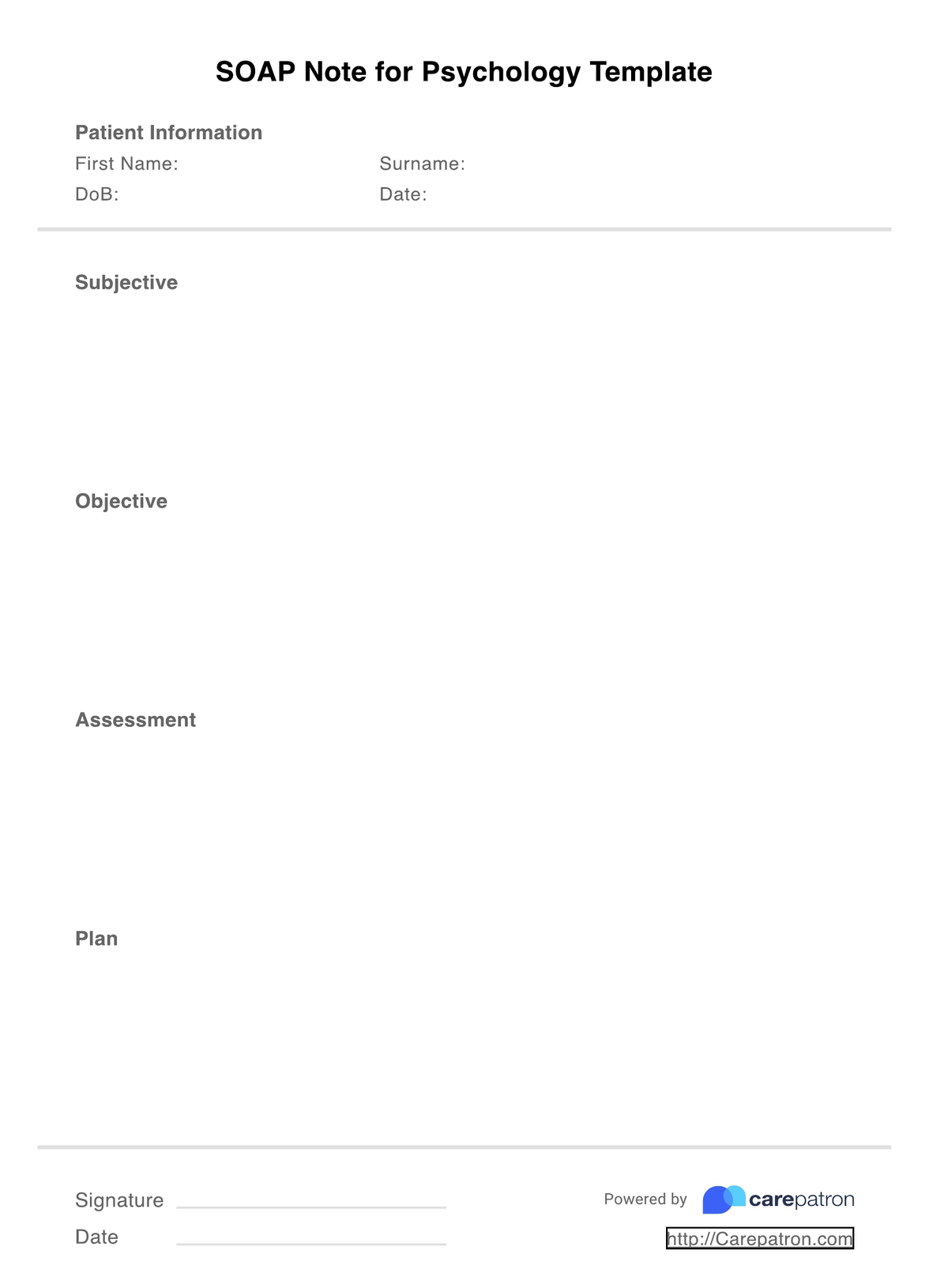
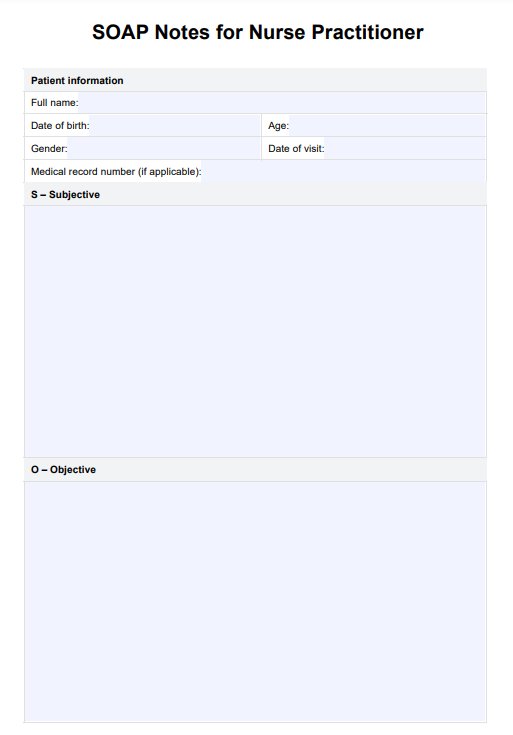
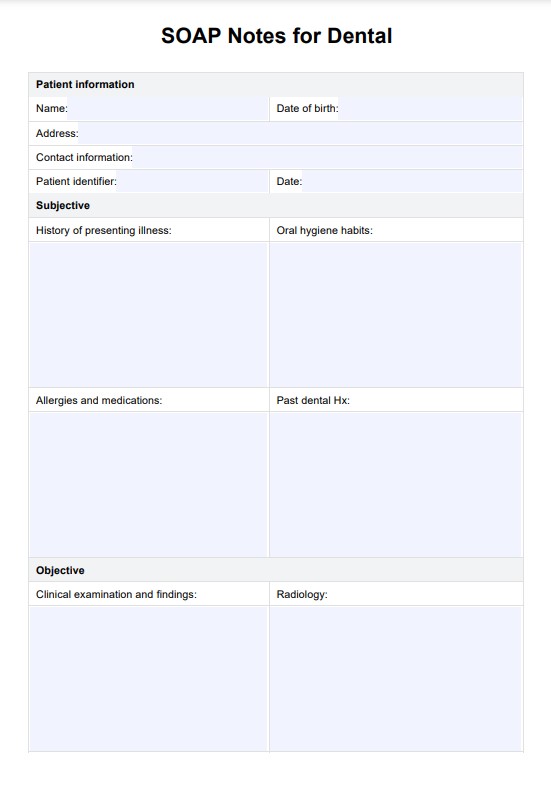
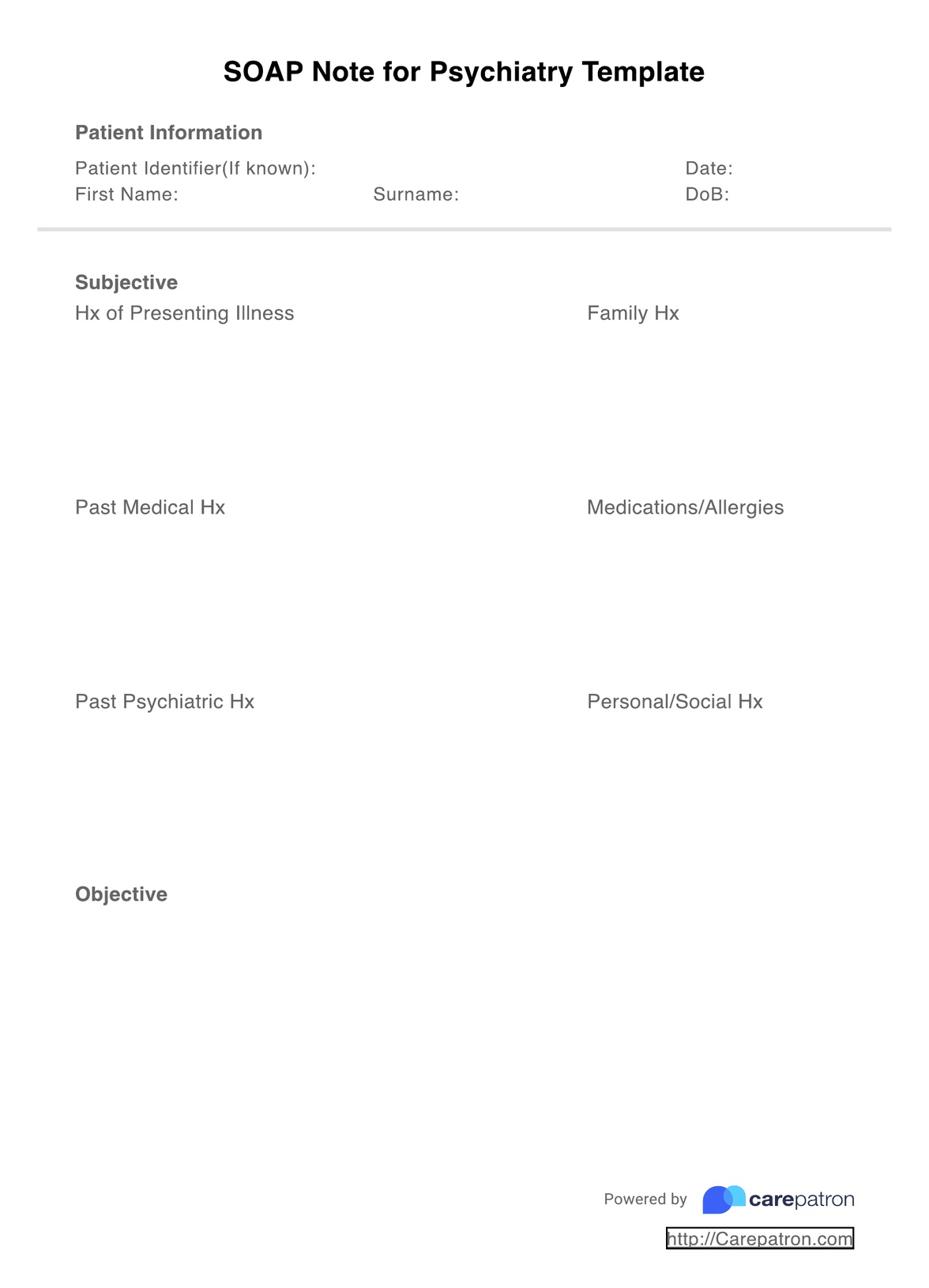
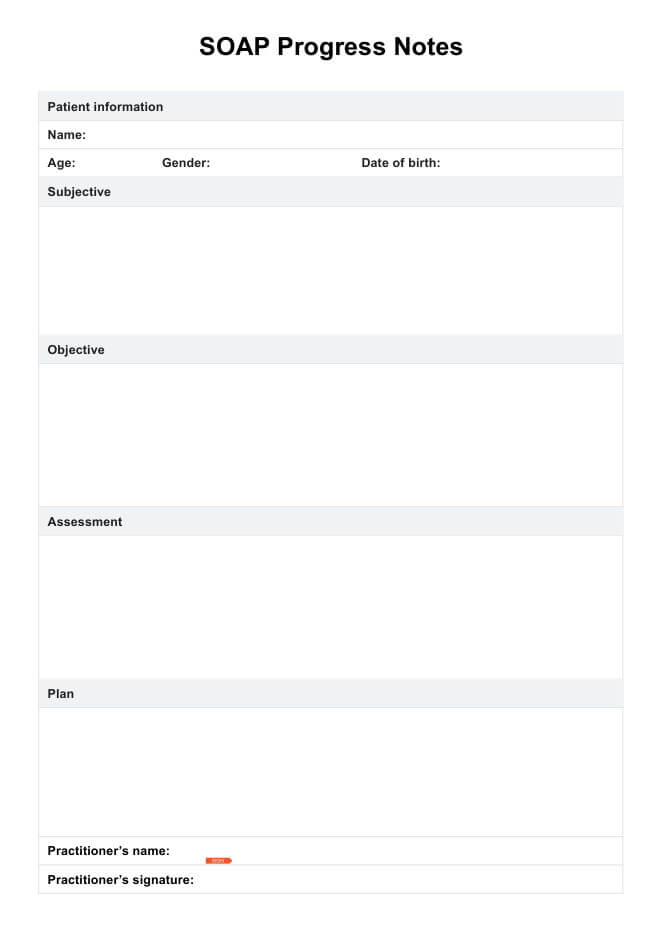
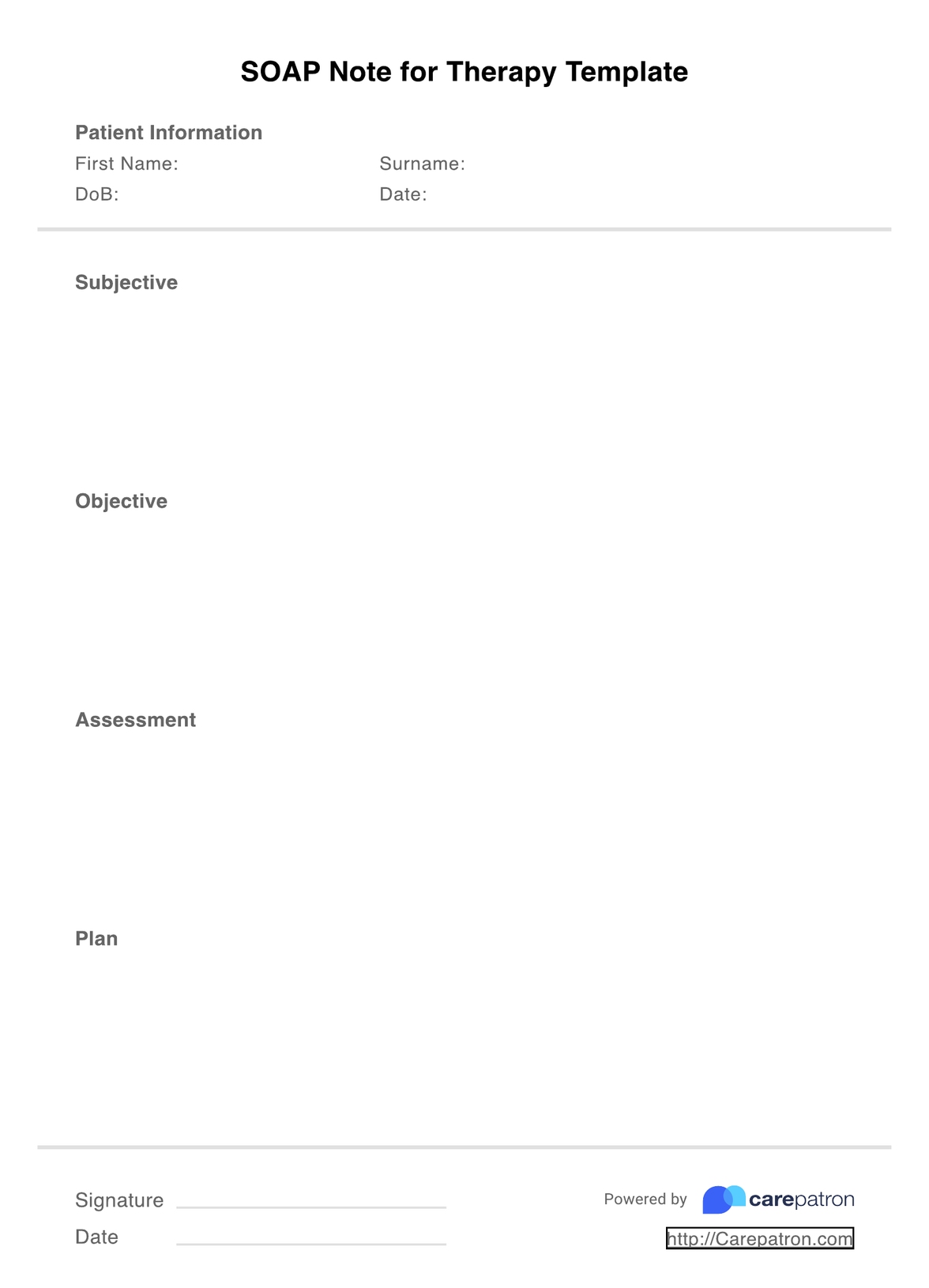
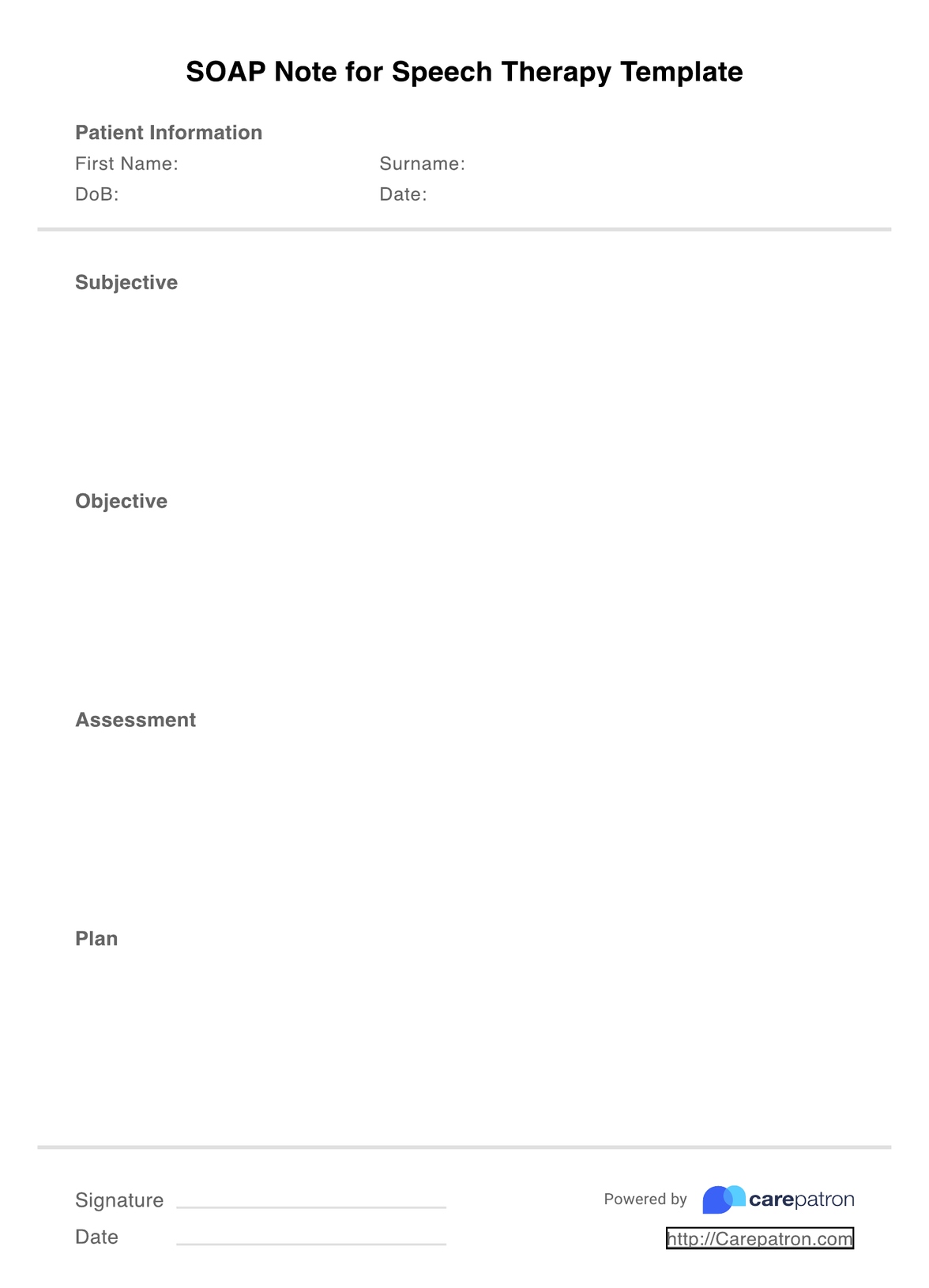
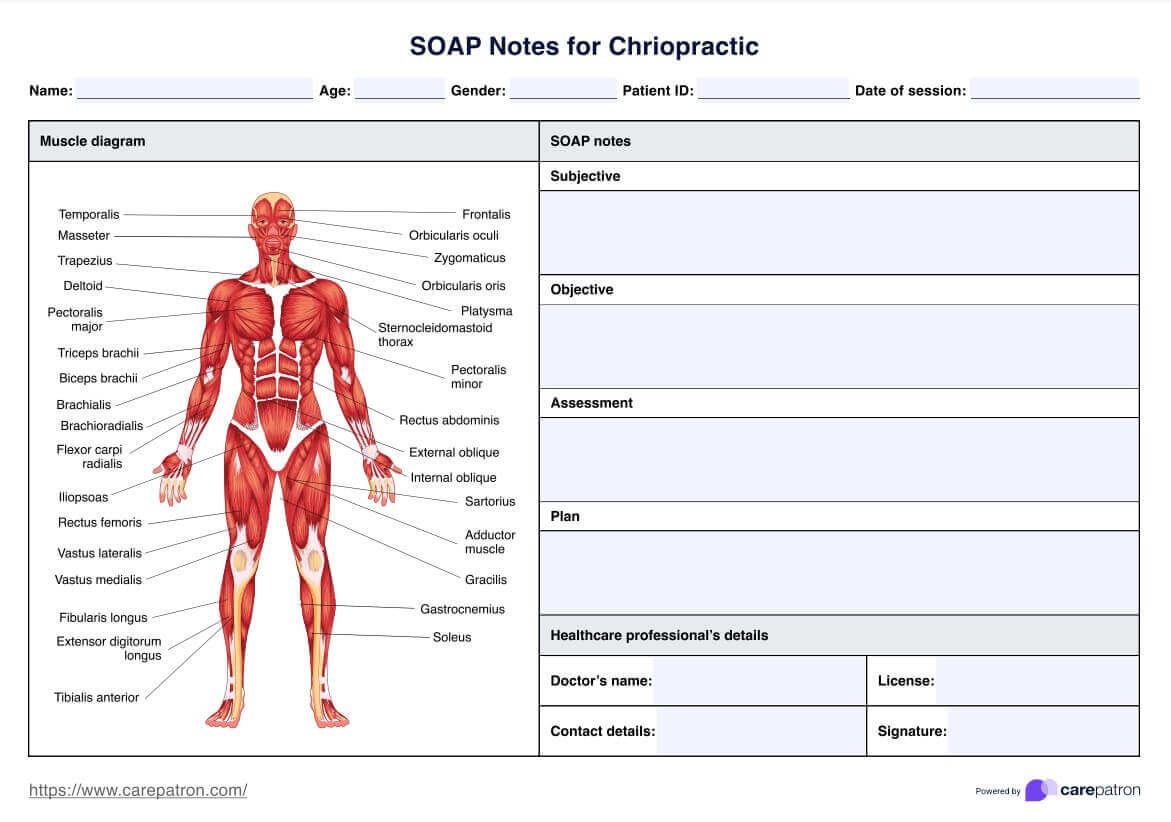
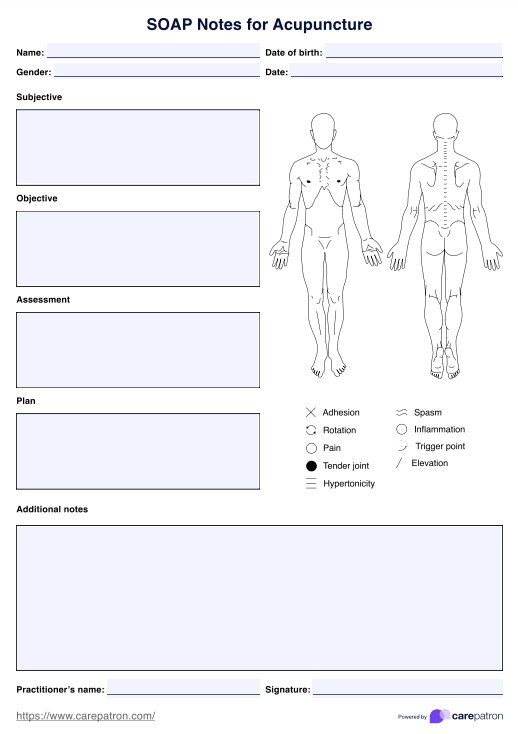
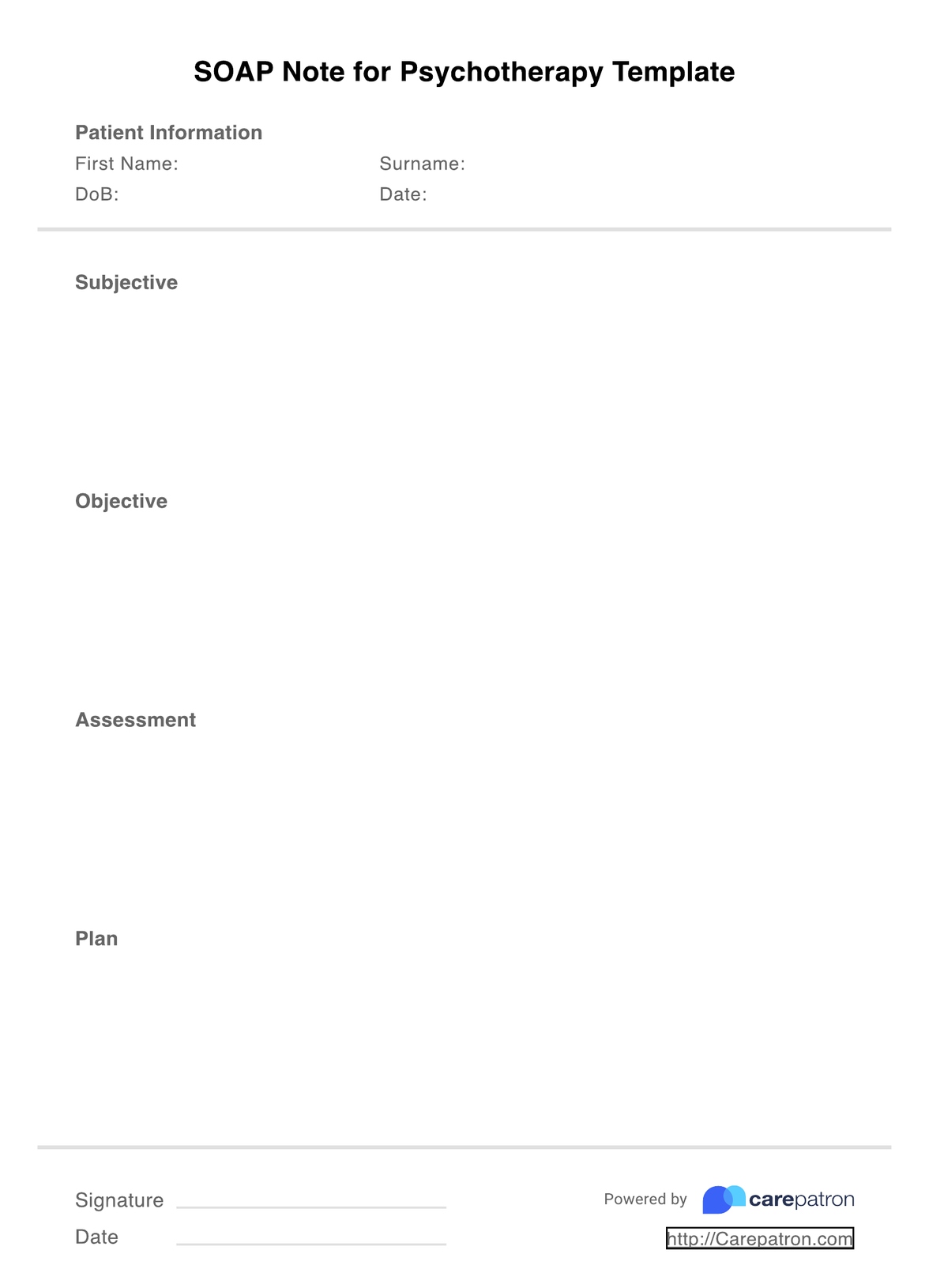
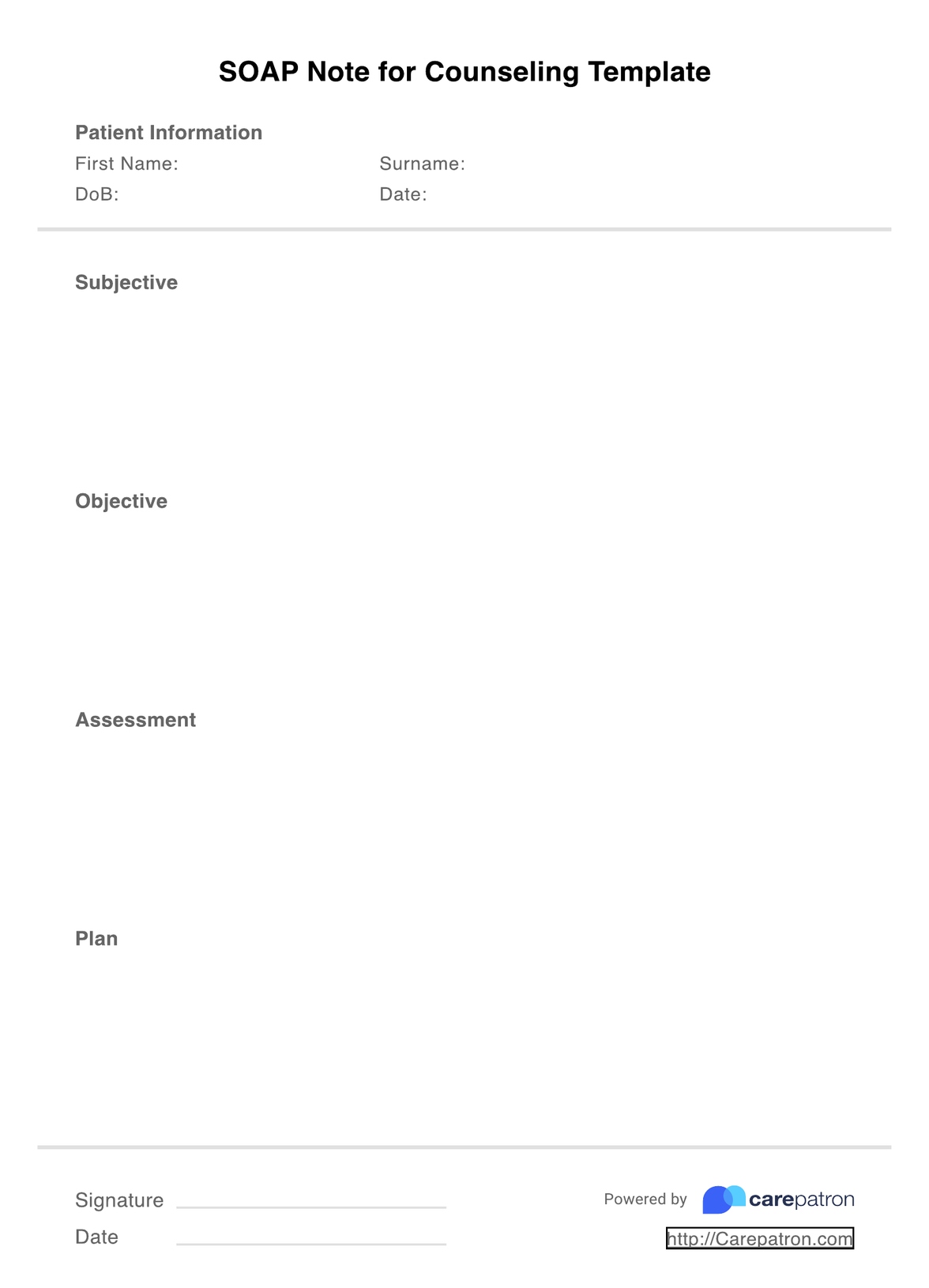
SOAP notes for social workers incorporate a universally accepted form, meaning that they are widely accessible by various healthcare professionals from all social, community, and health backgrounds, like child social workers, criminal social workers, and international social workers. These notes typically cover the four following major areas, namely:
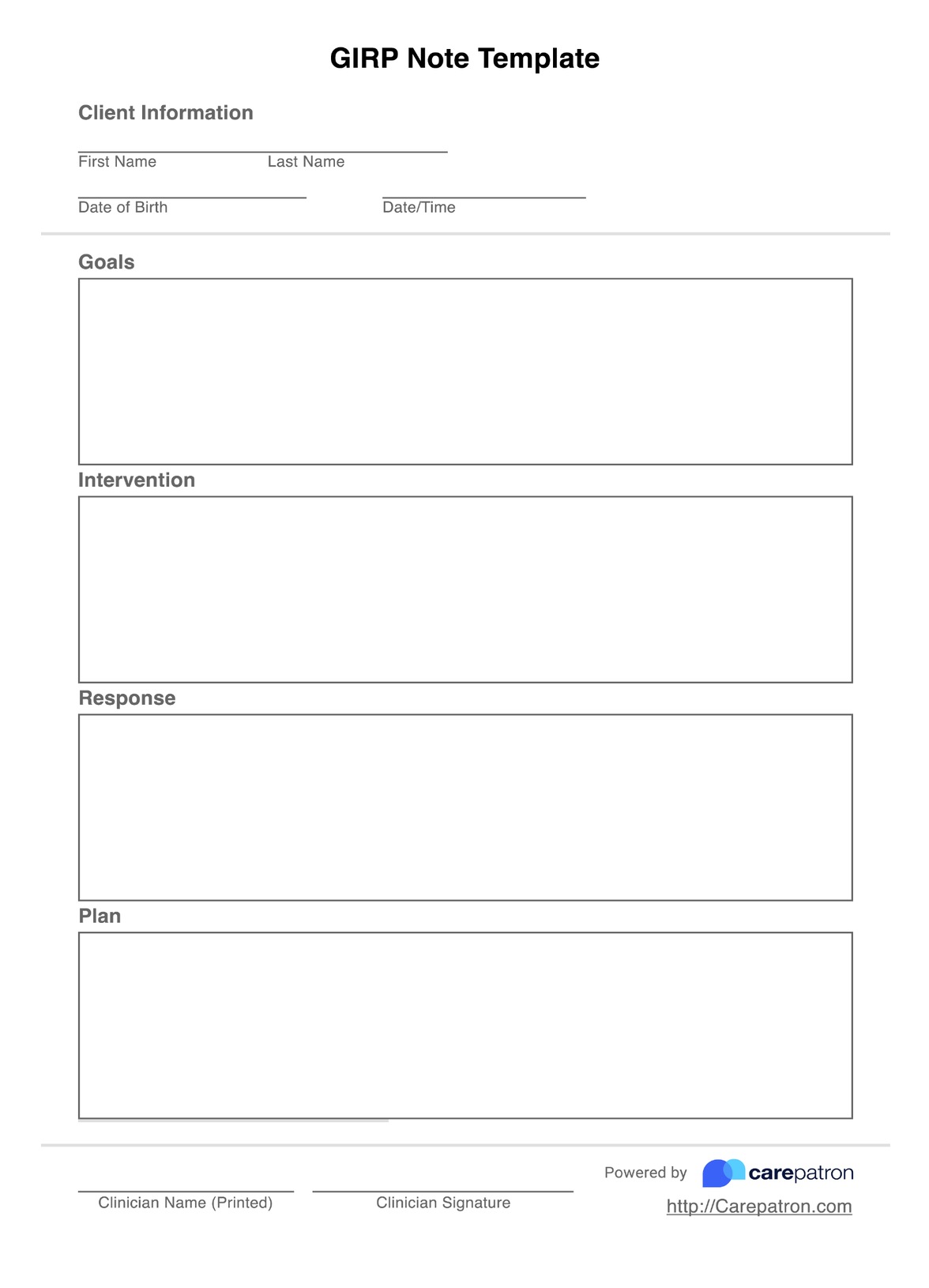
- Subjective: This includes subjective information concerning the client's feelings, thoughts, and any relevant client behavior. This will typically include what the client reports feeling, verbatim, as well as quotes from close relations if needed. The information gathered will help you better understand the client's perspective.
- Objective: The objective section pertains to factual or measurable data that can be quantifiably measured. Although social work doesn't always involve this kind of information, it is useful to include it as supporting evidence if relevant. This may entail vital signs, medical history, records, and other quantifiable data.
- Assessment: Assessment refers to any diagnosis, comments, or evaluations about the client's current state, as well as any current information on the client's treatment or progress plans.
- Plan: The final section explores the client's future course of action and progress goals. This may mean amending the current plan or creating a new one and indicating the time and date of any upcoming sessions.
SOAP Notes For Social Work Template
SOAP Notes For Social Work Template Example
How to use this SOAP Notes for Social Work Template
You may wonder, how exactly do you use SOAP (social work) notes? Although it may differ from social worker to social worker depending on your own unique needs and approach to work, the content essentially remains the same. To effectively incorporate SOAP notes into your social work practice, consider the following steps:
Step 1: Download the template
First, you need to download the PDF SOAP Note Template from the link above to use it. This should automatically open within your PDF software and be ready to edit. If you need a guide, you can also access our free social work SOAP Note example in the guide.
Step 2: Complete your credentials
It is very important that before you note client evaluations, you fill in the time and date of your sessions, as well as the client's name and basic information. This supports insurance and billing processes that may follow.
Step 3: Fill in the four SOAP sections
Once you've completed your credentials, record the subjective and objective information, assessment details, and plans in the corresponding sections of the SOAP note in as much concise and relevant detail as possible.
Step 4: Sign the document
It is strongly recommended that you sign the document to boost HIPAA compliance and credibility. Be sure to consult with your state legislation, as some states enforce this step!
Step 5: Securely store your SOAP notes
After you have finished your SOAP note and are happy with its accuracy, you must store it in a secure space. Ideally, this is a practice management software that incorporates encryption and other security protocols and safeguards to guarantee the highest level of protection.
Benefits of using SOAP notes for social workers
Using social work SOAP note templates also brings about greater benefits to you and your practice and ensures that you are strengthening the quality of your work. These benefits include:
Standardized notes
With SOAP note formatting, you can increase consistency across all clinical documents by using a standardized format. Treat all your clients with the same high-level care, and know your notes hit the nail on the head every time.
Easy organization
Because SOAP notes cover all the essential sections that you need in note-taking processes, you don't need to put any extra effort or thought into what goes into your document. You can organize notes efficiently, with all details structured logically.
Track progress
Naturally, SOAP notes are a great addition to social work as you can closely monitor client progress notes across time. This makes for more dedicated and accurate treatment plans, which is always a win.
Meaningful connections
One of the most important aspects of social work is connecting with clients and helping them accomplish healthy life goals. Communication is key, and with SOAP notes, you can better understand clients and make more meaningful connections. You can observe their perspective from multiple angles and make sound, evidence-based, and grounded professional judgments.
Save time
With SOAP notes, you can reduce the time spent writing documentation, which is extremely valuable. Any extra downtime to add value elsewhere is always welcome, especially with the hectic schedules that often accompany this kind of work. Time is valuable, and you can improve on this with SOAP notes.
Fulfill legal obligations
SOAP notes are excellent safeguards for cases of legal action. Social workers may likely find themselves in legal cases, and SOAP notes are a great way of providing evidence for your client, boosting your credibility. Demonstrate your expertise and create SOAP notes on par with legal standards.
Insurance
Medical billing and coding processes often use SOAP notes to improve accuracy within insurance claims. With SOAP notes, you can oversee all the medication, instruments, evaluations, and assessments that require reimbursement. This means you're far less likely to forget the small stuff, and you can increase revenue and disposable costs within your work.
Easy workflow
Use SOAP notes to optimize your workflow. You can produce high-quality clinical documents with significantly less effort, leaving time to attend to other important social work obligations.
Commonly asked questions
This is a great question and also an important one. It's important not to waffle in your SOAP notes, so ideally, they should be 1-2 pages long, with 3 pages and beyond becoming excessive.
Working within the social work industry may involve working with more than one type of person in a session. However, having one SOAP note for multiple people is not recommended, as this can be a conflict of interest and can result in complications if the individual desires one-on-one treatment later. To keep things simple, stick to one person per SOAP note.
Yes, they absolutely can. It is recommended that they use electronics to reduce time, but this is not a must. If you prefer handwritten documents that are more efficient for you, feel free to do so.

















-template.jpg)