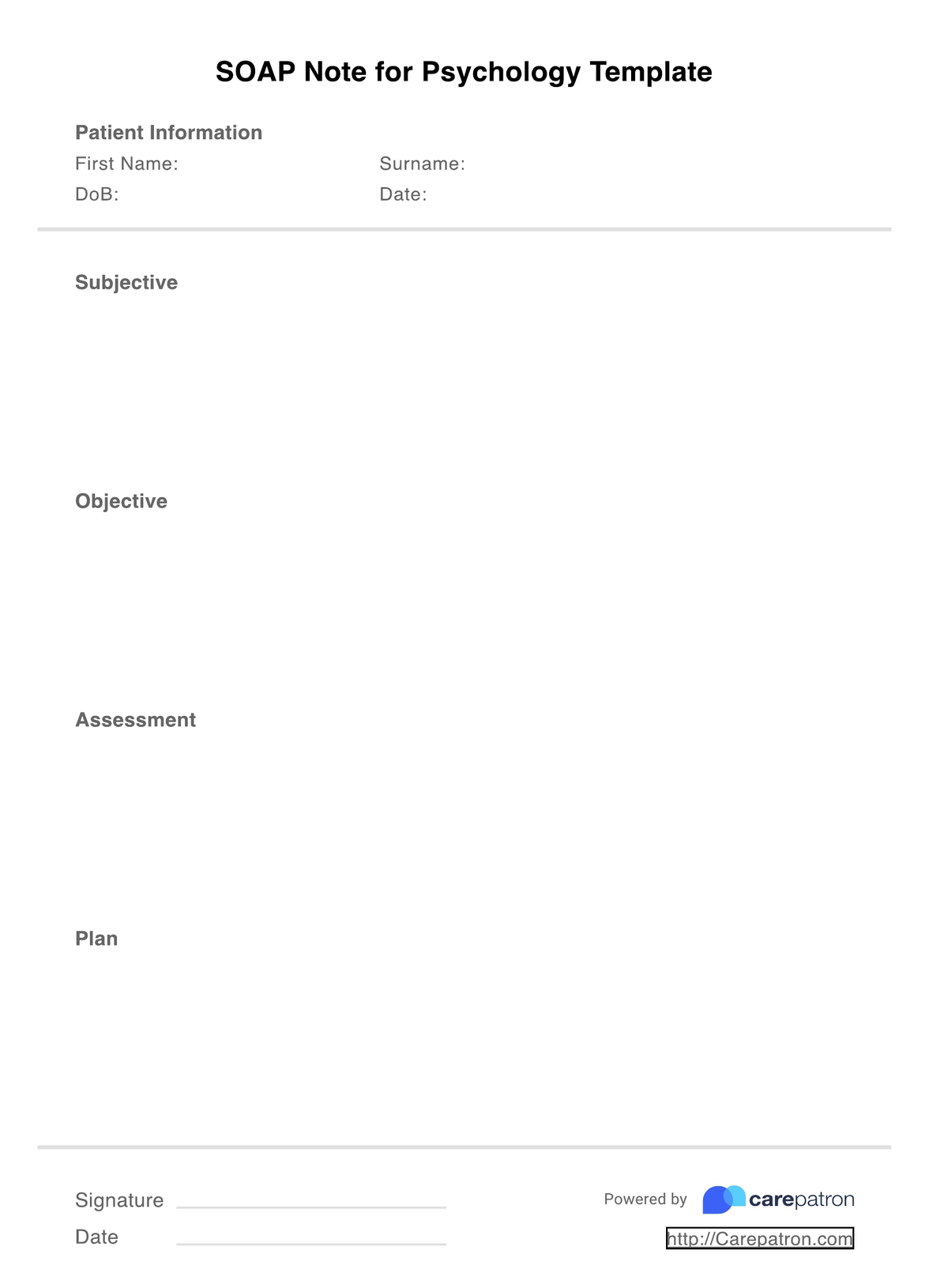
What is a Psychology SOAP Notes Template?
A SOAP note is a specific type of formatting structure that helps psychologists organize their progress notes. Following each session with a client, psychologists are required to write progress notes that detail relevant information regarding that session. SOAP notes separate this information into four sections:
Subjective: The subjective section includes the patient’s description of their concern. This section often includes direct quotes from the patient and information regarding symptoms and how the concern is impacting their everyday life.
Objective: The objective section refers to your clinical observations about the patient’s behavior, response to intervention, and any tests or examinations that were completed.
Assessment: A synthesis of the previous two sections, the assessment is your professional interpretation of the session. This includes any improvements or declines in health you have observed, how the treatment plan is progressing, and whether the patient has achieved their goals.
Plan: In the final section of the SOAP note, the plan outlines the details of upcoming sessions, any changes to the treatment plan, and goals that the patient has.
Using a SOAP note format as a psychologist will help you keep your documentation clear, concise, and organized. As the most popular format for progress notes, the SOAP structure is also very useful for communicating between different members of a patient’s care team.