Patellar Instability Treatment Guidelines
Get our free Patellar Instability Treatment Guidelines to have on hand guidelines for evaluating and managing patellar instability. Download today!


What is patellar instability?
Patellar instability is a condition where the patella dislocates from the trochlear groove, often due to injury to the medial patellofemoral ligament (MPFL). Chronic patellar instability may result from anatomic factors like patella alta, abnormal tibial tubercle position, or trochlear dysplasia.
Patellar instability is diagnosed based on history, exam findings like patellar apprehension with knee flexion, and imaging. Treatment options include bracing, physical therapy to strengthen the medial quadriceps tendon, and surgical procedures like MPFL reconstruction or tibial tubercle osteotomy for recurrent instability.
Symptoms of patellar instability
Common symptoms of patellar instability include:
- Knee pain, especially in the front of the knee
- Feeling of the knee "giving way" or buckling
- Visible deformity or misalignment of the patella
- Swelling and stiffness in the knee
- Apprehension or pain when extending the knee
Causes of this instability
Several factors can contribute to patellar instability:
- Trauma or direct blow to the knee causing dislocation
- Anatomic factors like patella alta, trochlear dysplasia, increased Q-angle
- Generalized ligamentous laxity
- Muscle imbalances or weakness, especially in the quadriceps
- Recurrent patellar dislocations cause injury to stabilizing structures like the medial patellofemoral ligament (MPFL)
How is this instability assessed?
A comprehensive evaluation is crucial for accurate diagnosis and appropriate management. This involves a detailed patient history to identify the mechanism of injury, prior dislocations, and risk factors such as family history, hyperlaxity, or anatomical abnormalities.
A thorough physical examination assesses patellar mobility, alignment, apprehension, and associated injuries. Key exam findings include tenderness over the medial patellofemoral ligament (MPFL), increased passive patellar translation, and a positive patellar apprehension test.
Imaging studies such as X-rays, CT scans, or MRI evaluate bony anatomy, alignment, and soft tissue injuries like MPFL tears. Specific measurements, including patellar height (Insall-Salvati ratio, Caton-Deschamps index), trochlear depth, and tibial tubercle-trochlear groove (TT-TG) distance, help identify anatomical risk factors for instability.
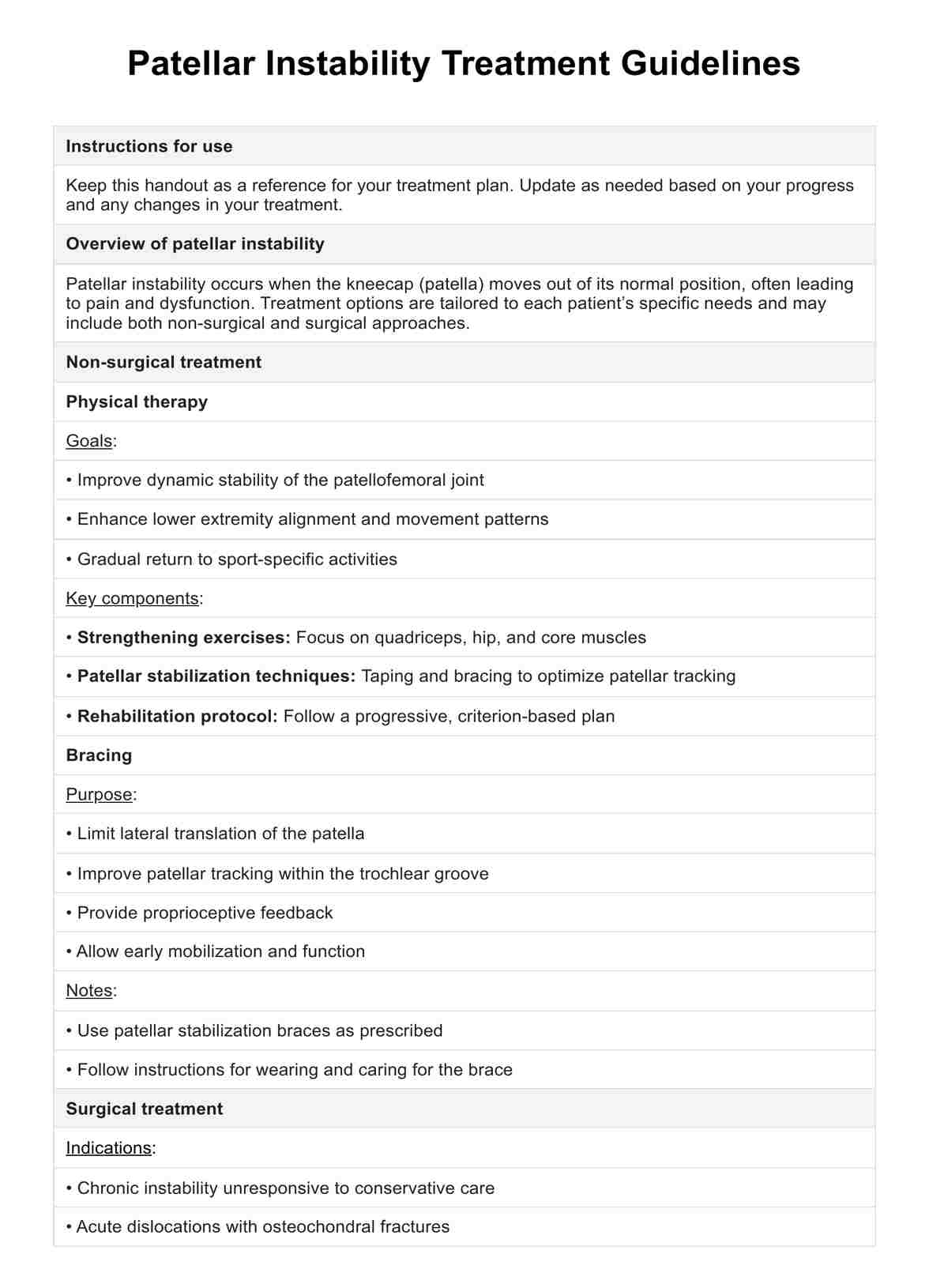
Patellar Instability Treatment Guidelines Template
Patellar Instability Treatment Guidelines Example
How is patellar instability treated?
Patellar instability is treated on 4 main approaches:
Conservative treatment
The initial management of acute first-time patellar dislocations is usually conservative. This typically involves a brief period of immobilization in extension to provide comfort and allow early healing. Early range of motion and strengthening exercises are then initiated to prevent stiffness and muscle atrophy.
Surgery
Surgery is considered for chronic patellar instability unresponsive to conservative care or acute dislocations with osteochondral fractures. Common options include MPFL repair or reconstruction, tibial tubercle osteotomy, trochleoplasty, lateral retinacular release or lengthening, and repair of chondral or osteochondral injuries. The specific procedures are chosen based on a comprehensive evaluation of the individual's anatomical risk factors and pathology.
Physical therapy
Physical therapy is vital for both conservative and post-operative management of patellar instability. It focuses on strengthening the quadriceps, hips, and core to improve patellofemoral joint stability. It uses taping and bracing for optimal patellar tracking, enhances lower extremity alignment and movement, and gradually returns to sport-specific activities. A progressive, criterion-based rehabilitation protocol guides the patient’s return to full function.
Bracing
Patellar stabilization braces are used in conservative management to limit lateral patellar translation, improve tracking, provide proprioceptive feedback, and allow early mobilization. While they can enhance alignment and reduce pain, their long-term efficacy is uncertain.
Benefits of using this treatment guidelines template
Here are some of the many benefits of having a on hand:
- Structured treatment approach: By following a systematic approach, healthcare providers can ensure that all aspects of the patient's condition are addressed, from initial assessment to follow-up care.
- Personalized patient care: The template ensures that each treatment plan is customized to the individual patient's condition and needs, leading to more effective and targeted care.
- Enhanced communication Clear documentation and detailed guidelines improve communication between the patient, healthcare providers, and support staff, ensuring everyone is on the same page regarding the treatment plan.
- Consistency in care: Using a standardized template promotes consistency in treatment practices, which can lead to better patient outcomes and streamline the healthcare process.
- Comprehensive evaluation: The template encourages thorough evaluation and documentation of the patient’s condition, which aids in selecting the most appropriate and effective treatment options.
Commonly asked questions
Treatment depends on whether the instability is acute or chronic, the severity, and individual risk factors. Most first-time dislocations are treated conservatively with immobilization, PT, and bracing. Surgery is considered for recurrent instability or acute injuries with osteochondral fractures.
Surgical stabilization procedures like MPFL reconstruction and tibial tubercle osteotomy have good success rates in reducing recurrent instability.
Recovery time varies but most patients return to normal activities in 2-3 months after a first-time patellar dislocation treated conservatively. Return to sports may take 3-4 months. Recovery after surgical stabilization is longer, typically 6-12 months.
Patellar instability or medial patellar instability is diagnosed through a combination of patient history, physical examination, and imaging studies. Clinicians will assess symptoms such as pain, swelling, and episodes of the knee giving way. During the physical exam, special tests may be conducted to evaluate the stability of the patella.