Yes, it is a legal requirement that all patients can access their SOAP notes. For this reason, you must remain professional and objective in your documentation. Do not include any observation that isn't supported by evidence, and omit judgemental language, abbreviations, and jargon that aren't easily understood.
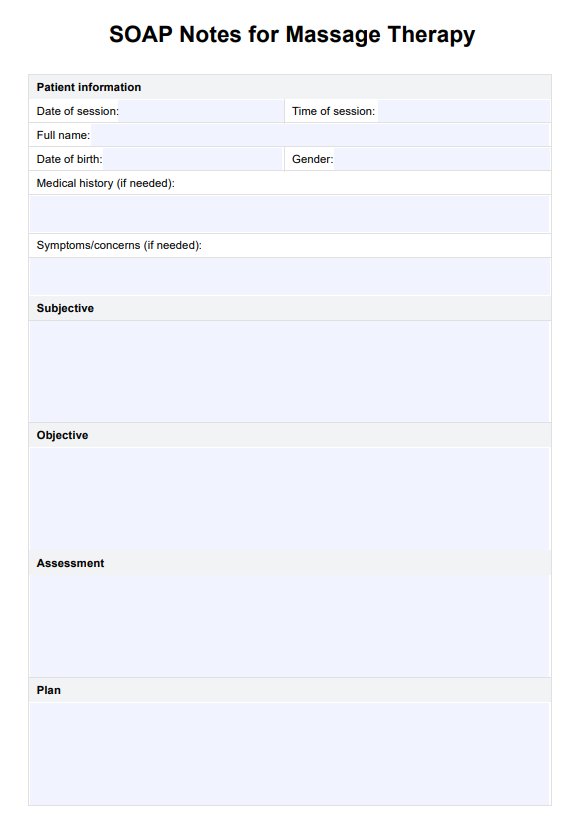
SOAP Notes for Massage Therapy Template
Streamline your clinical documentation and your accuracy and effectiveness in your massage therapy practice with our SOAP Notes for Massage Therapy Template.
SOAP Notes for Massage Therapy Template Template
Commonly asked questions
Yes, HIPAA regulations apply to SOAP notes. You must legally write progress notes and store them safely and securely. Because SOAP notes contain confidential data, you must have electronic and physical safeguards to protect your patients.
If you make a mistake on your SOAP note, draw a single line through the error, and then write the date and your initials. This ensures that the process of making the error and why it was changed remains clear to any third parties that may view the document.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











