What is a massage therapy SOAP notes template?
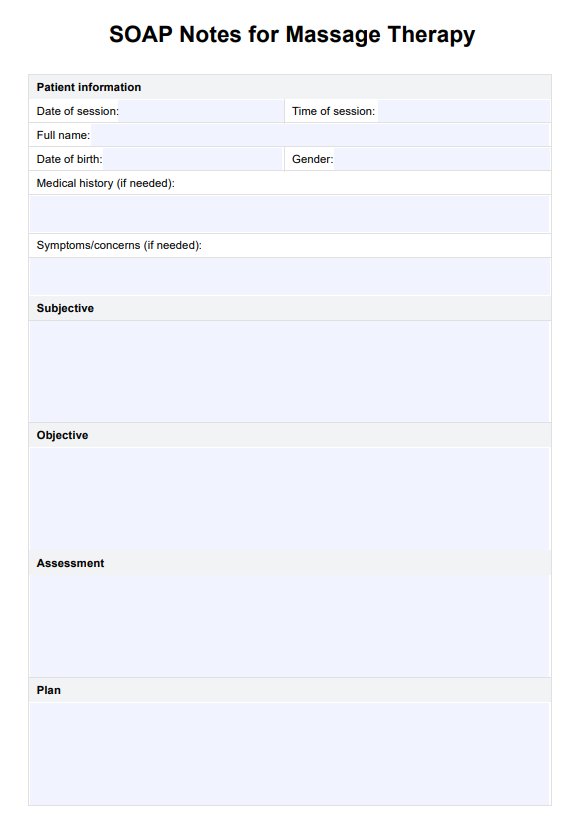
Writing progress notes is an essential component of working as a massage therapist. Progress notes are a type of clinical documentation that helps massage therapists keep track of the client's progress by documenting massage therapy sessions and detailing the important aspects of each session. One of the best ways to organize and streamline this note-taking progress is by using the Massage SOAP notes format. The SOAP note format separates relevant information into four different sections:
Subjective: The first section includes the patient’s subjective statements regarding their chief complaint. In this section, it can be a good idea to include direct quotes from the patient regarding their complaint, symptoms, and how their day-to-day life is being impacted.
Objective: In this section, you should include any observations you make about the patient’s behavior and affect. This information needs to be observable and measurable and should include any tests or examinations you conduct.
Assessment: The assessment is essentially a synthesis of the first two sections. You want to include your interpretation or analysis of the subjective and objective information you have received.
Plan: Finally, this section outlines the patient's future plan, including future sessions, referrals, and any changes made to the treatment plan.
As you can see, the SOAP format is a useful and intuitive way of organizing progress notes. Regardless of the number of massage therapy customers that your practice has, utilizing the SOAP note template is guaranteed to improve your workflow, productivity, and overall communication.