SOAP Notes for Chiropractic Template
Check out this high-quality SOAP note template for your chiropractic practice. You can support your clients and ensure that you effectively record all relevant health information.


What is a chiropractic SOAP notes template?
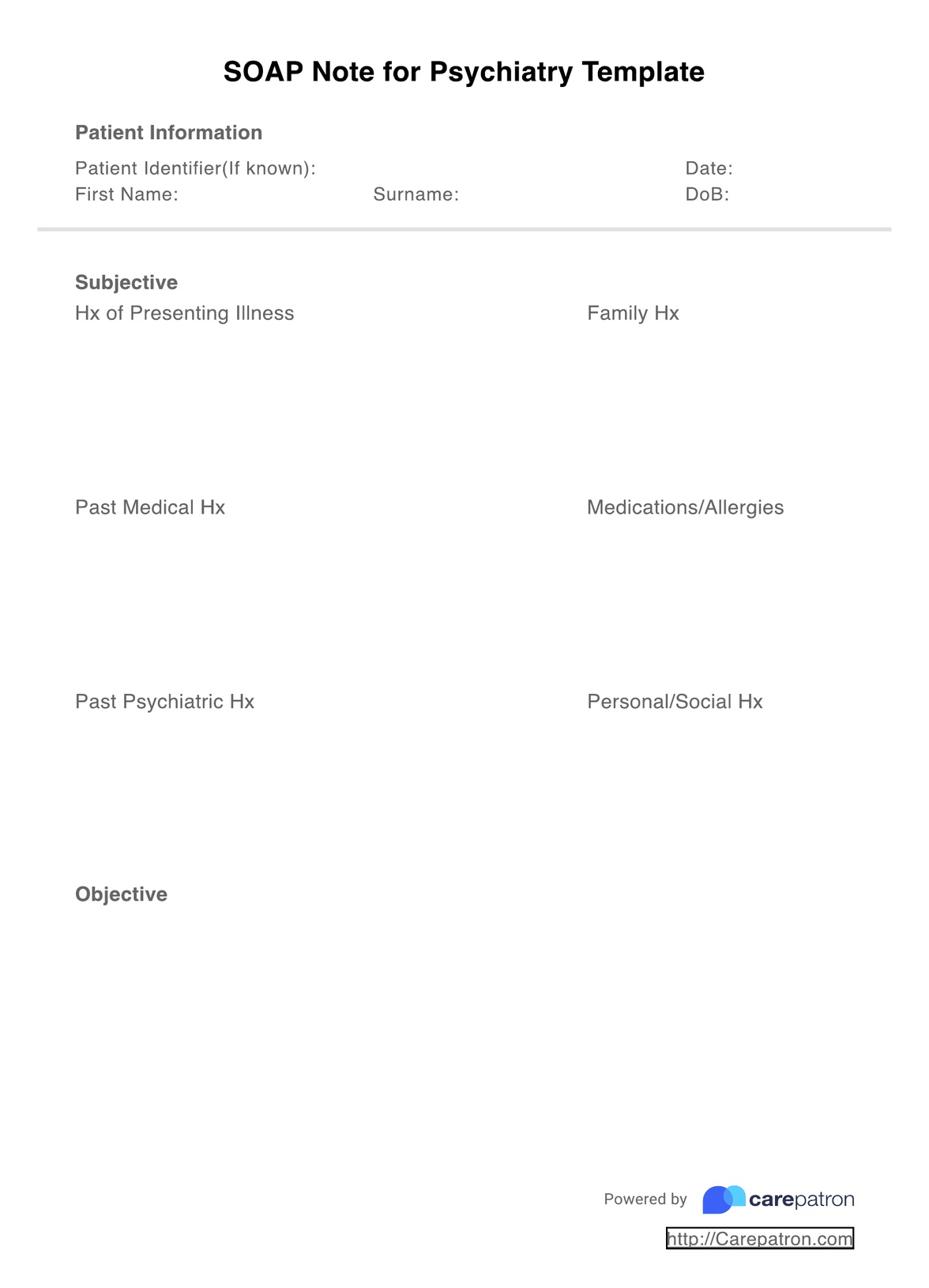
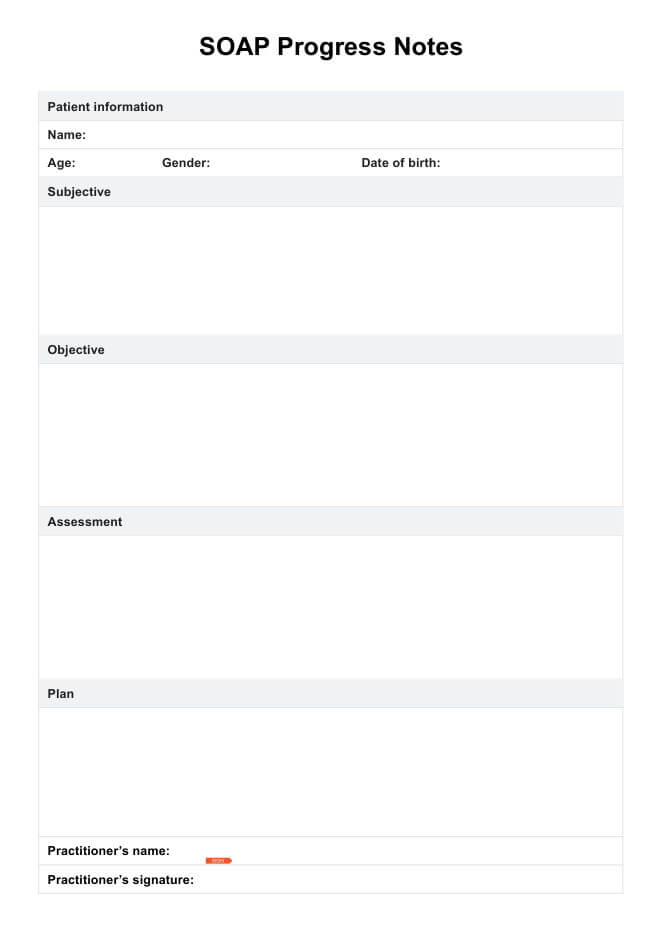
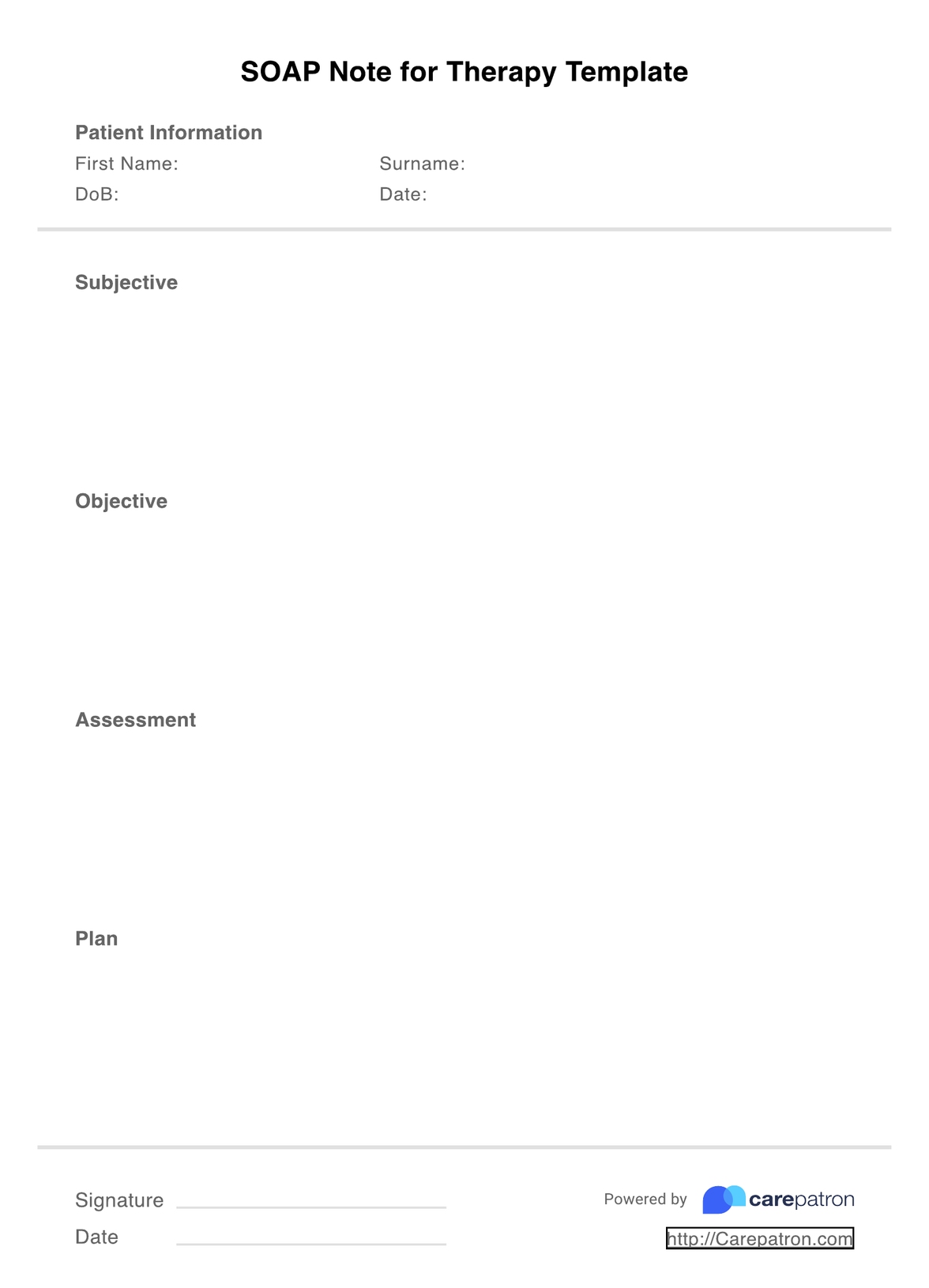
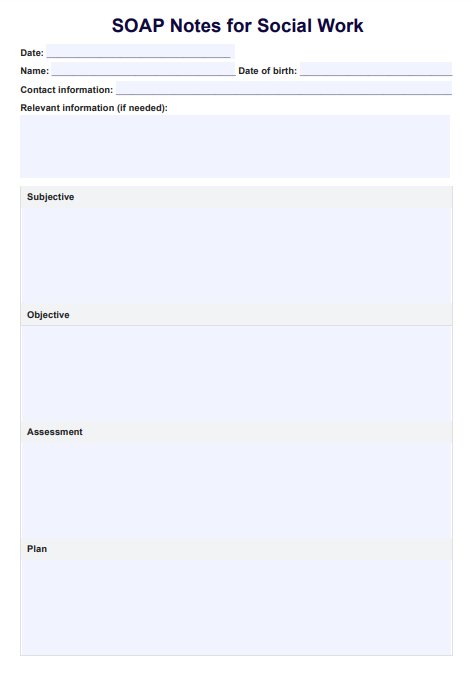
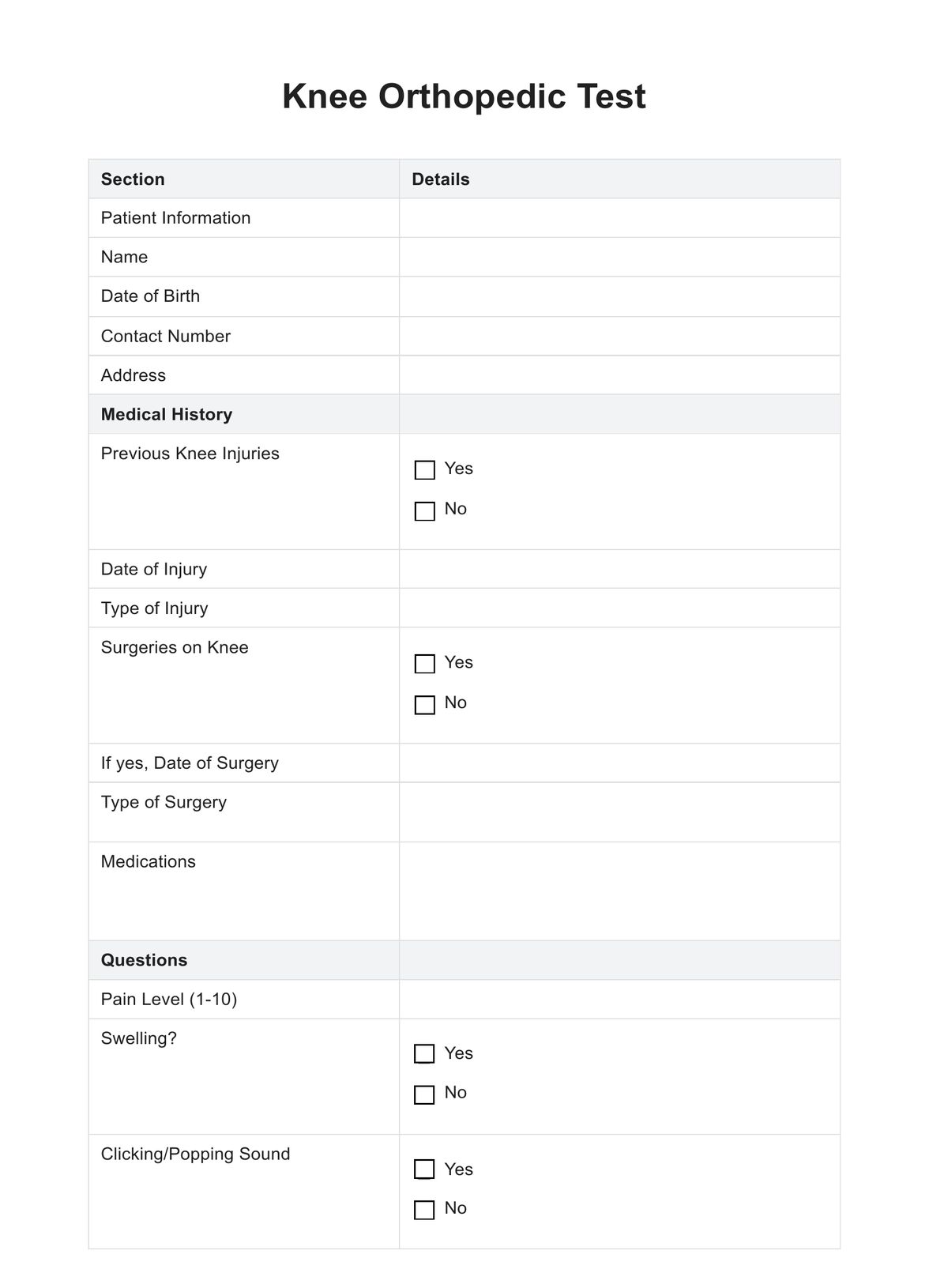
SOAP notes are a widely used clinical documentation method among healthcare providers that enables health professionals to assess clients broadly and work towards the highest-quality treatment possible. SOAP means Subjective, Objective, Assessment and Plan, four important sections that make up a comprehensive SOAP note.
For chiropractors, using chiropractic SOAP note templates is an excellent way to ensure you keep track of client health and implement effective exercises and manipulations that address the root causes of client concerns. These are the best ways to alleviate pain and significantly improve the condition over time within your chiropractic practice.
Sometimes, capturing all the essential information needed can be tricky without compromising on time efficiency. SOAP note templates are designed with this exact need in mind, and they can help boost simplified workflows for chiropractors. You can represent the client's goals, wants, and desires without spending much time on planning. SOAP notes outline your critical information, including the subjective, objective, assessment, and plan sections, which are crucial for developing an effective treatment plan.
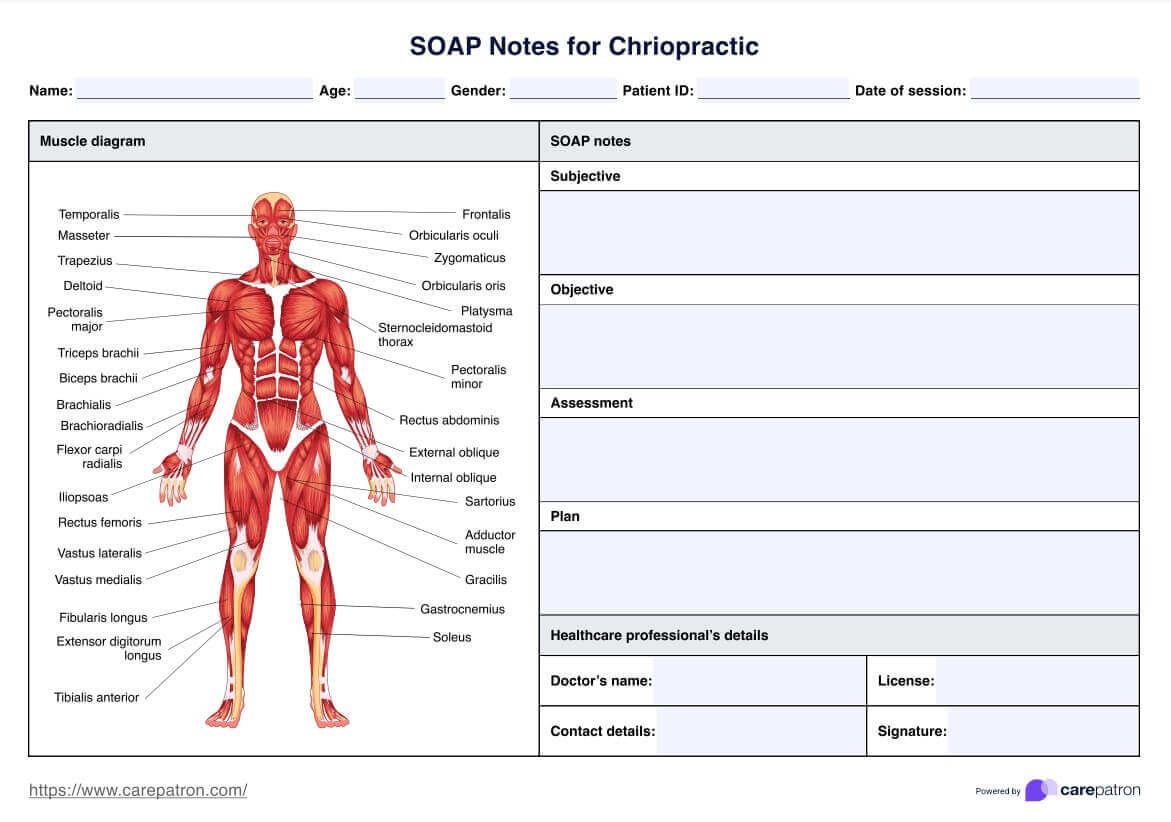
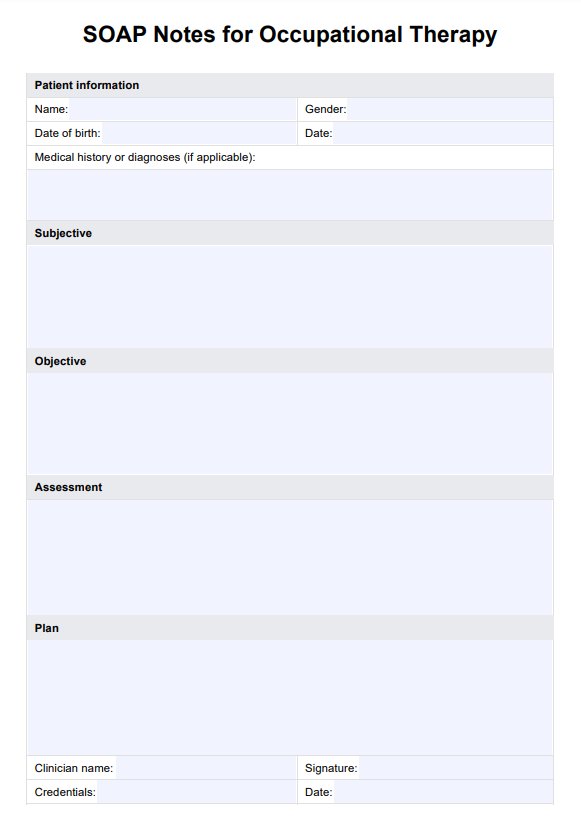
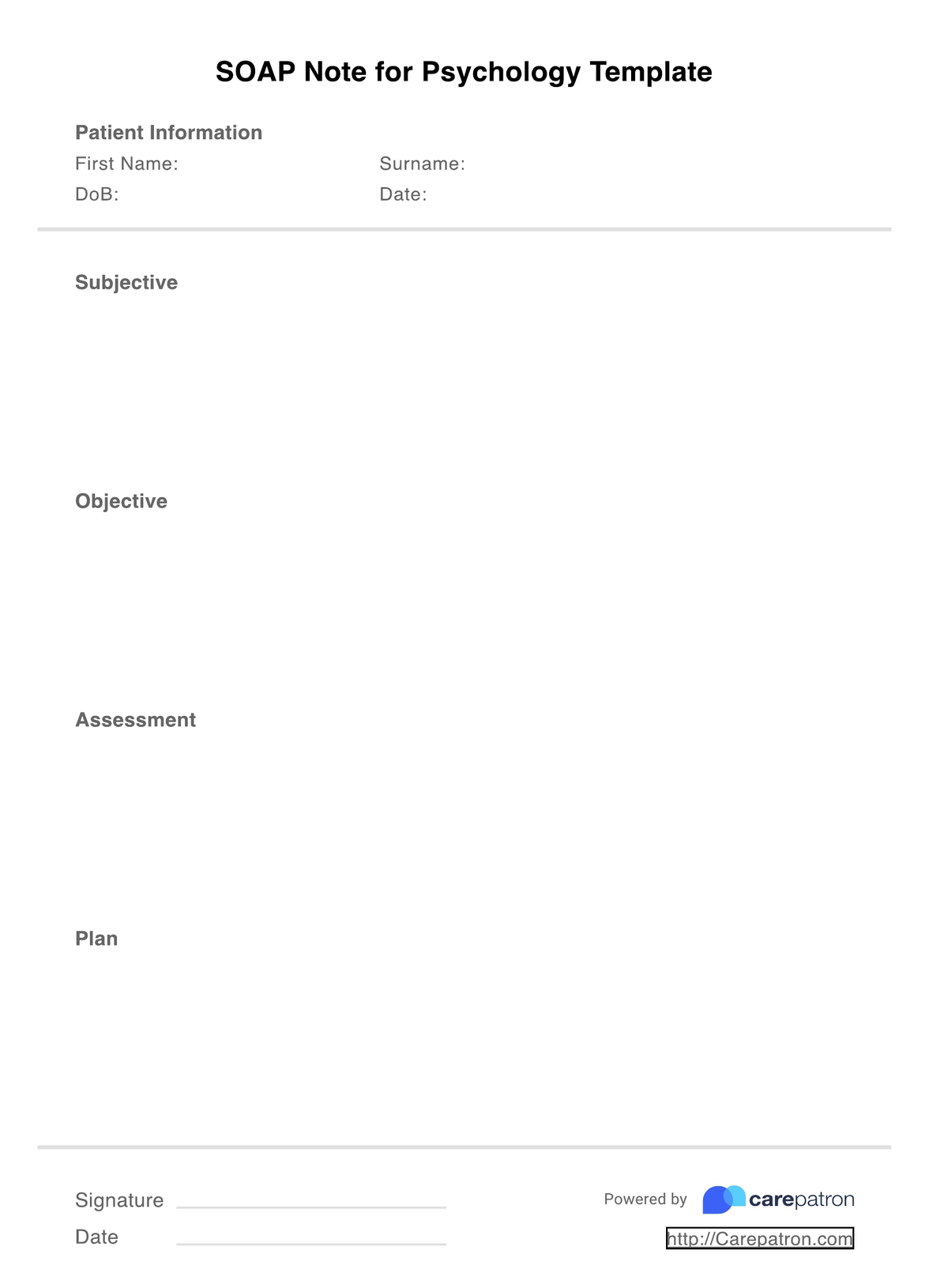
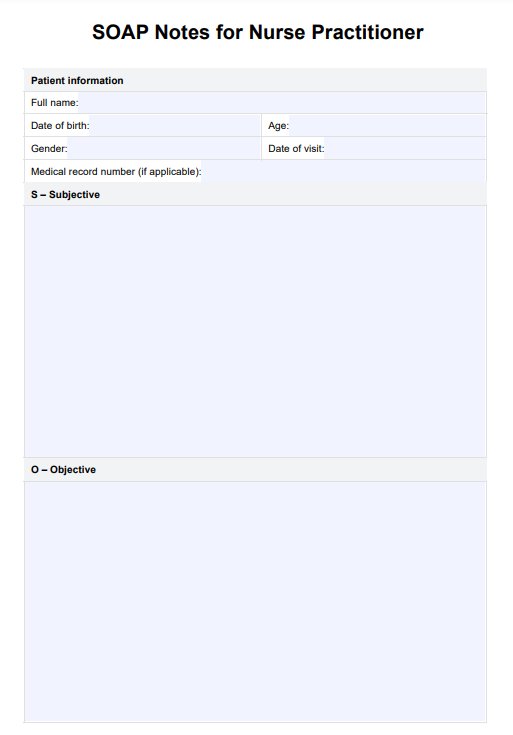
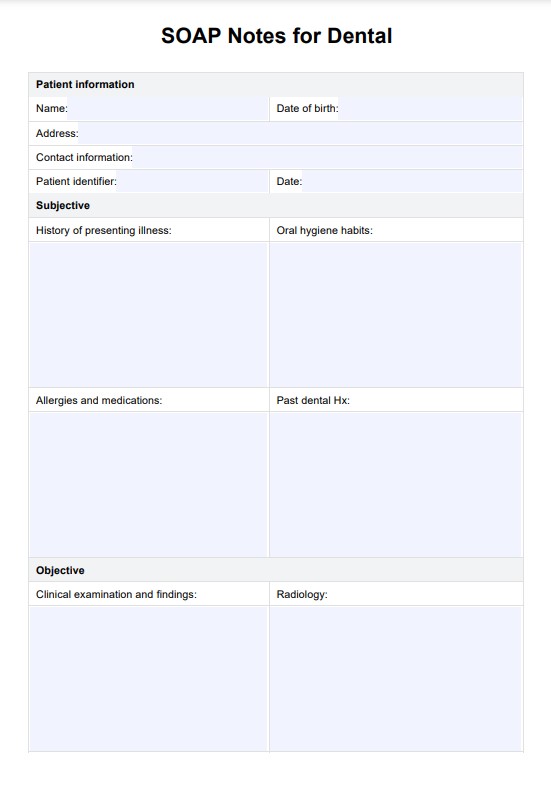
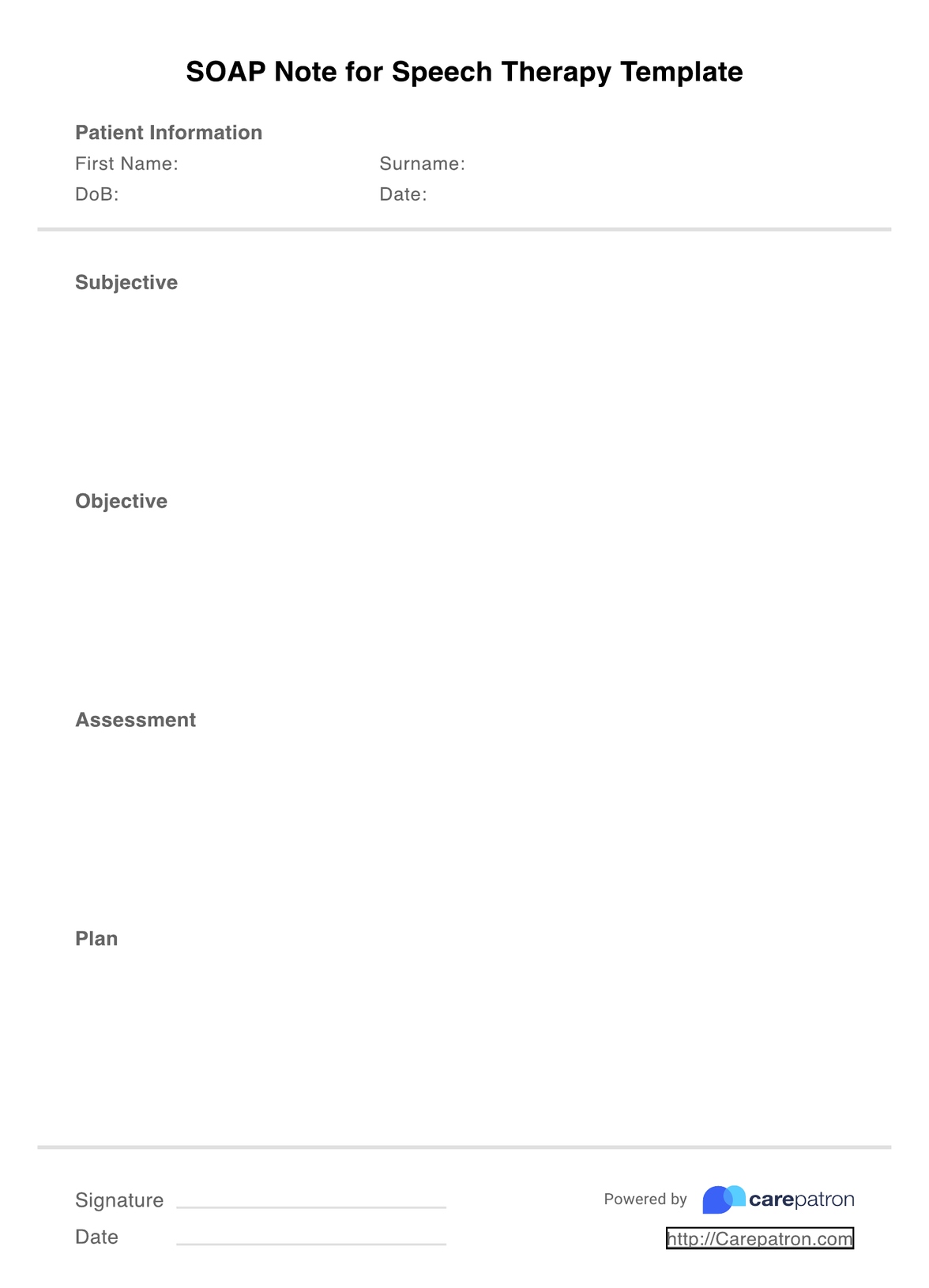
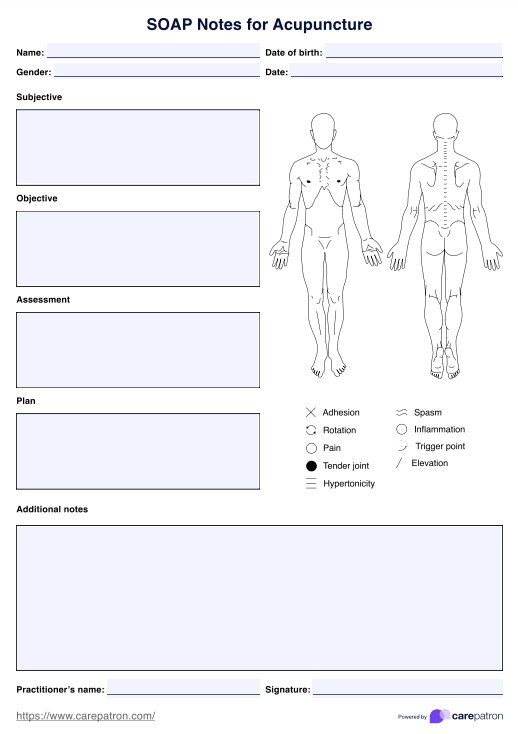
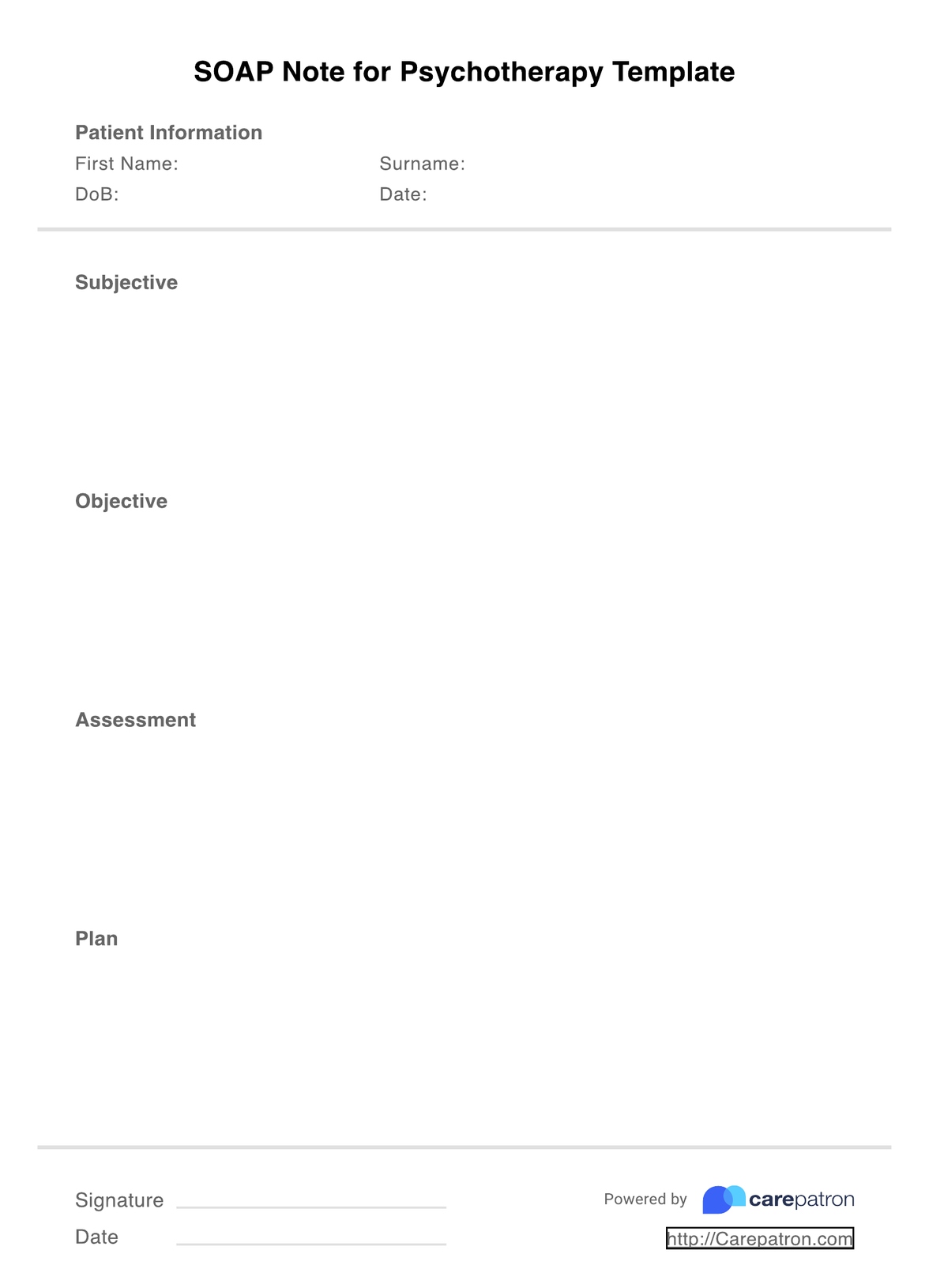
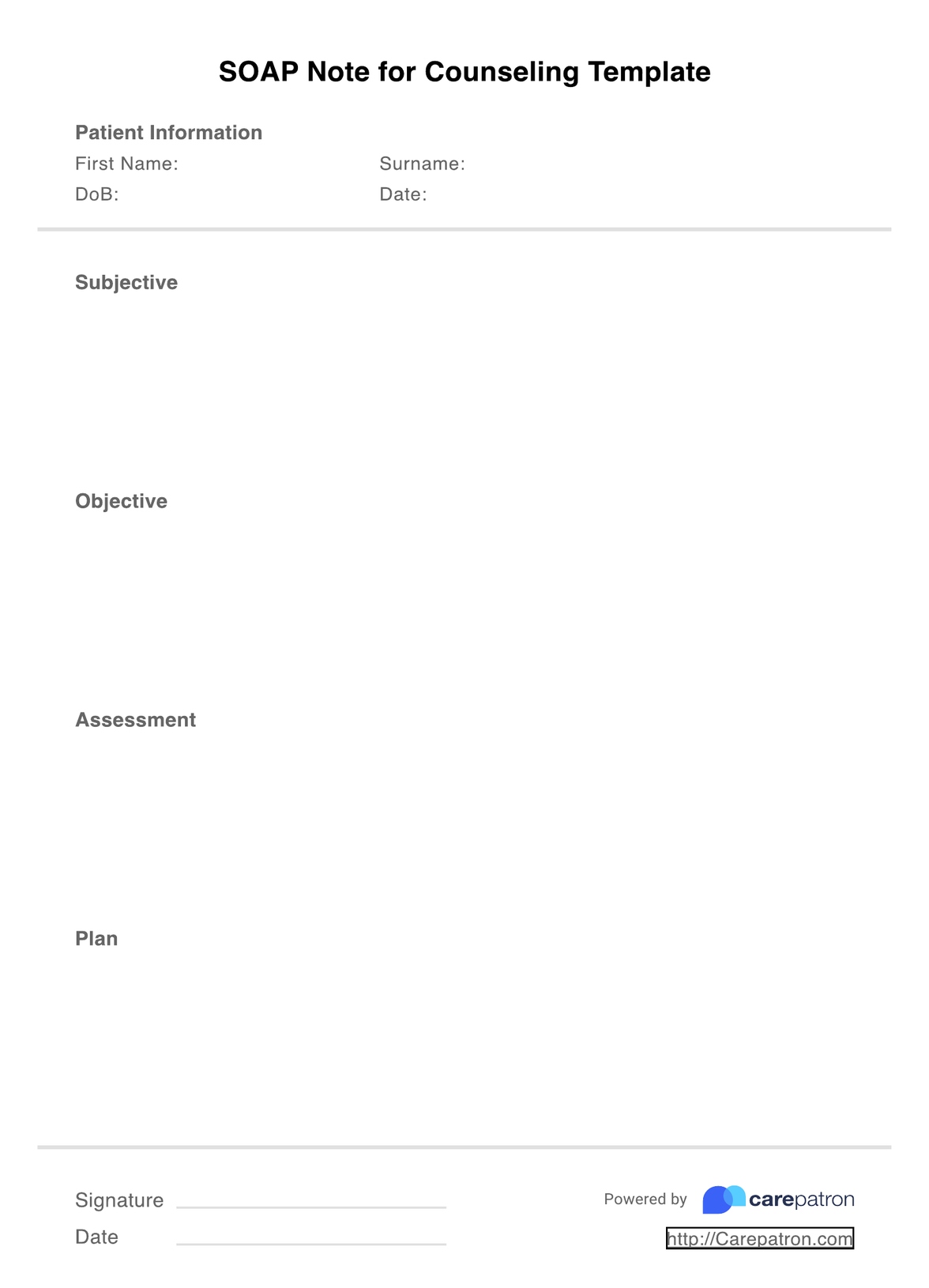
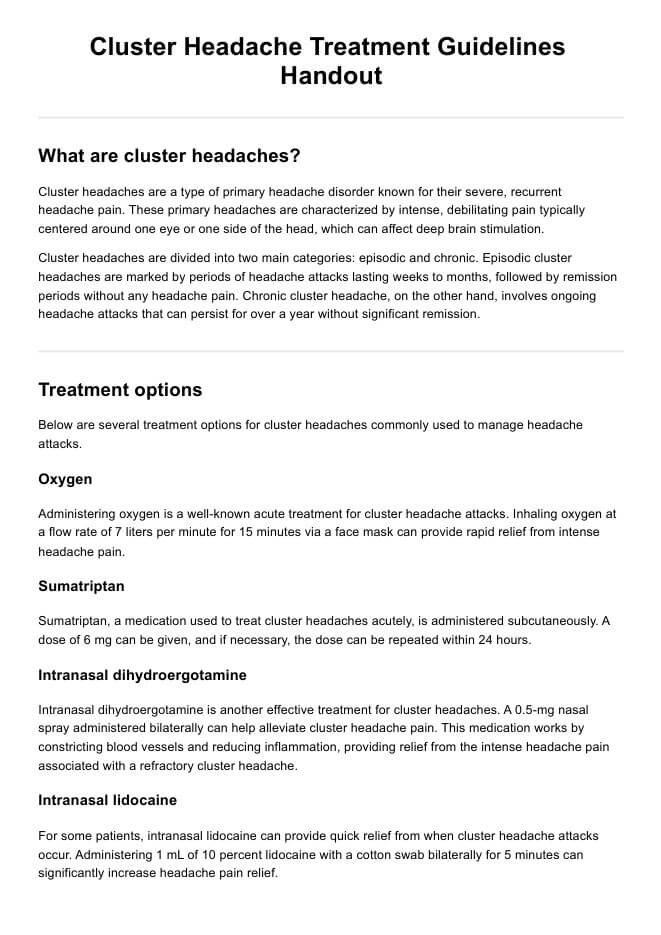
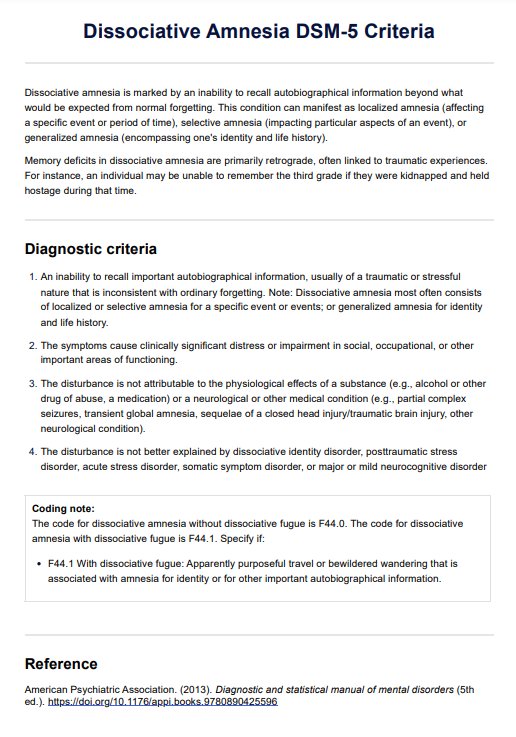
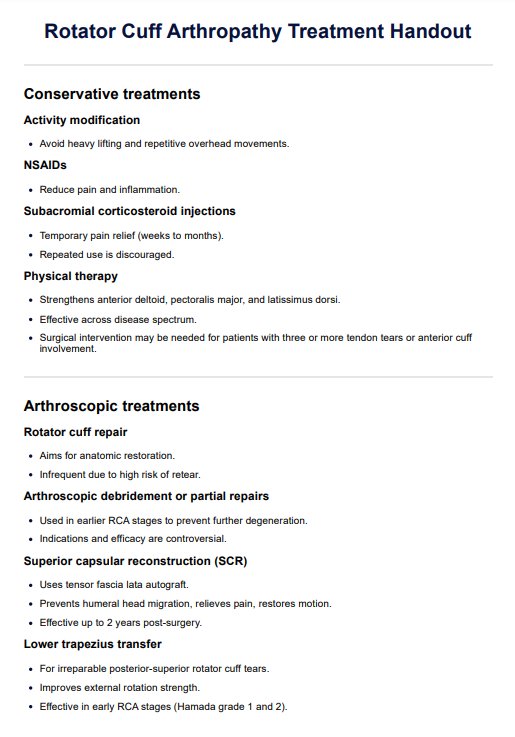
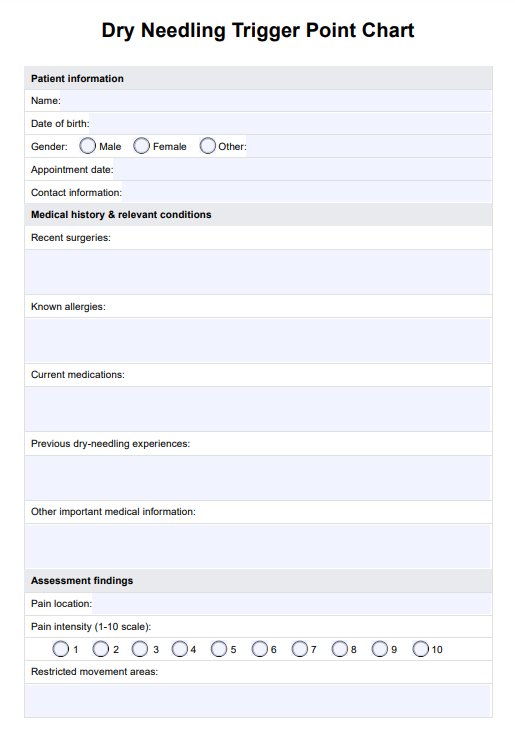
SOAP Notes for Chiropractic Template
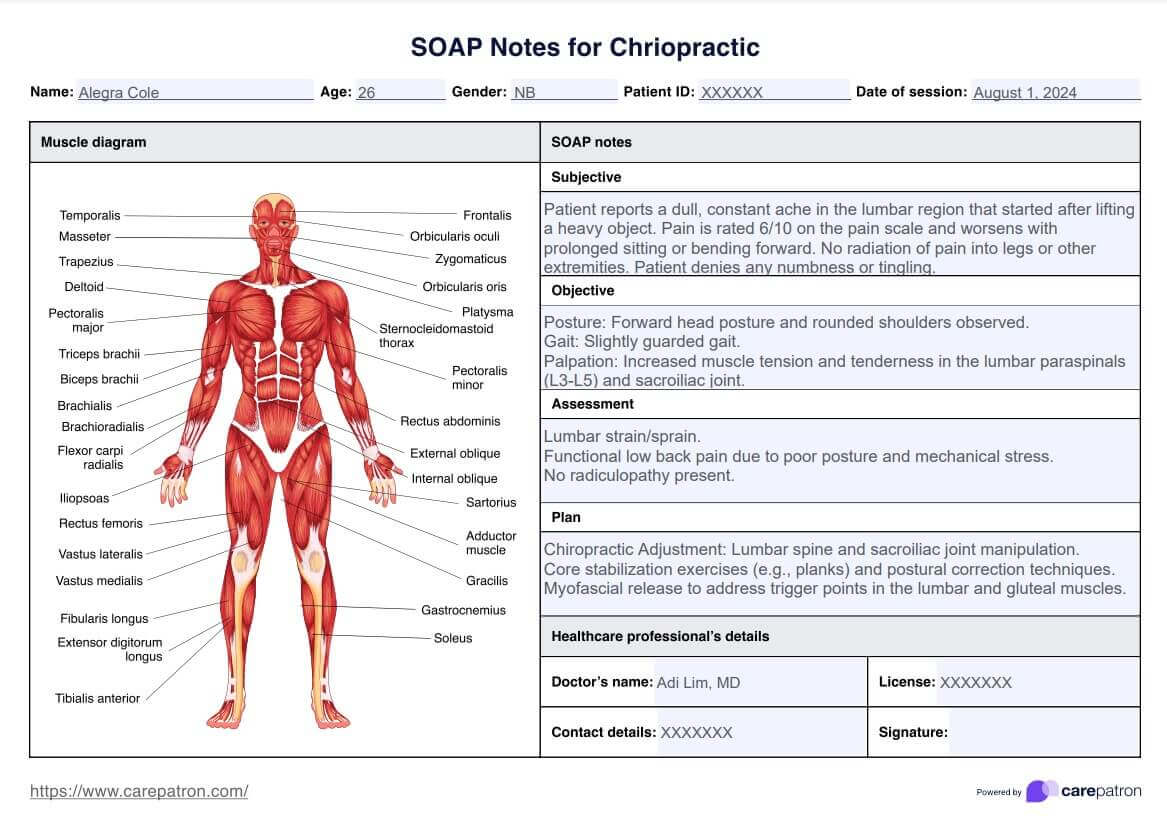
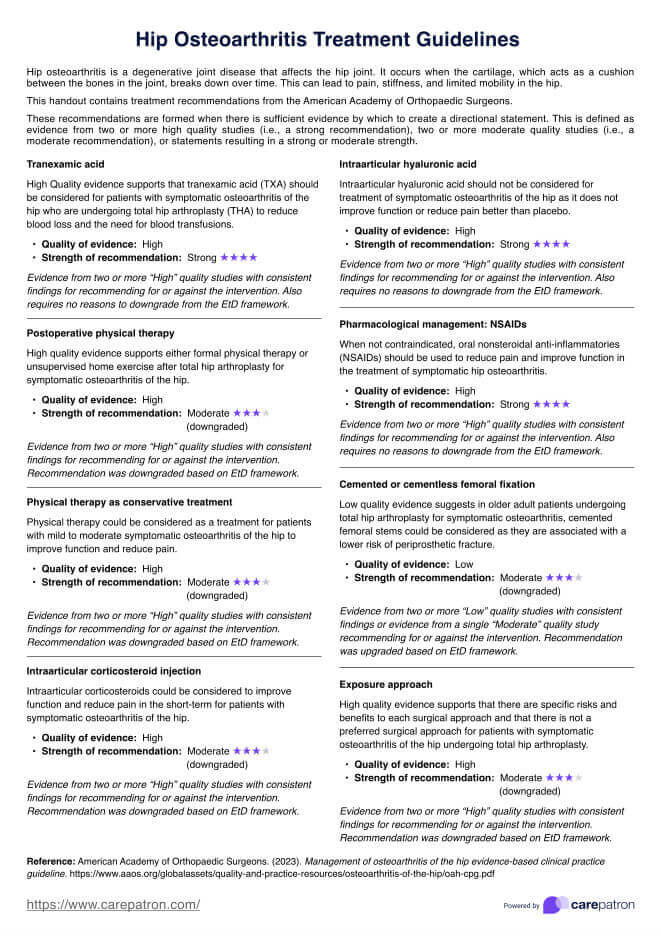
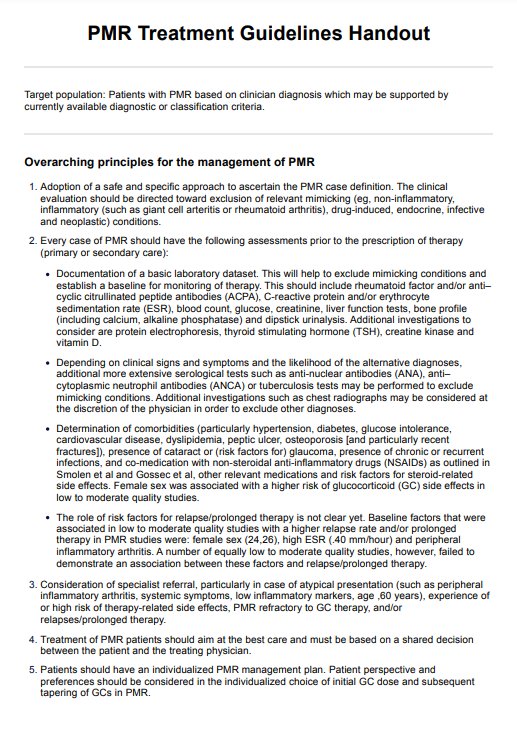
SOAP Notes for Chiropractic Template Example
How to use this SOAP Notes for Chiropractic Template
Chiropractic SOAP notes cover four main sections, and their format is super easy to use across different health contexts and professionals. Here's how to use our template:
Step 1: Download the PDF template
Before you begin, download the template on your preferred note-taking device. This takes a few seconds, and once it's complete, you should open the PDF in your reader software to make the necessary changes to it.
Step 2: Fill out your credentials
The next step is to enter the date of your session with the client, their name and ID (if applicable) and other information. This can minimize client confusion and allow easy access to all important information.
Step 3: Complete the SOAP sections
Complete the SOAP note form by writing SOAP notes that succinctly capture all relevant information. This should include the four relevant subjective, objective, assessment, and plan sections so that any fellow chiropractor or healthcare professional can pick up where you left off. Doing so gives you a better understanding of your client or patient's condition and creates a solid foundation for the treatment plan. Chiropractic practices benefit from complete SOAP notes as they ensure continuity of care.
Step 4: Sign the document
End the SOAP note by signing the document at the bottom of the page. This works towards authorizing the note; in many states, this is enforced within the legislation.
Step 5: Securely store your SOAP notes
After you're happy with your SOAP note, be sure to upload it using secure, HIPAA-compliant software. This will protect your patient information and maintain a high level of security against potential data hacks.
Who can use this chiropractic template?
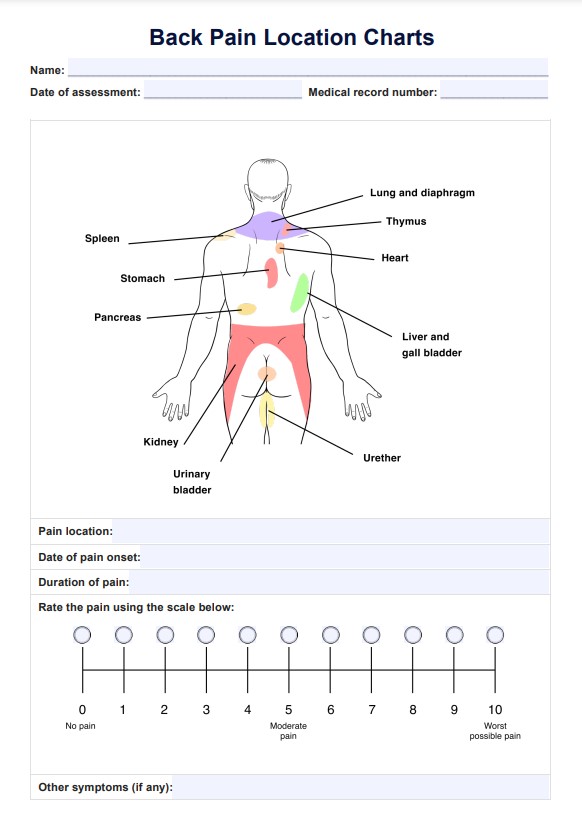
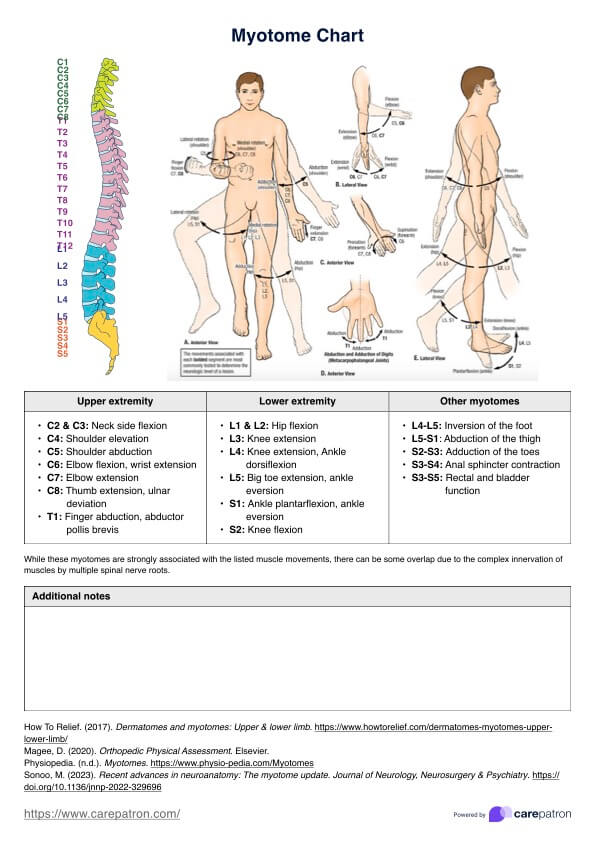
Chiropractors typically fall under the definition of health professionals who assess and treat conditions that pertain to bones, muscles, and joints. If your line of work is within the musculoskeletal area and neck pain fits within these defined terms, you will almost certainly benefit from using chiropractic SOAP notes and their templates.
Chiropractors from different fields will also find the universal SOAP note format useful, with these including:
- Vitalistic chiropractors: Those within the traditional umbrella of alternative chiropractors can use these notes to achieve high-quality health outcomes.
- Non-vitalistic chiropractors: Even those who practice through the less common non-vitalistic type will benefit from SOAP notes and being able to use them in conjunction with modern medicine.
Both assistants and qualified chiropractors can also utilize SOAP notes to ensure that all problem areas are identified, all manipulations are recorded, and exercises are given. The client or patient's progress and response to these should also be noted to ensure that each session builds upon the progress of the previous, with SOAP notes designed to increase the effectiveness of this ritual. The content of the four SOAP note sections will differ between each chiropractor, which is perfectly fine, so long as you cover all bases and follow the standardized structure.
Benefits of using the chiropractic SOAP note template
In addition to their usefulness, there are various benefits to using chiropractic adjustments and SOAP note templates, including the following points.
Effective management
With SOAP notes, you can organize all relevant information to be accessible from one place without worrying about managing each SOAP note. You can standardize your notes and have consistency across your records, leading to faster chiropractic SOAP notes.
Save time
Naturally, this means you can also save time on creating, drafting, and editing your templates, as the outline is already completed. This way, you know exactly what areas to expand upon, and there's a dedicated space for each important characteristic, so you're only spending time on the absolute essentials.
Greater communication
Because SOAP notes provide a simplified format, you can ensure that you note all important information highlighting obvious client concerns. You can have an overview of all potential contributors to client pain and develop a more effective treatment plan that addresses each issue. This higher form of communication means fellow chiropractors and other healthcare providers and professionals can benefit from your notes, especially regarding referrals.
Meaningful client relationships
SOAP notes are designed to represent the client's condition, goals, and responsiveness to treatment, meaning they place clients at the forefront of future treatment outcomes. You can work with clients and provide more holistic assessments considering their experience and health objectives.
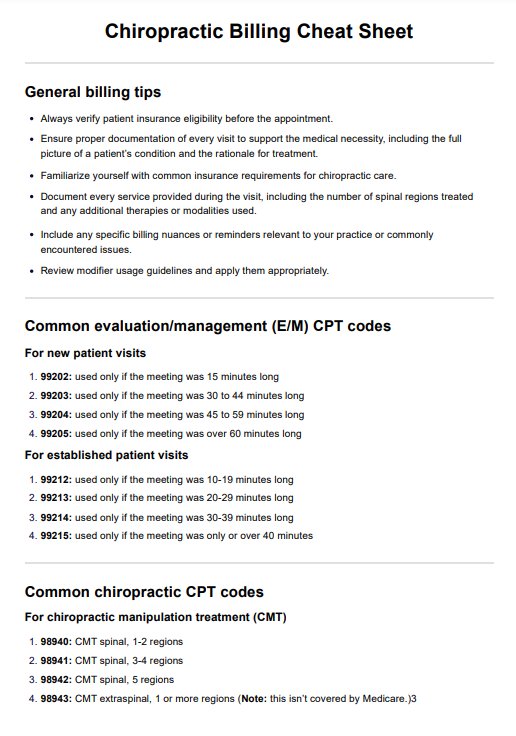
Legal and insurance
SOAP notes are also beneficial as they protect your practice against potential legal cases and can result in higher reimbursements for insurance claims. SOAP records keep track of all health interactions and medical necessity, including the equipment, medications, and treatment used. This is highly effective for safeguarding your work and ensuring that you monitor all expenses accurately.
Commonly asked questions
This is a great question. However, there is no black-and-white answer. A good rule of thumb is to stick to one to two pages, as anything beyond that is considered too excessive. Being succinct and concise is key when it comes to SOAP notes!
Yes, you can edit SOAP notes even if you've uploaded them into a system. However, for record-keeping purposes, make sure to sign and date each amendment.
A good SOAP note is clear, concise, and organized. It effectively captures the patient's subjective complaints, objective findings, assessment, and a plan that guides clinical decision-making and ensures continuity of patient care.