SOAP Notes for Counseling Template
A fantastic PDF SOAP note template for counseling, helping you to simplify documentation and improve clinical outcomes for your patients.


What are SOAP Notes for Counseling?
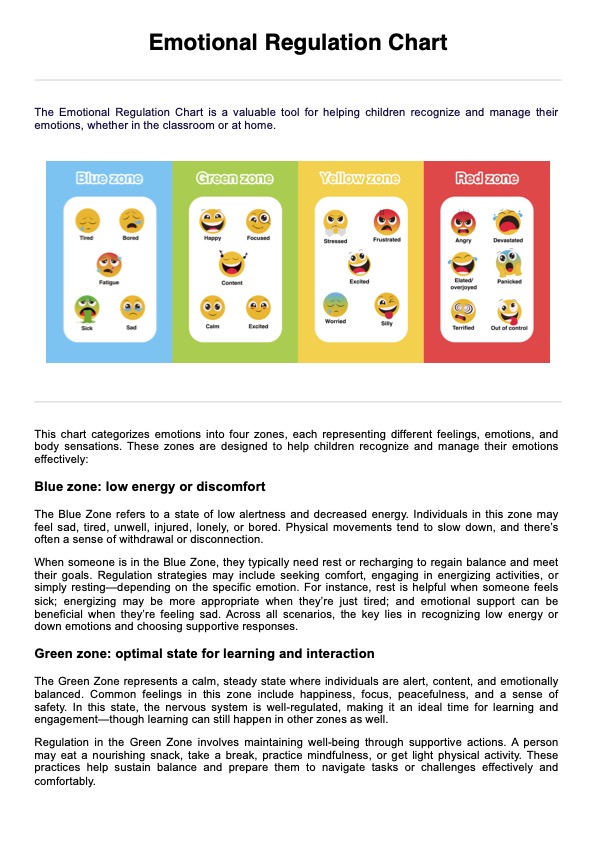
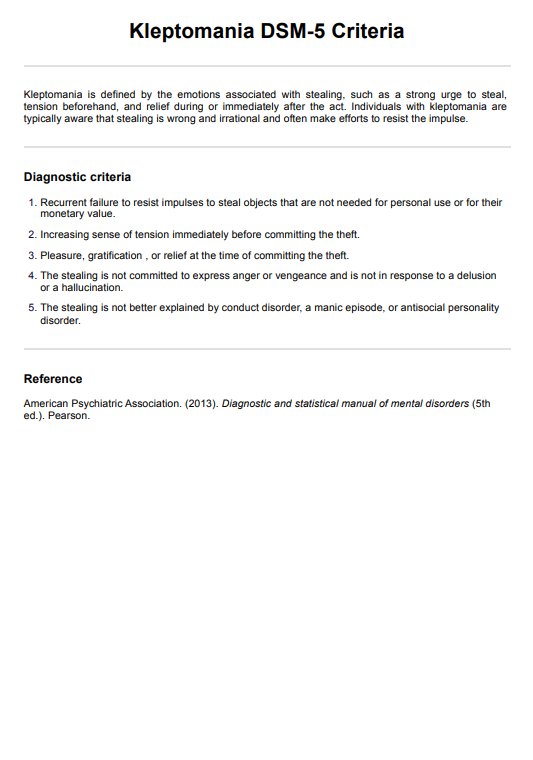
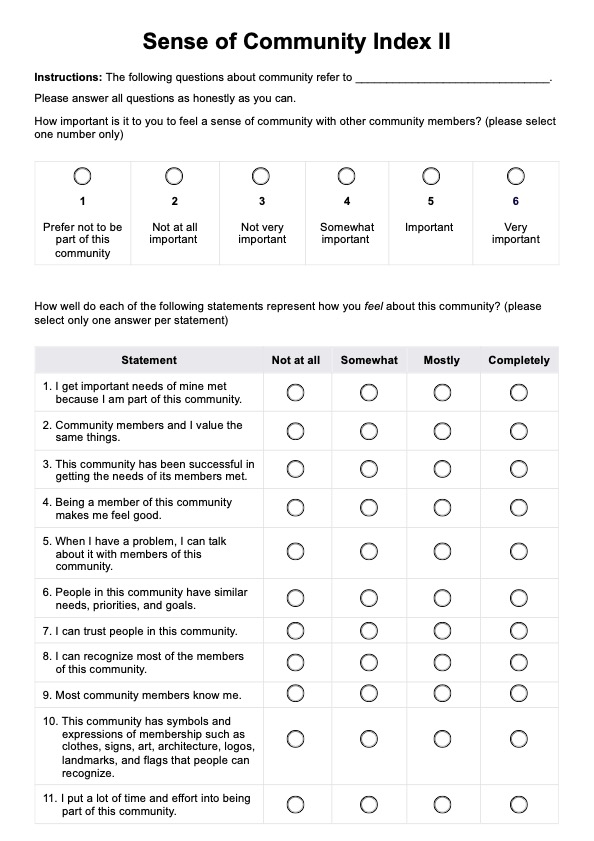
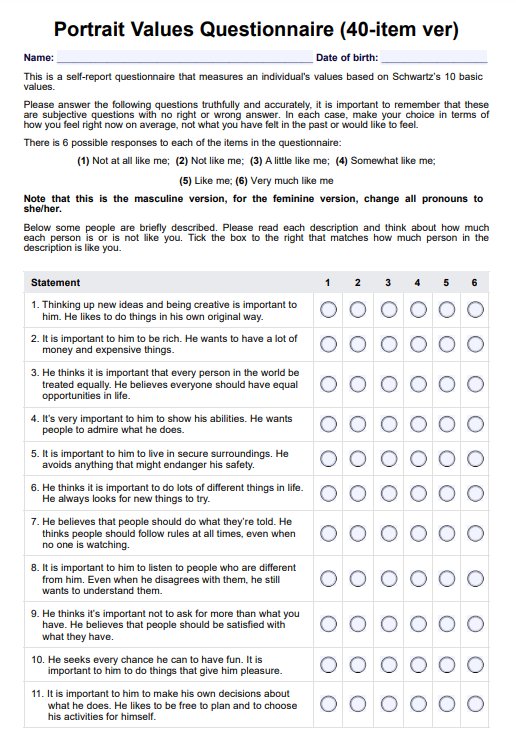
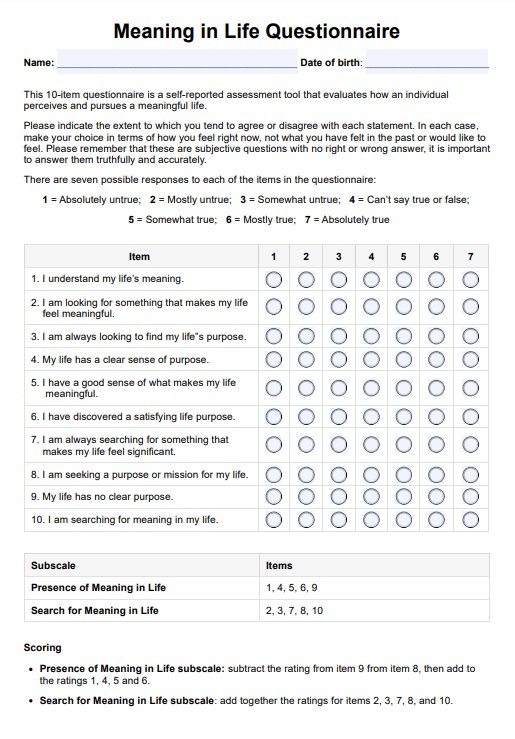
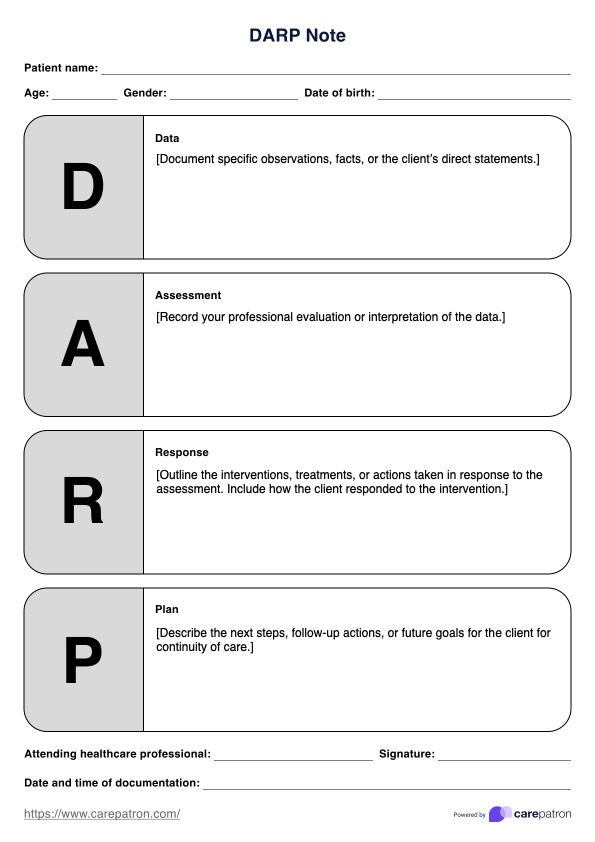
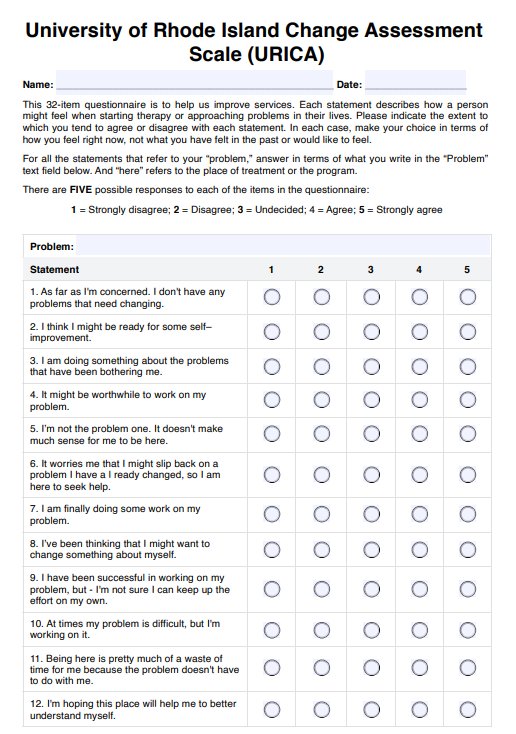
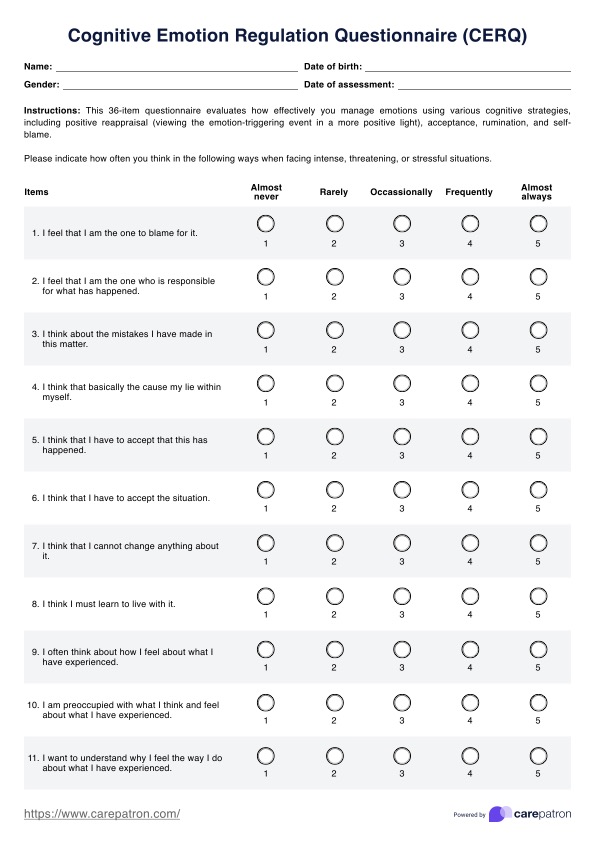
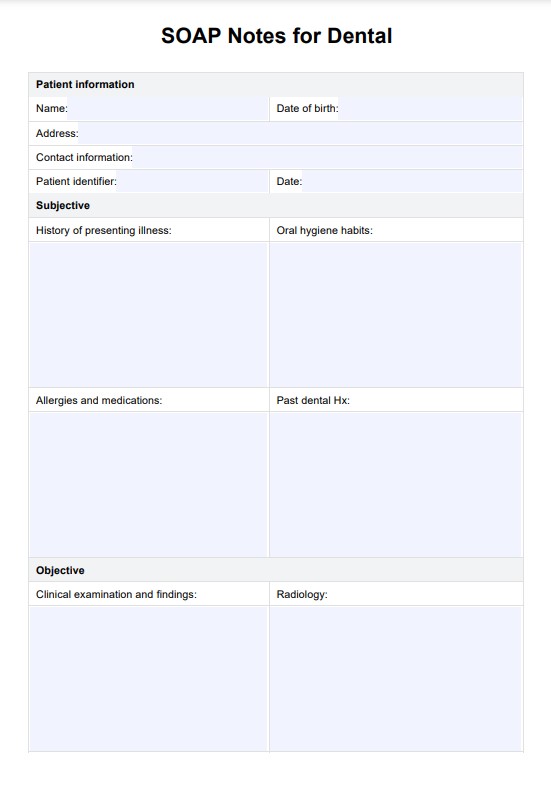
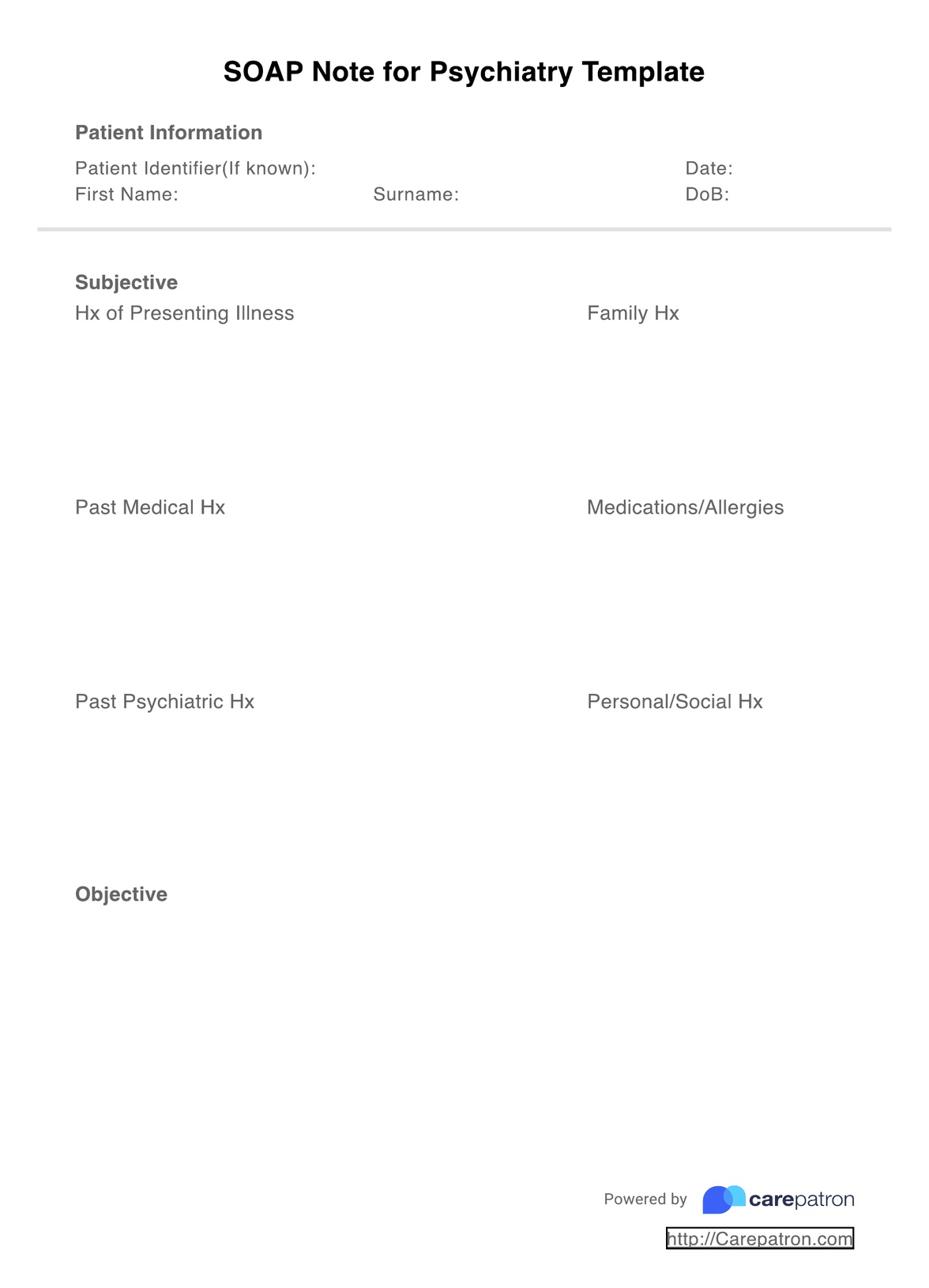
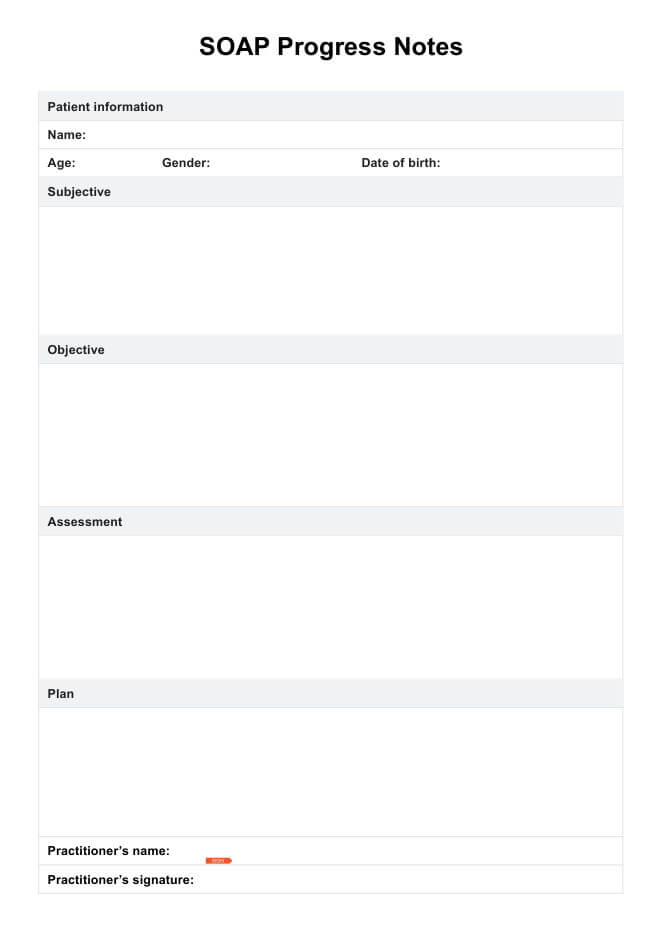
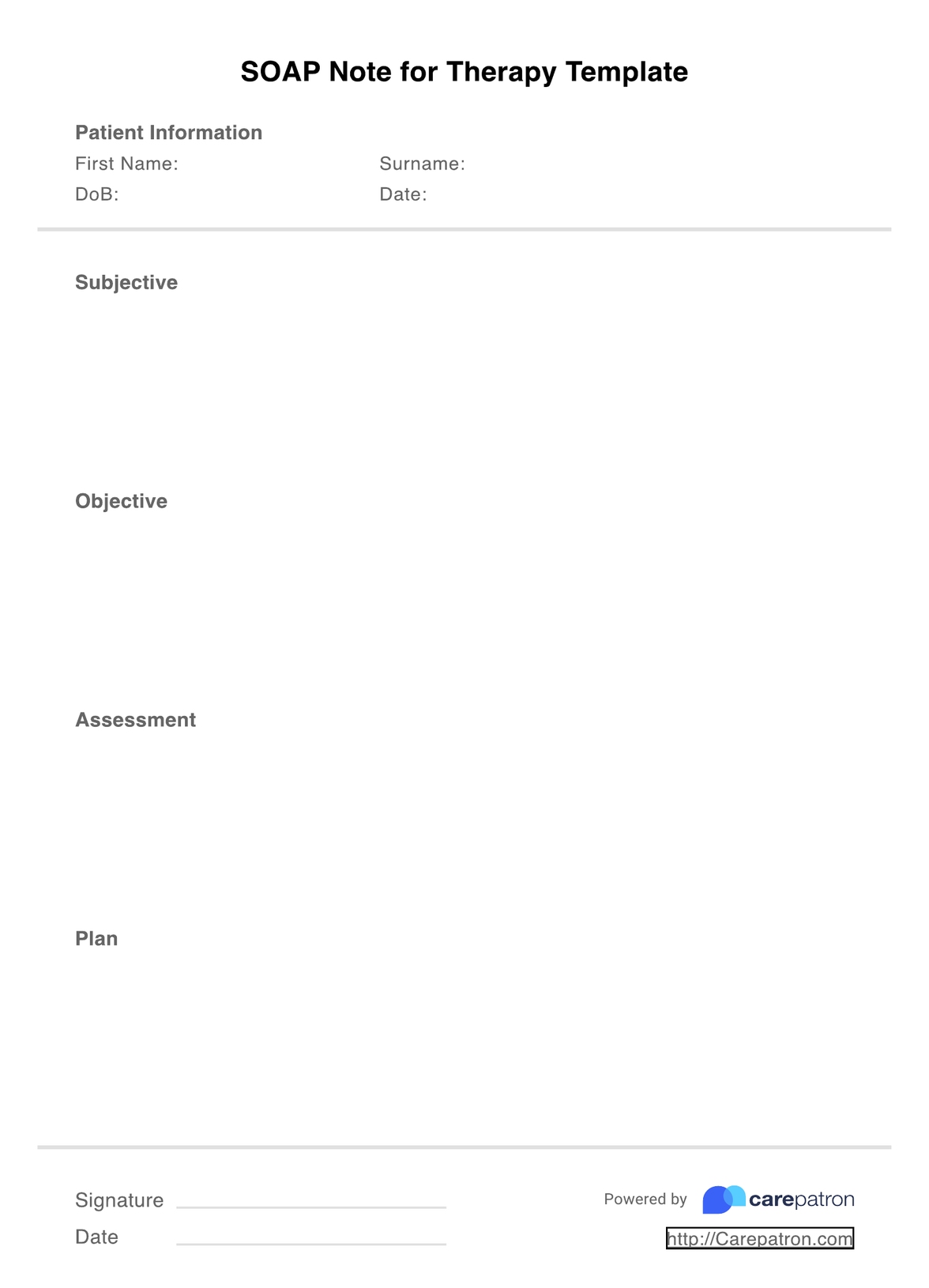
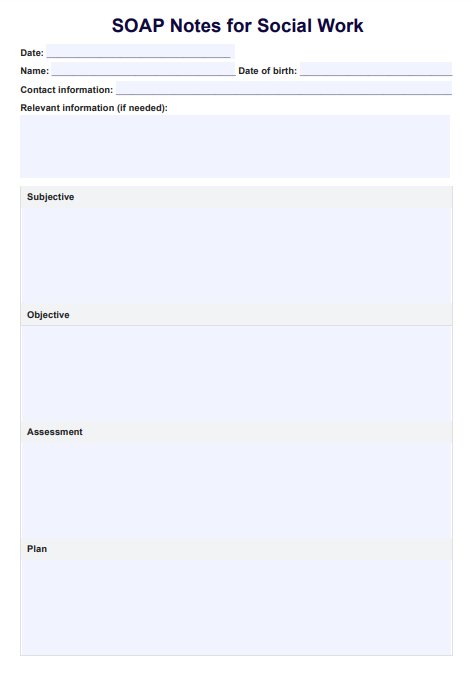
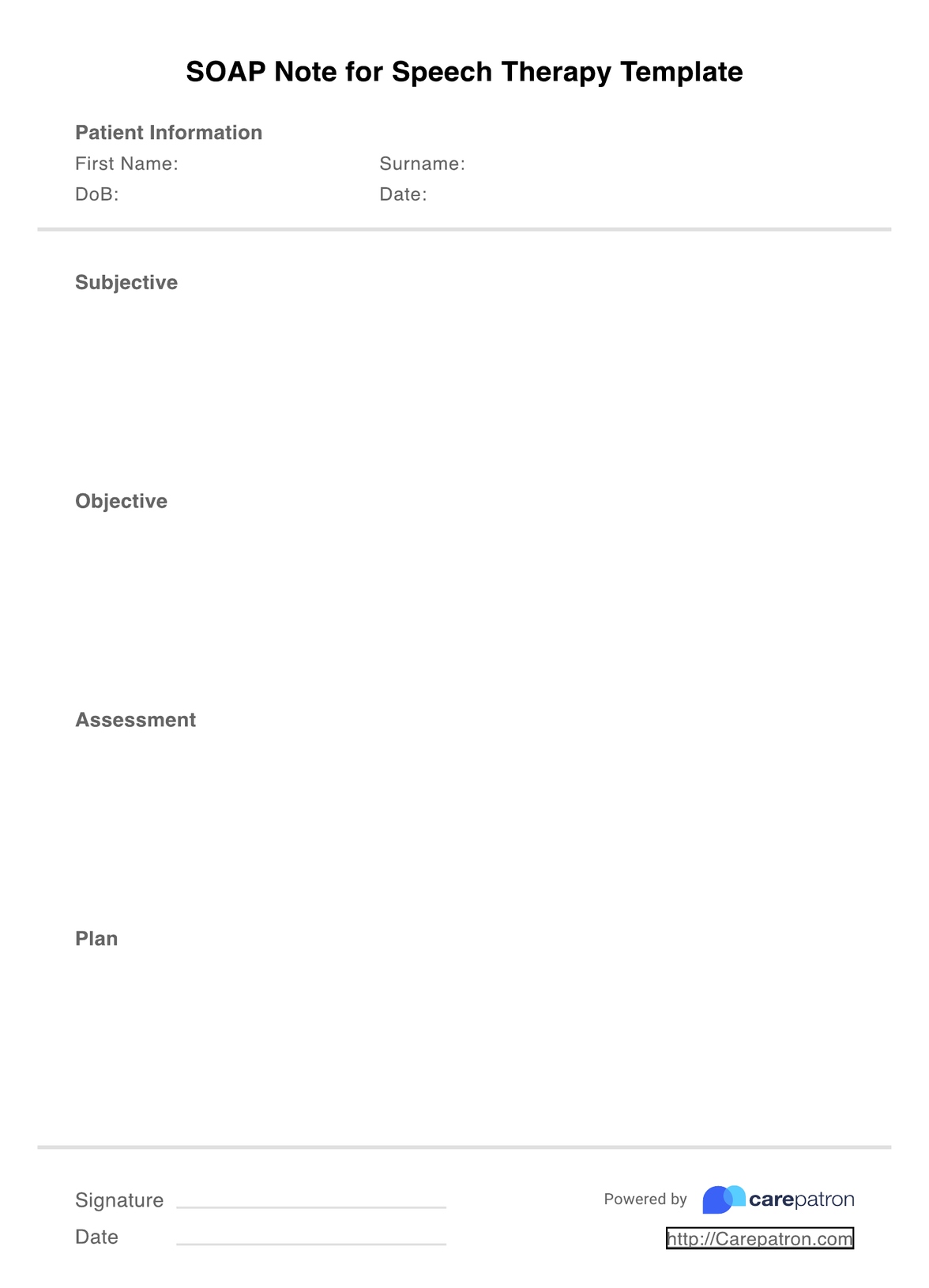
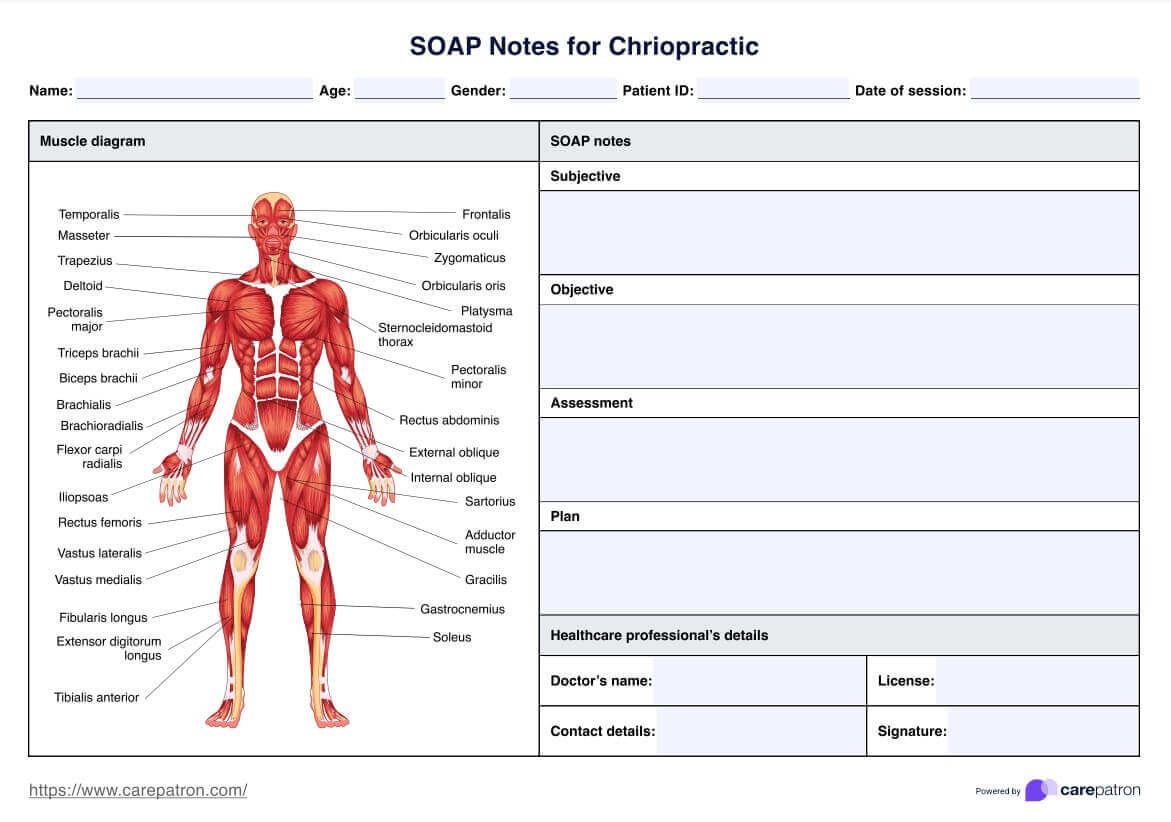
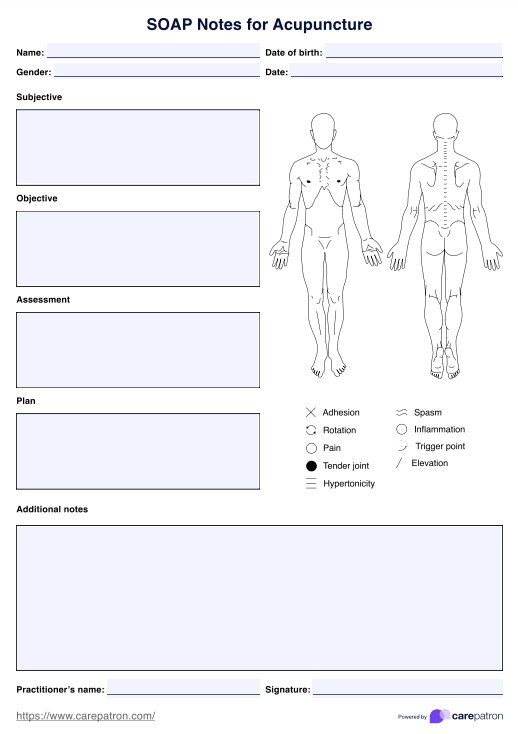
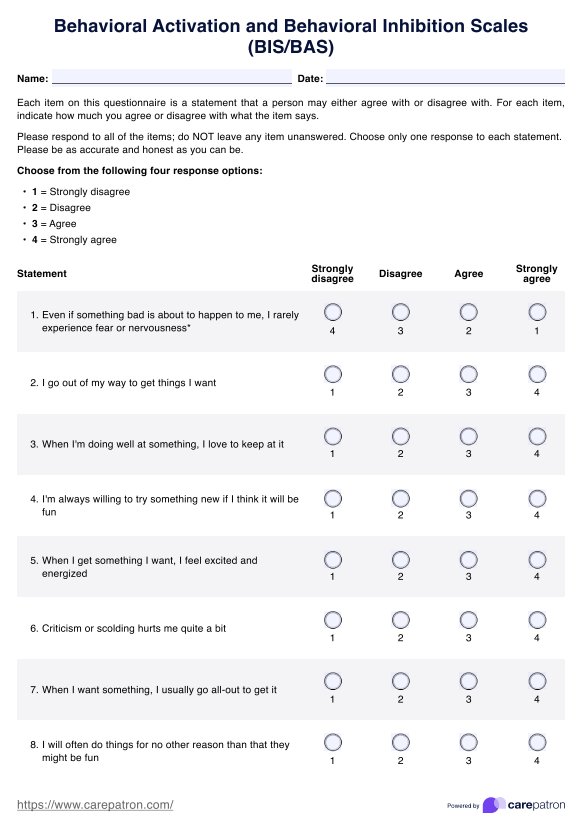
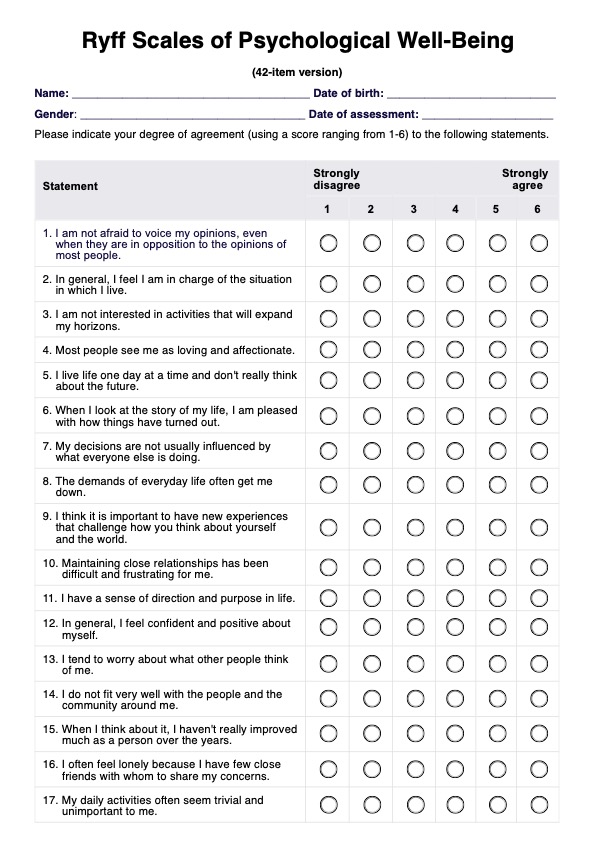
SOAP notes are a form of clinical documentation that are used by counselors to track the progress of their patients. The PDF resource that we have created is a template that will allow you to streamline your note-taking. It separates the progress note into the four relevant sections:
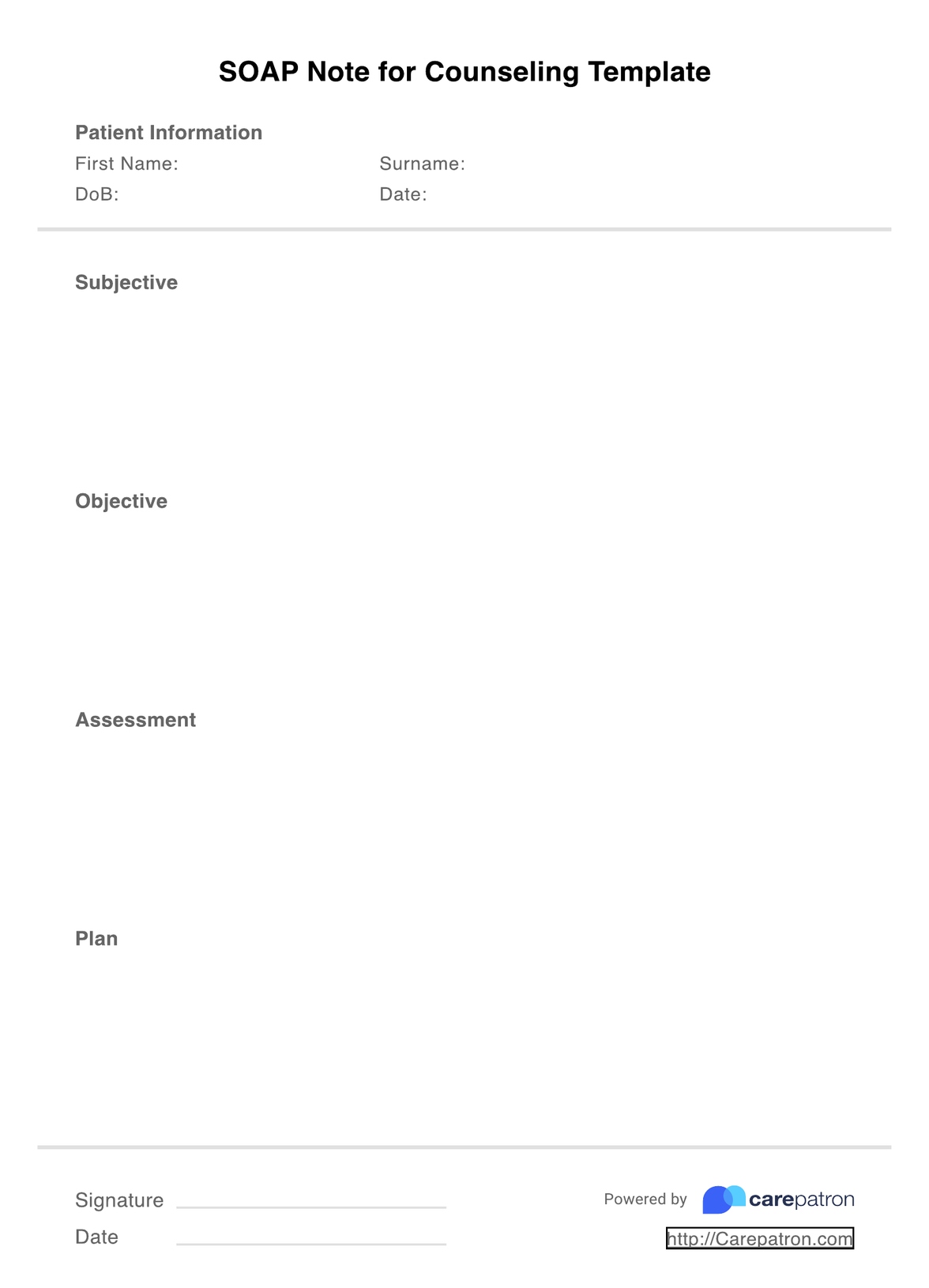
Subjective: The subjective section includes the patient’s description of their concern, including symptoms and how it is affecting their day-to-day life. This section often includes direct quotes from the patient.
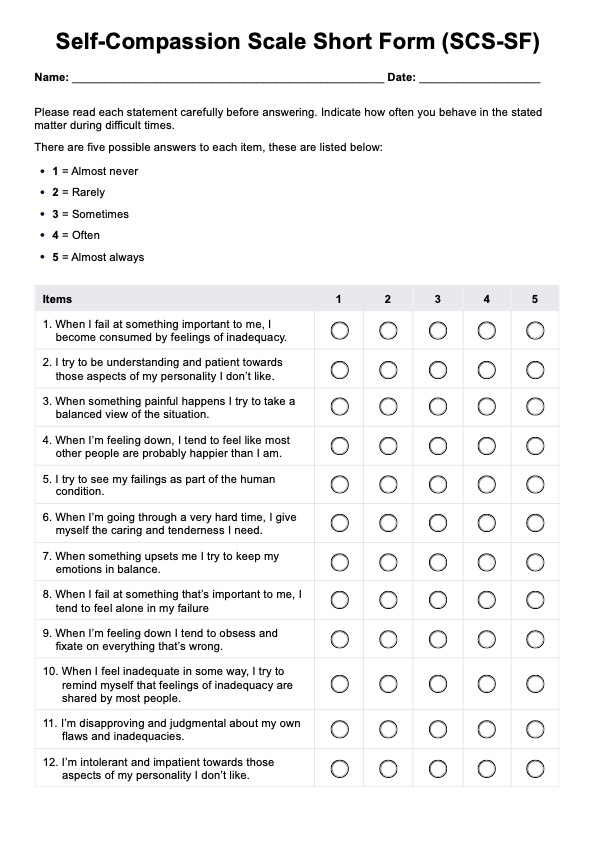
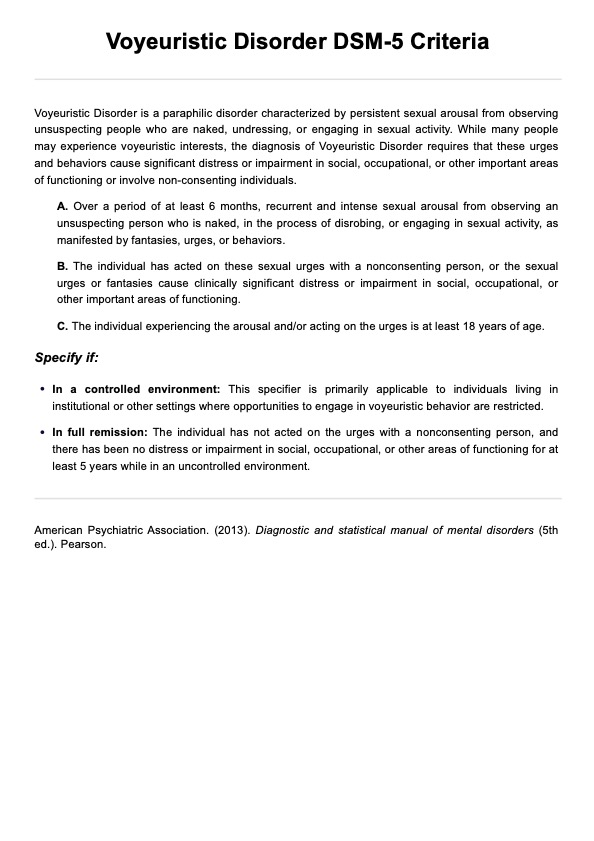
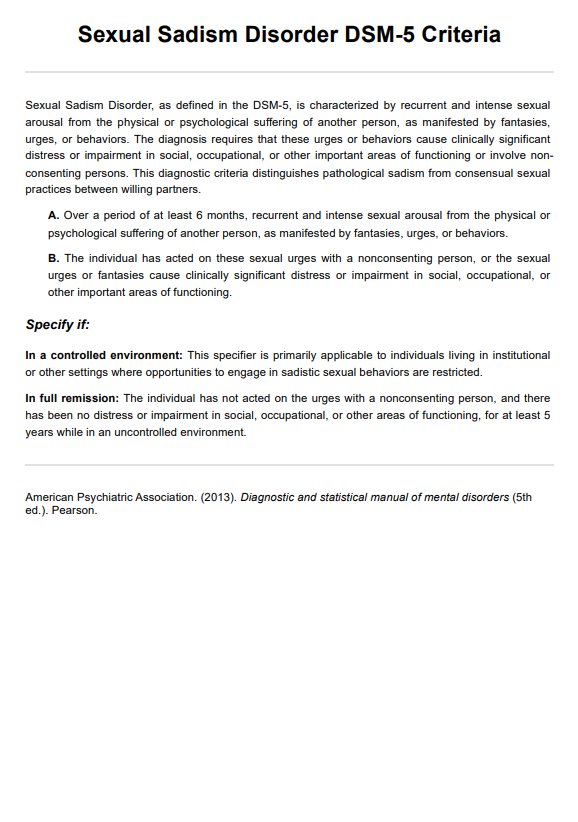
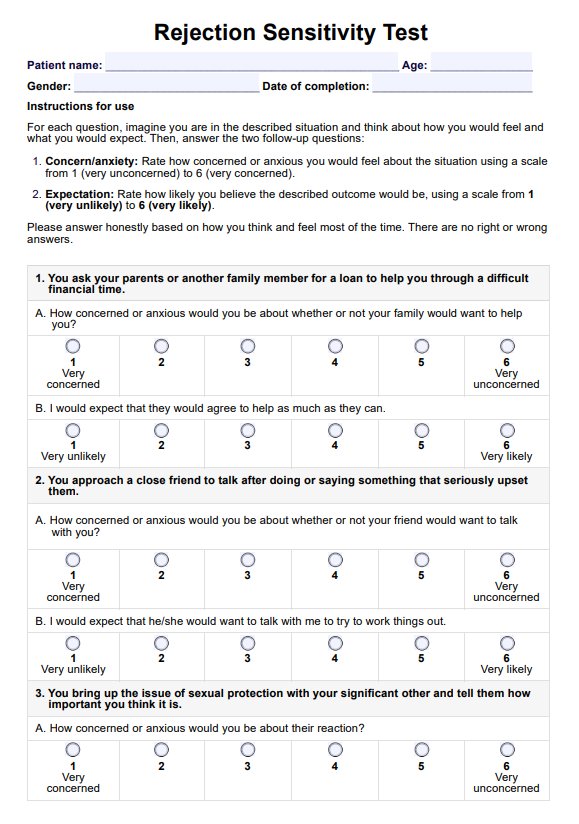
Objective: The objective section includes any tests, assessments or evaluations that you completed during the session.
Assessment: The assessment section is a synthesis of the subjective and objective information and includes an analysis or evaluation of the patient’s concern, health status, and treatment progress.
Plan: Finally, the plan outlines the future steps for the patient’s treatment, including any upcoming sessions, goals, referrals, or changes to the treatment plan.
Using a SOAP note template is one of the easiest and most effective ways you can save time on your documentation, without compromising its quality. Often, , including Carepatron, will have SOAP note (and other progress note) templates integrated into their platforms. These tools give counselors access to fantastic resources that aim to simplify their work and by doing so, save both money and time. Utilizing templates additionally ensures that your documentation is coherent and organized. Because SOAP notes are often shared between all members of a patient’s care team, keeping their structure consistent is one of the best ways to improve coordination of care.
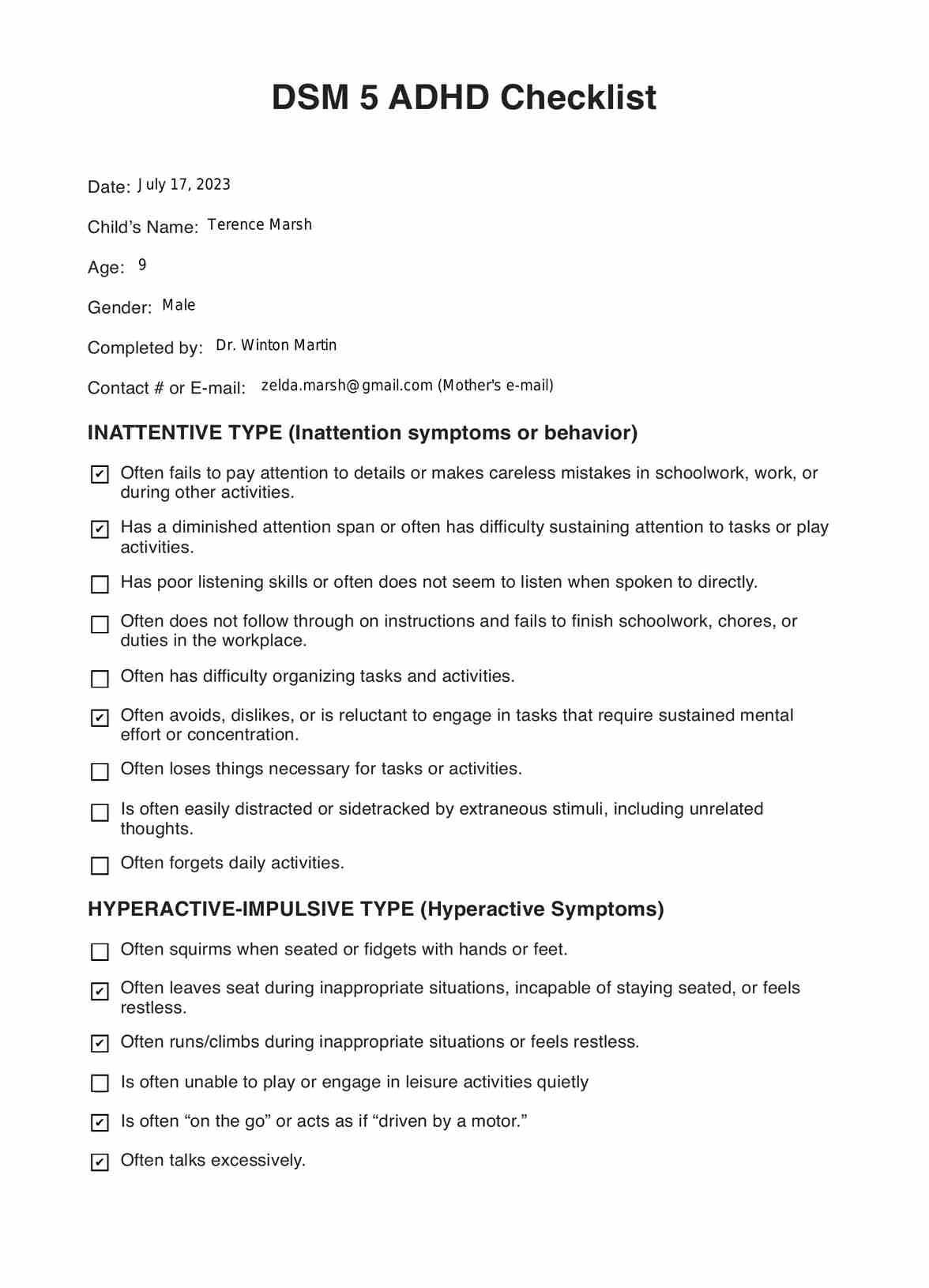
SOAP Notes for Counseling Template
SOAP Notes for Counseling Template Example
How to Use This SOAP Note in Counseling?
Regardless of whether you offer in-person or online counseling sessions (or maybe you do both!), working as a counselor requires quite an extensive amount of clinical note-taking. In addition to tracking the progress of patients, SOAP notes are used in both legal and insurance situations. So how exactly do you use our SOAP note template?
Step One: Download the PDF
First things first: in order to use our template, you need to download the PDF. This will give you viewing and editing access, allowing you to fill in the relevant sections.
Step Two: Essential credentials
Within the SOAP note, you need to include the following credentials: the date/time of the session, the patient’s name (and ID number where relevant) and your own professional credentials.
Step Three: Fill out the four sections
The four sections of a SOAP note are subjective, objective, assessment, and plan. After you have recorded the relevant credentials, you need to fill out each of these four sections appropriately. It’s important that you cover all important information without repeating yourself: conciseness is key. If you want to find out more about what exactly needs to go in a counseling SOAP note, check out this helpful SOAP note guide that Carepatron has created.
Step Four: Store your SOAP notes securely
After you have written your SOAP note, you need to store it in a safe and HIPAA-compliant manner. Using a software like Carepatron is one of the best ways you can do this. Practice management systems have electronic and physical safeguards in place that will protect your ePHI, ensuring your SOAP notes are both protected and accessible at all times.
Who Can Use This Counseling SOAP Note Template?
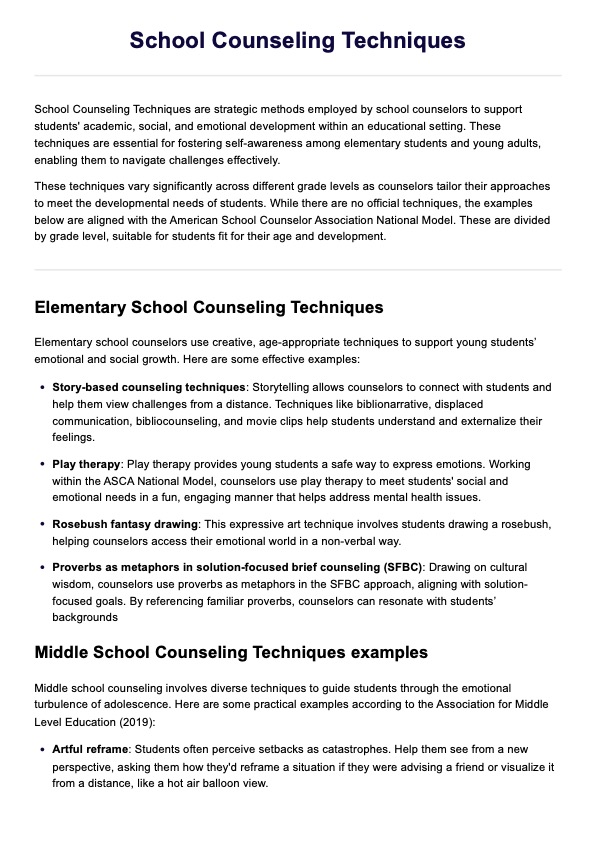
Our SOAP note template has been created with a range of different counselors in mind. Although every counselor likely has their own preferences regarding how they organize and plan sessions with clients, we have tried to create a template that is applicable to everyone, regardless of these small differences.
The types of counselors that can use our SOAP note template include, but are not limited to:
- Mental health counseling
- Family and relationship counseling
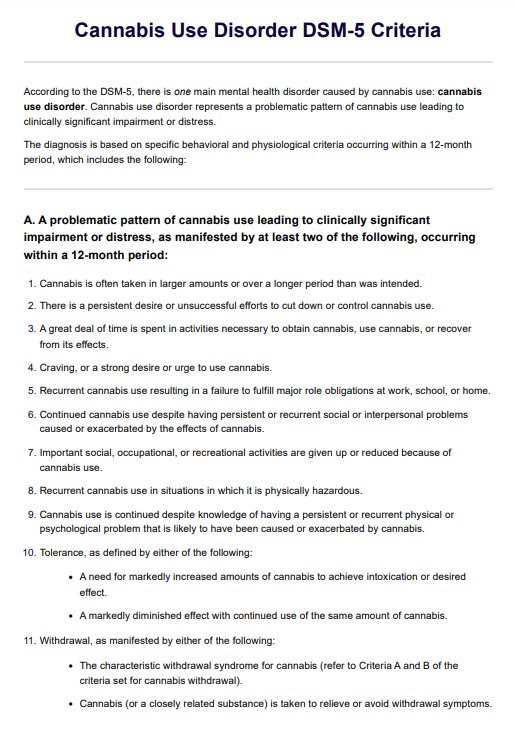
- Substance use counseling
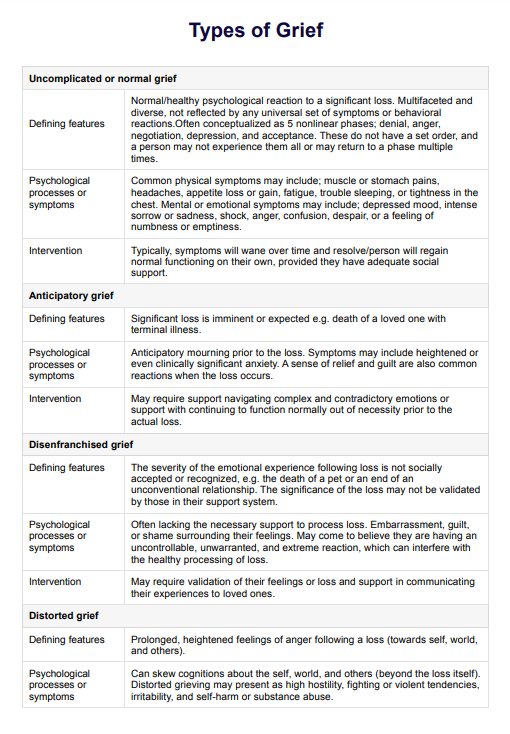
- Grief counseling
- Youth counseling
Although the content of the sessions relating to each of these types of counseling will differ, the SOAP note format remains the same. Additionally, our SOAP note template can be utilized for both individual and group sessions. If you are writing a SOAP note for a group counseling session, then it is generally recommended that you write an individual note for each participating member. This helps to ensure that you have covered enough detail in your documentation and that the progress of each patient can be successfully managed.
Why is This Template Useful For Counselors?
This SOAP note template is useful for counselors for a range of different reasons, including the following:
- Layout: One of the best aspects of the SOAP note template is that the layout has already been organized for you. All you have to do is access the PDF and fill in the relevant sections.
- Informed decisions: Using a SOAP note template helps ensure that all of the information required to make an informed clinical decision is accessible. As long as you stay on top of your note-taking, then these SOAP notes will allow you to track a patient’s progress more effectively, adjusting treatment plans and where necessary and making more informed decisions.
- Care team has access to vital information: The SOAP note template helps to create consistency across all of your clinical documentation. This means that every member of a patient’s care team can access the patient’s SOAP notes, leading to better communication and coordination of care.
Benefits of Using the Counselor SOAP Note Template
In addition to having a range of uses, the counselor SOAP note template also has a wide array of different benefits:
Consistency
SOAP notes have been designed to guarantee consistency across your clinical documentation. With our SOAP note template, you can ensure that your progress notes all use the same structure, making them easily understood by all members of the patient’s care team.
Save time
Counselors lead very busy lives. As such, any tool that helps streamline their workload is greatly appreciated, and this is exactly what the counselor SOAP note template aims to do. By downloading a simple PDF template, you’ll be able to finish your SOAP notes in record time - without compromising the quality of your documentation.
Track patient progress
Of course, one of the most important purposes of SOAP notes is to track your patients’ progress. This template allows you to do this effectively, ensuring that all of the relevant information regarding a patient’s treatment has been recorded. You can review your past notes and amend treatment plans, diagnoses, and medications where necessary.
Improve clinical outcomes
Every counselor should constantly be looking to improve clinical outcomes. Using a SOAP note template can help organize your notes more effectively, improving communication and consequently leading to more informed clinical decisions. All of these factors can facilitate a better treatment program for your patients, leading to improved outcomes.
Legal and insurance situations
It’s important to remember that SOAP notes are legal documents. In order to protect yourself and your patients, and simplify insurance and billing processes, having effective and consistent SOAP notes is vital. We’ve created our PDF template with this in mind, helping to ensure you cover all relevant information in an accessible way.
Commonly asked questions
This can be quite a difficult question to answer, given it is largely dependent on the type of session you had with your patient. However, it’s important to remember two things: SOAP notes need to cover all important areas of information, and they also need to be concise. Approximately, your SOAP notes should be somewhere between 1-2 pages.
The best time to write your SOAP notes is immediately after each session with a patient. This ensures that information is still fresh in your mind and you don’t miss out on any important details. Staying on top of your documentation will also help you stay productive and ensure you don’t have stacks of notes to write at the end of each week.
After you have written your SOAP notes, you need to store them in a HIPAA-compliant manner. In order to keep them protected at all times, we recommend using EHR or practice management software like Carepatron.






-template.jpg)