SOAP Notes For Speech Therapy Template
Functional SOAP note template for speech therapy, helping you to streamline your documentation and create compelling and accurate SOAP notes.


What is a speech therapy SOAP notes?
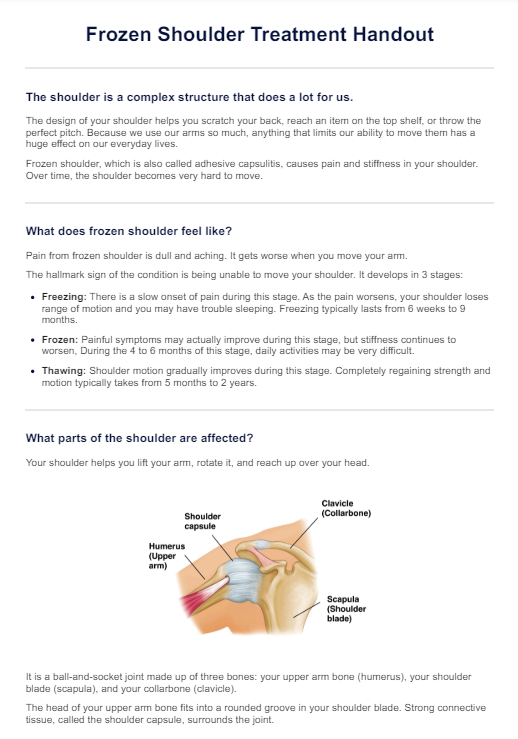
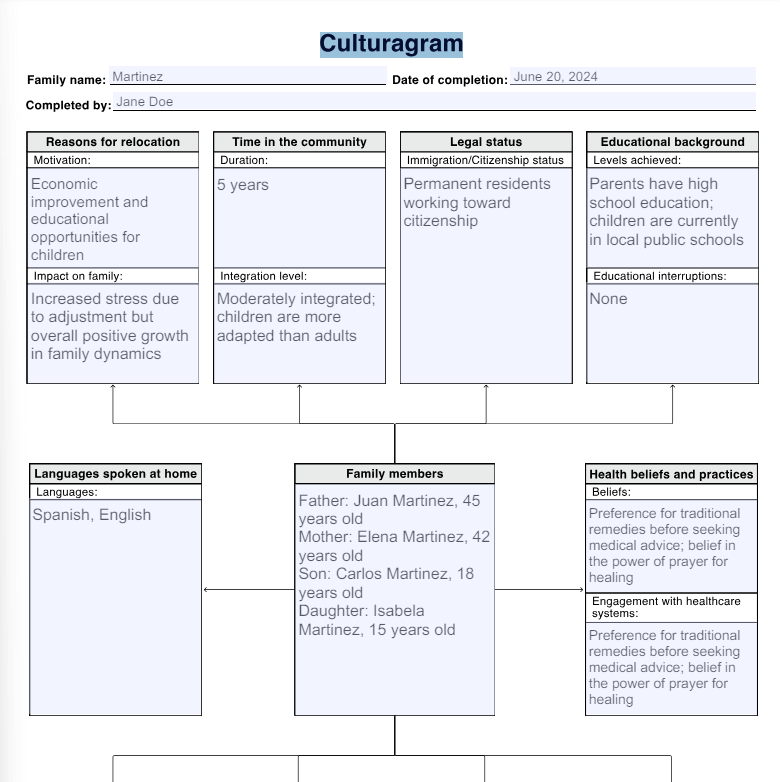
Within the confines of a private practice's therapy room, speech pathologists engage in the art of documenting client progress during speech therapy. After each session, they conscientiously write notes, translating subjective observations into objective data—a crucial aspect for future sessions.
Witnessing patient progress firsthand, therapists find fulfillment in their skilled interventions. The records serve as guideposts, shaping the roadmap for individual sessions and marking tangible strides. This meticulous process measures progress and weaves a growth narrative for the treatment session. It creates a vital bridge connecting the previous session to the promising horizons of the next session.
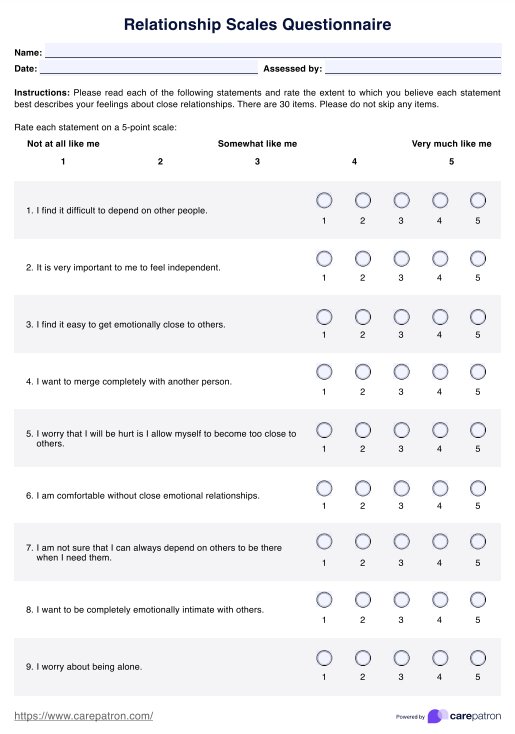
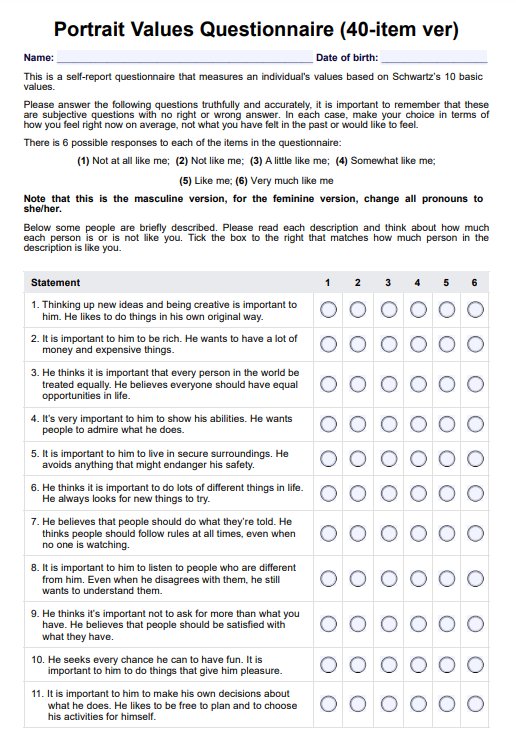
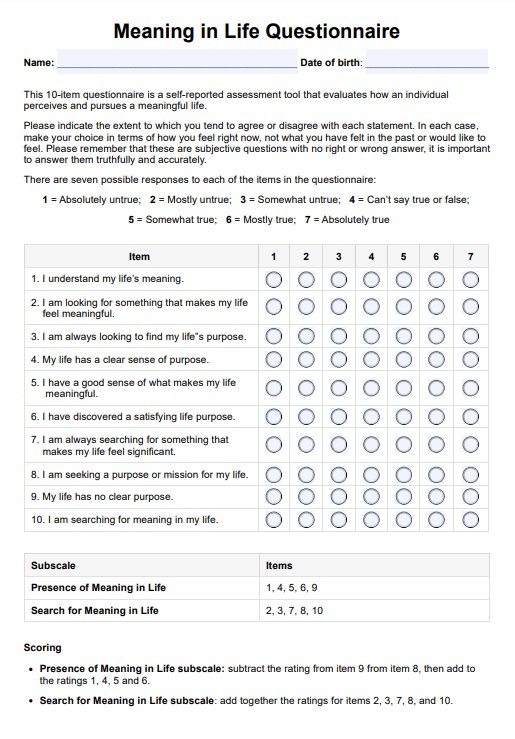
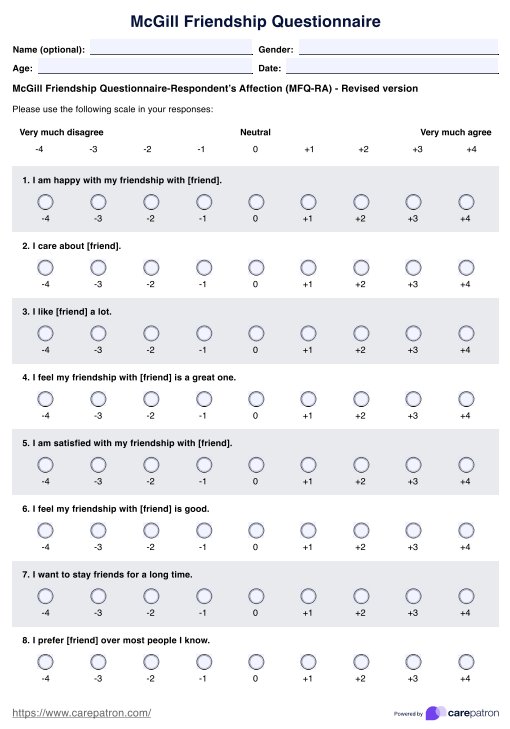
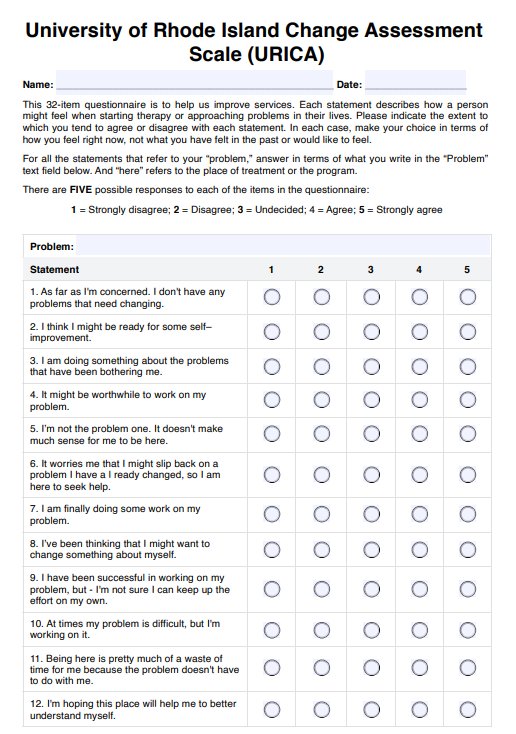
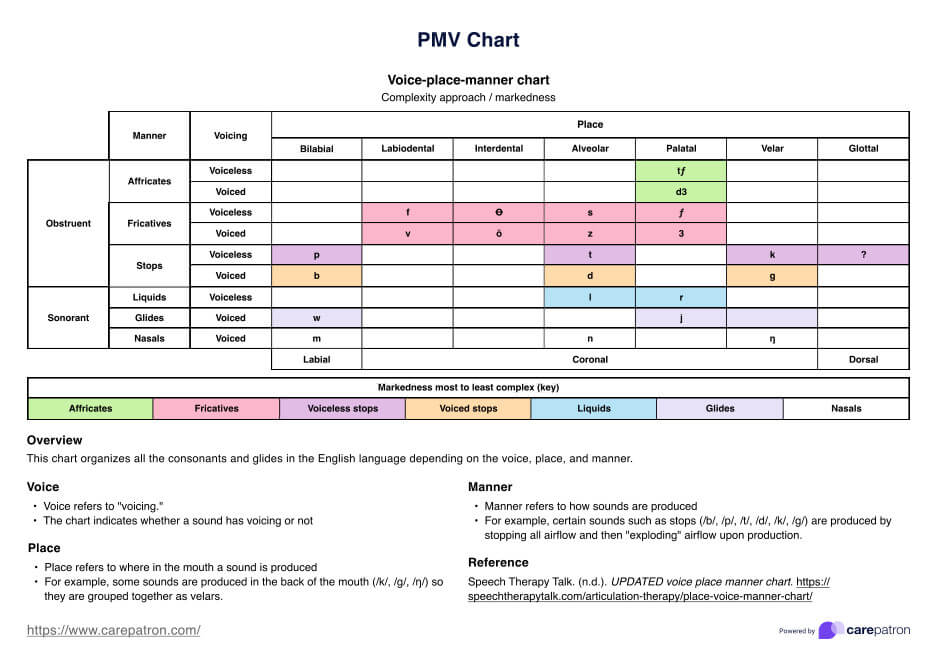
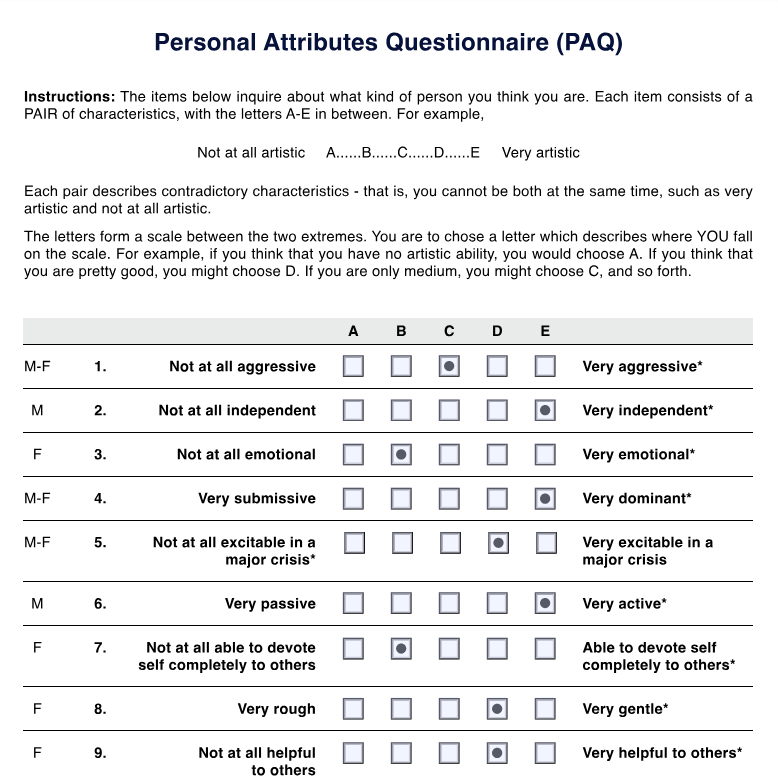
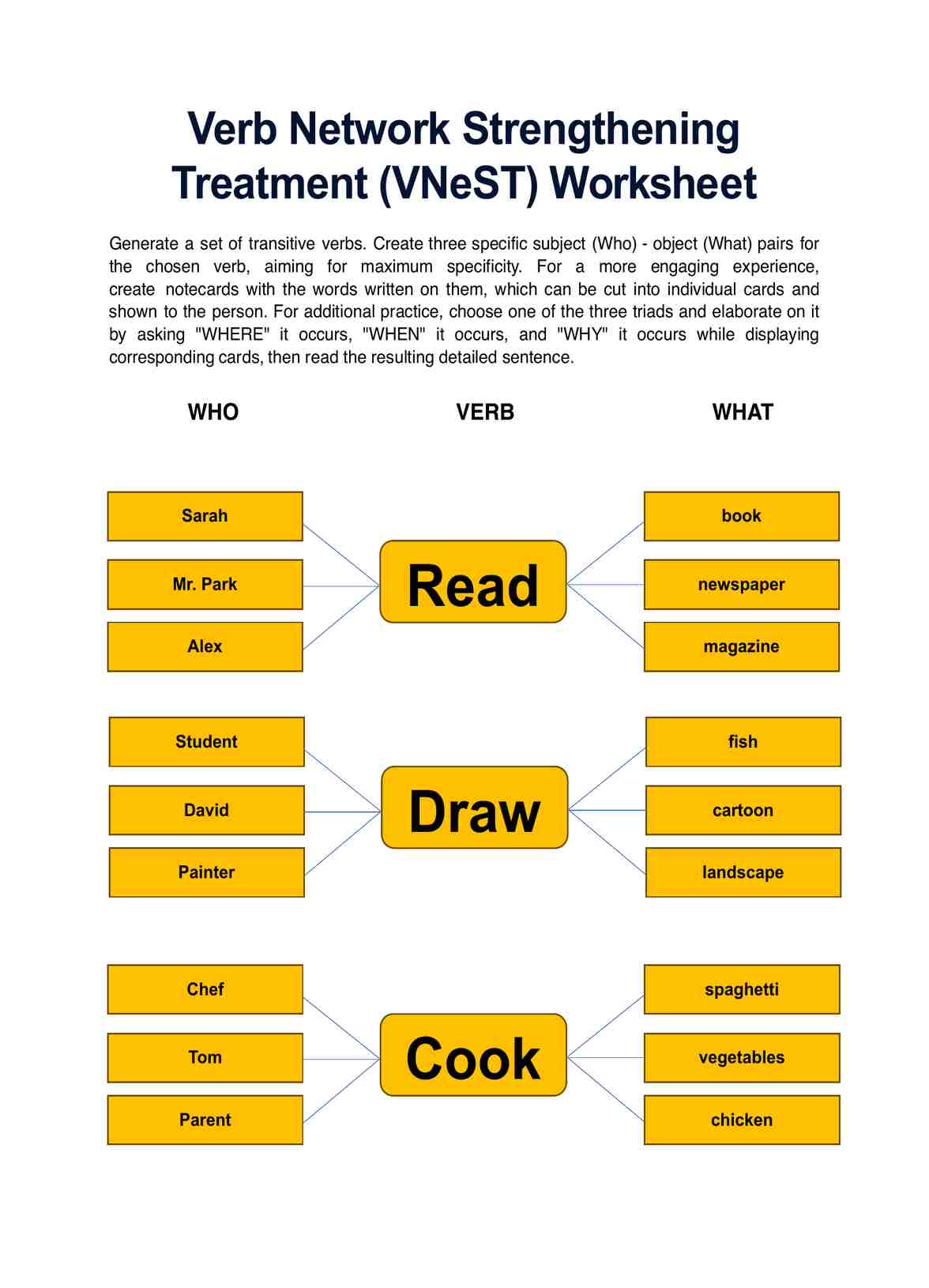
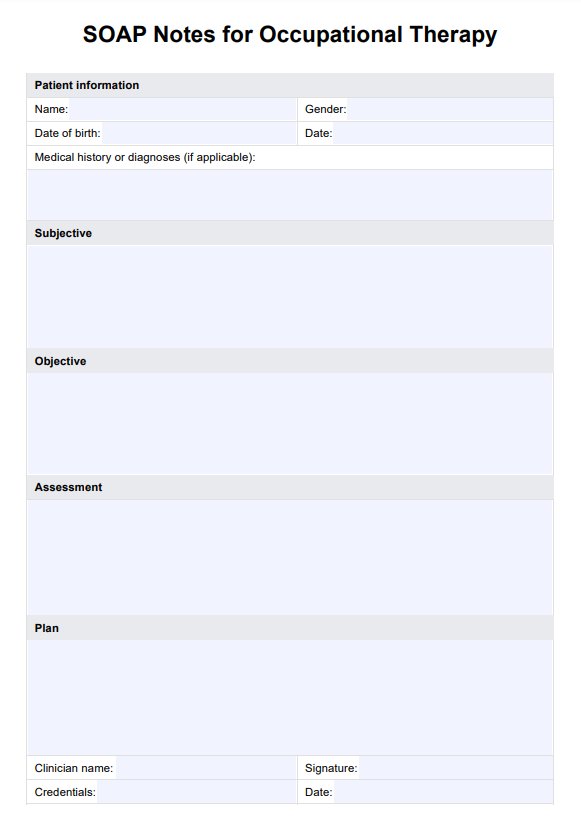
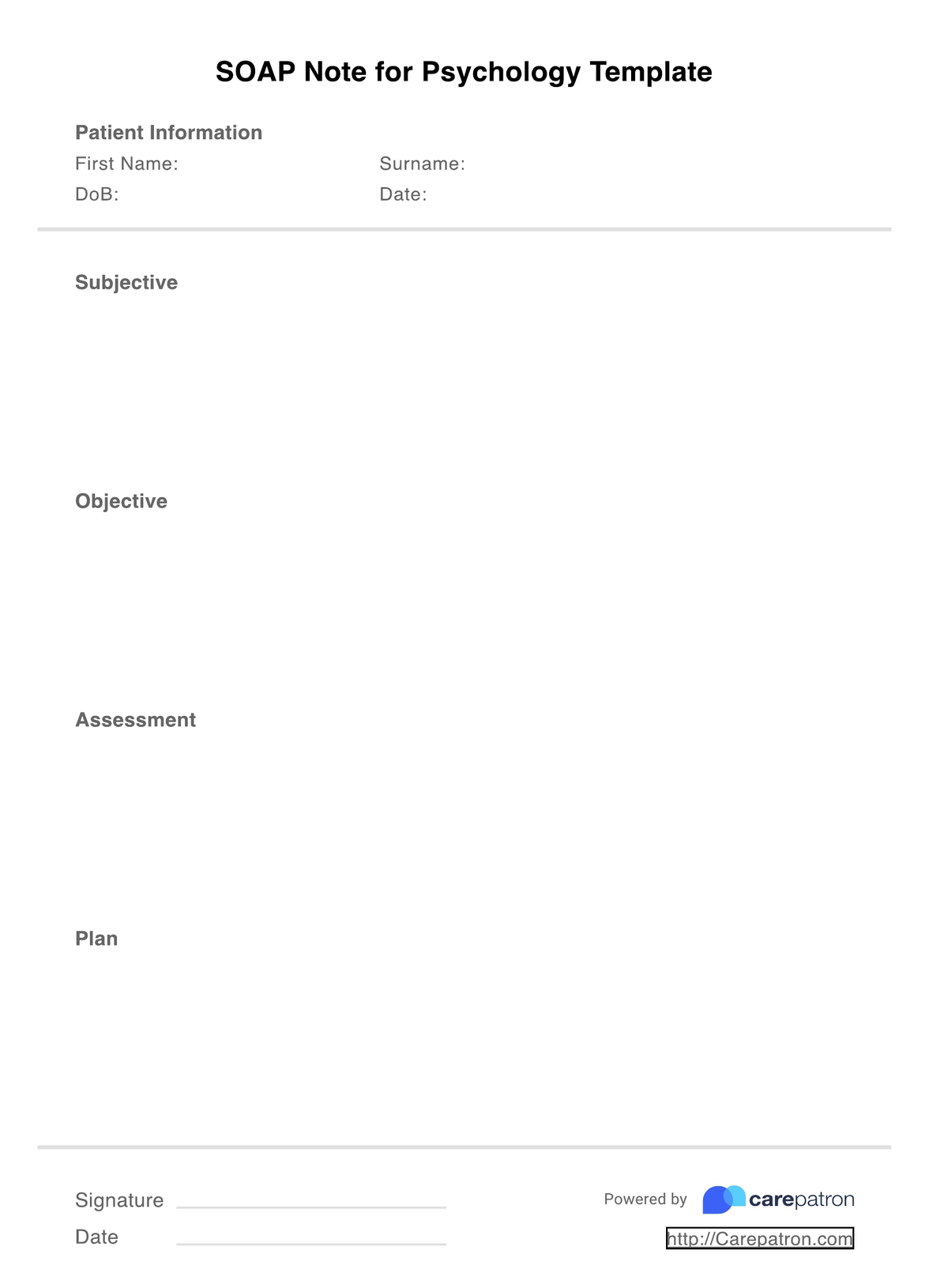
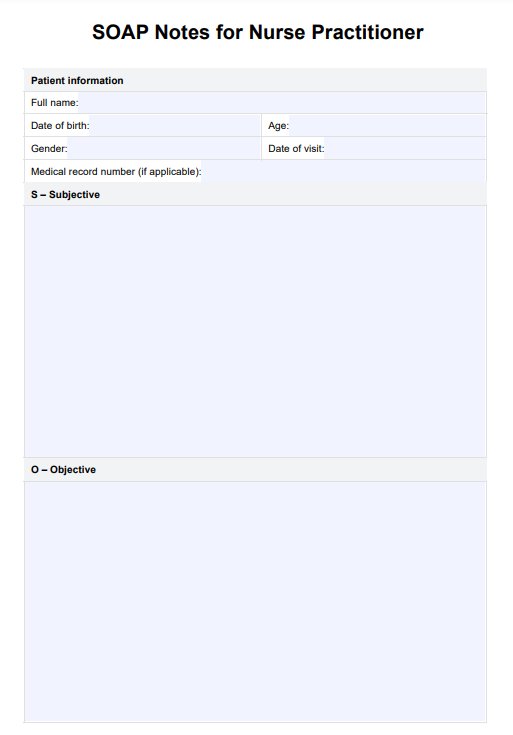
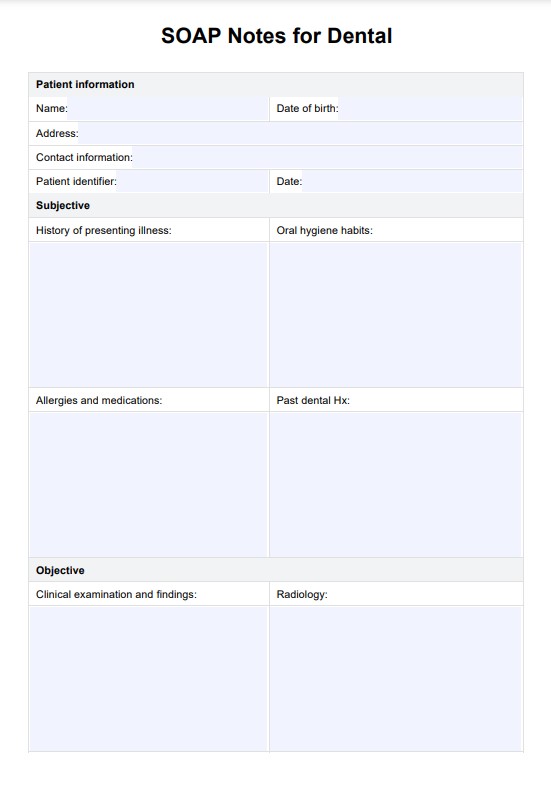
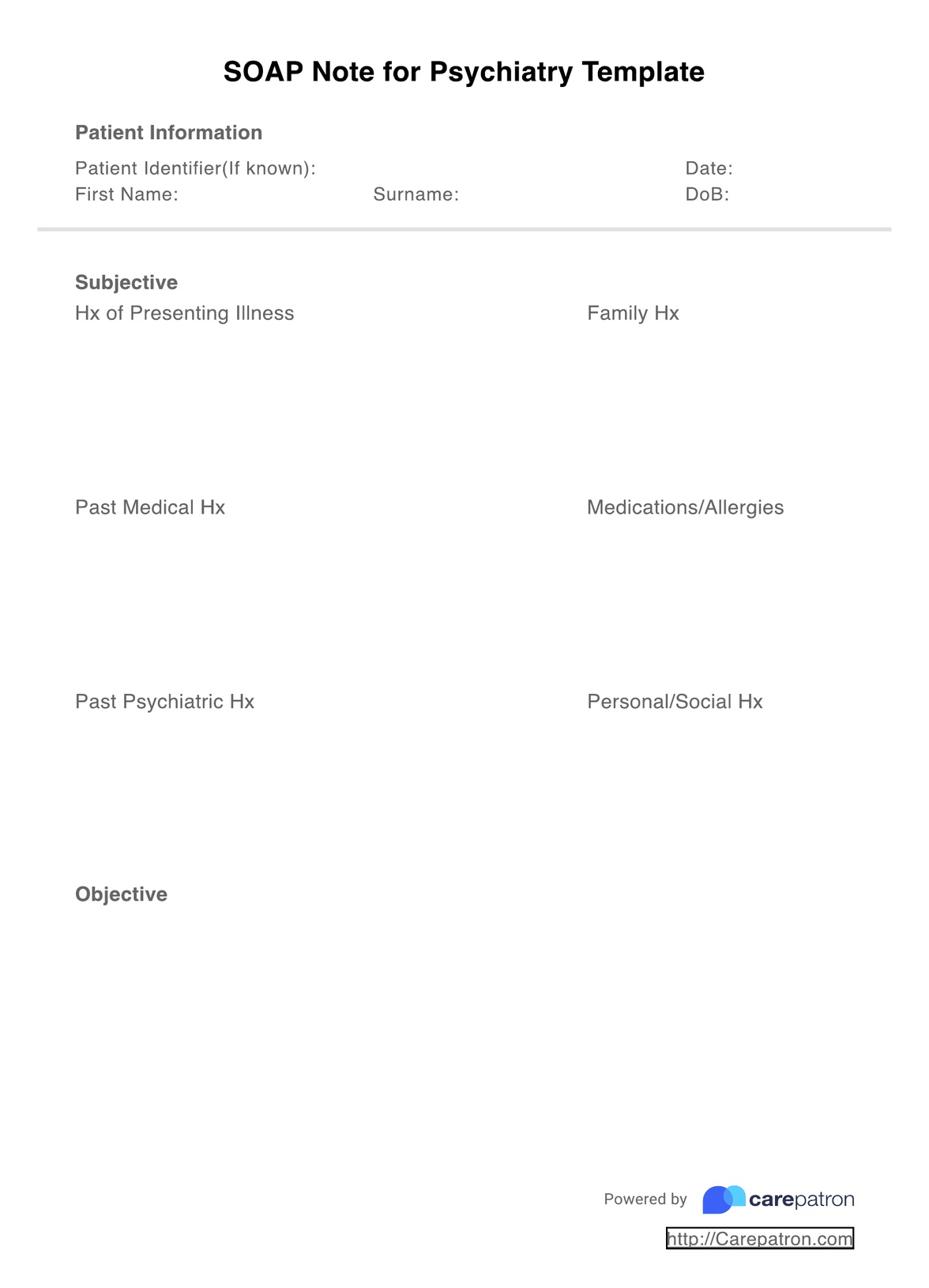
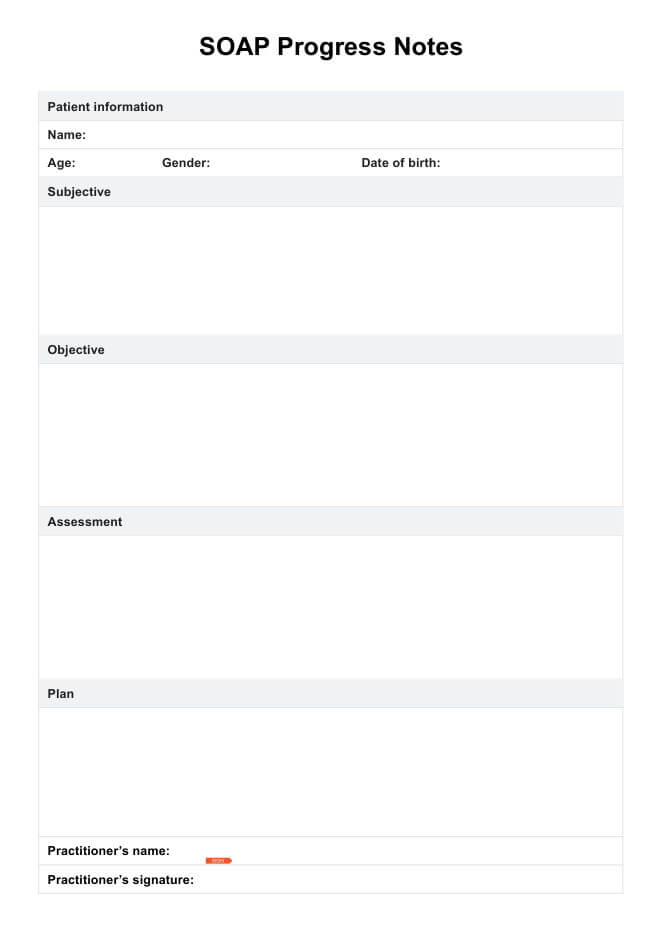
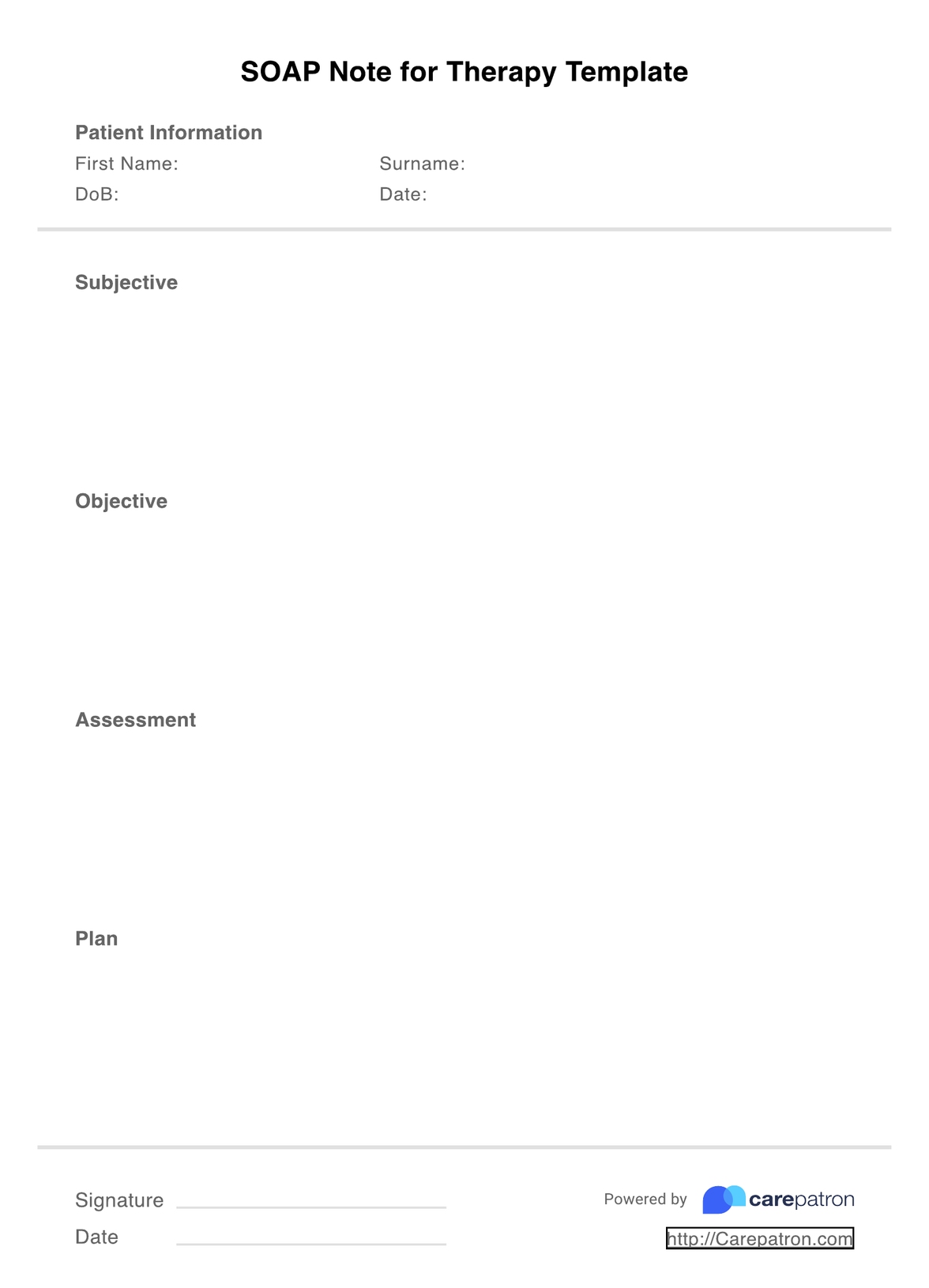
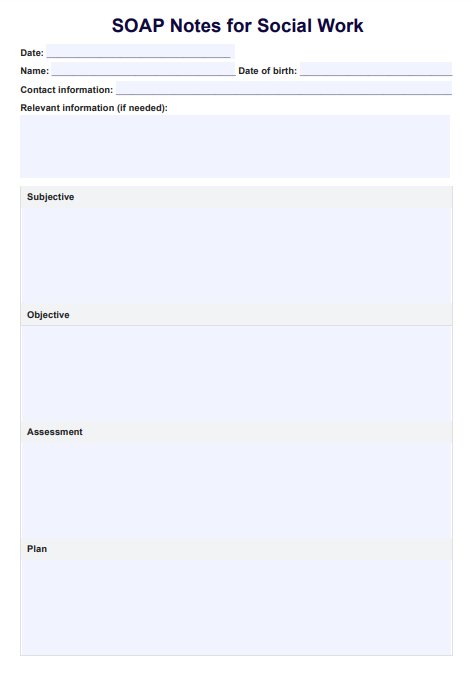
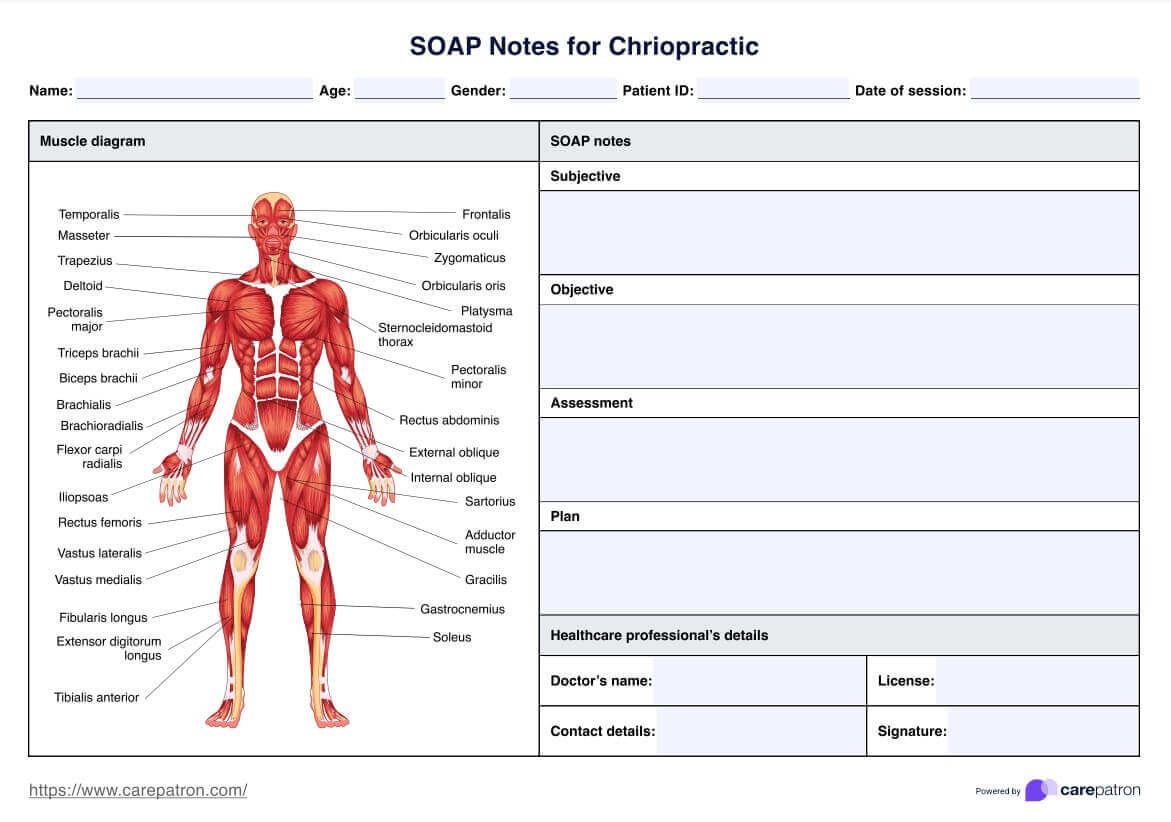
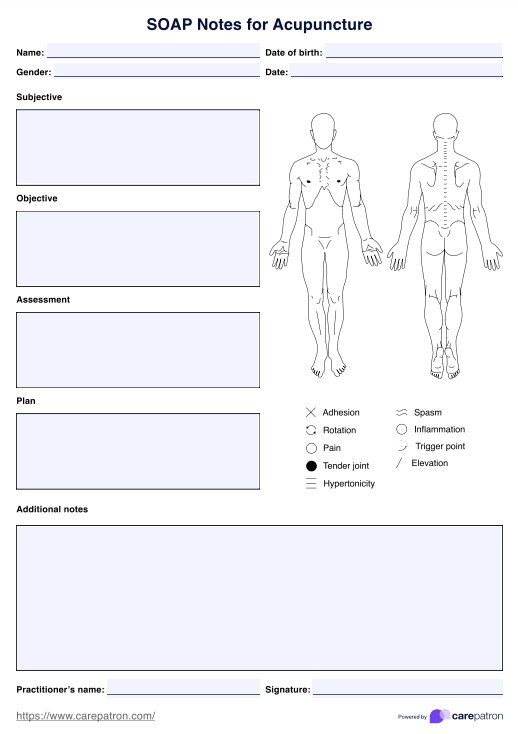
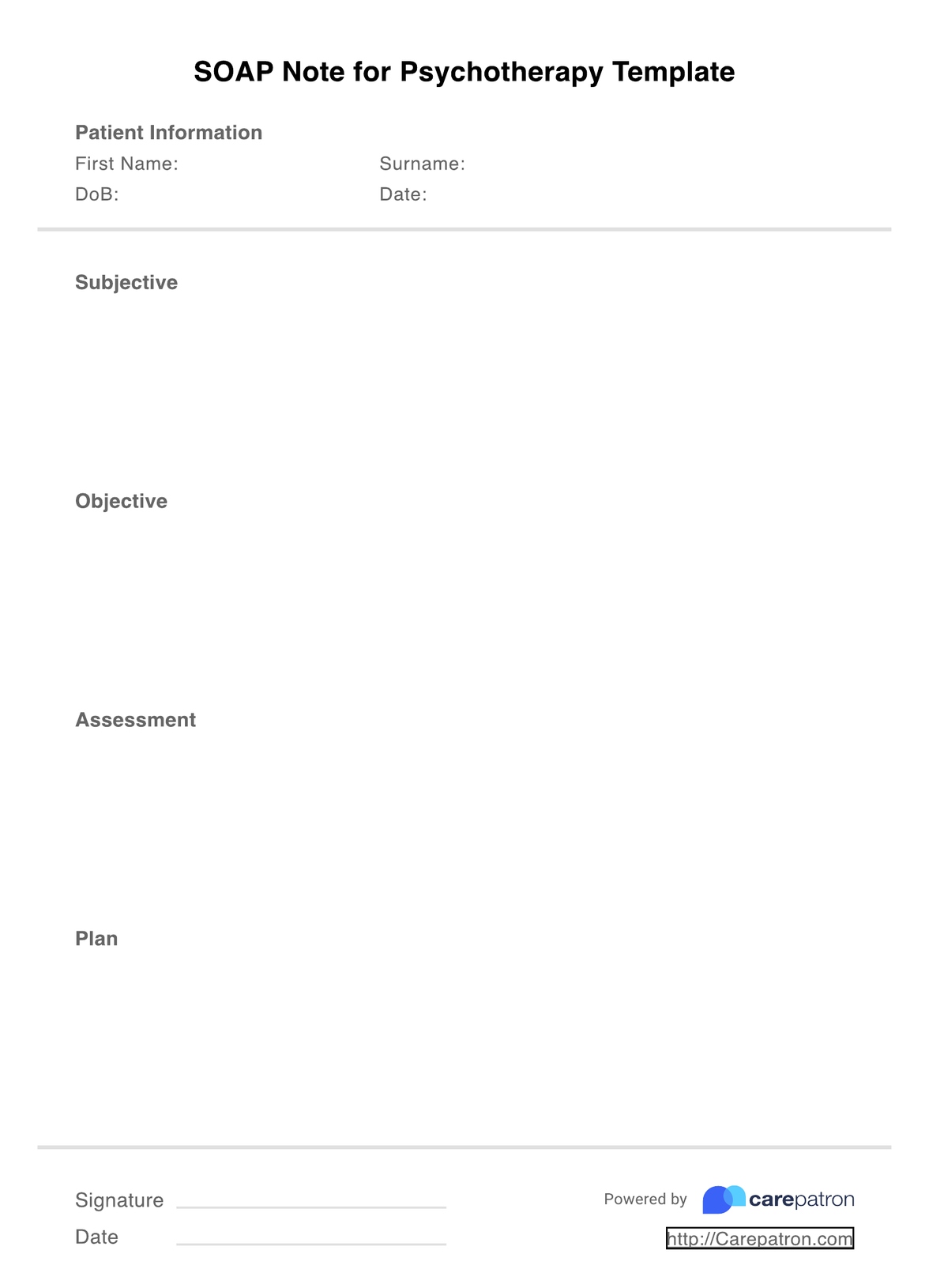
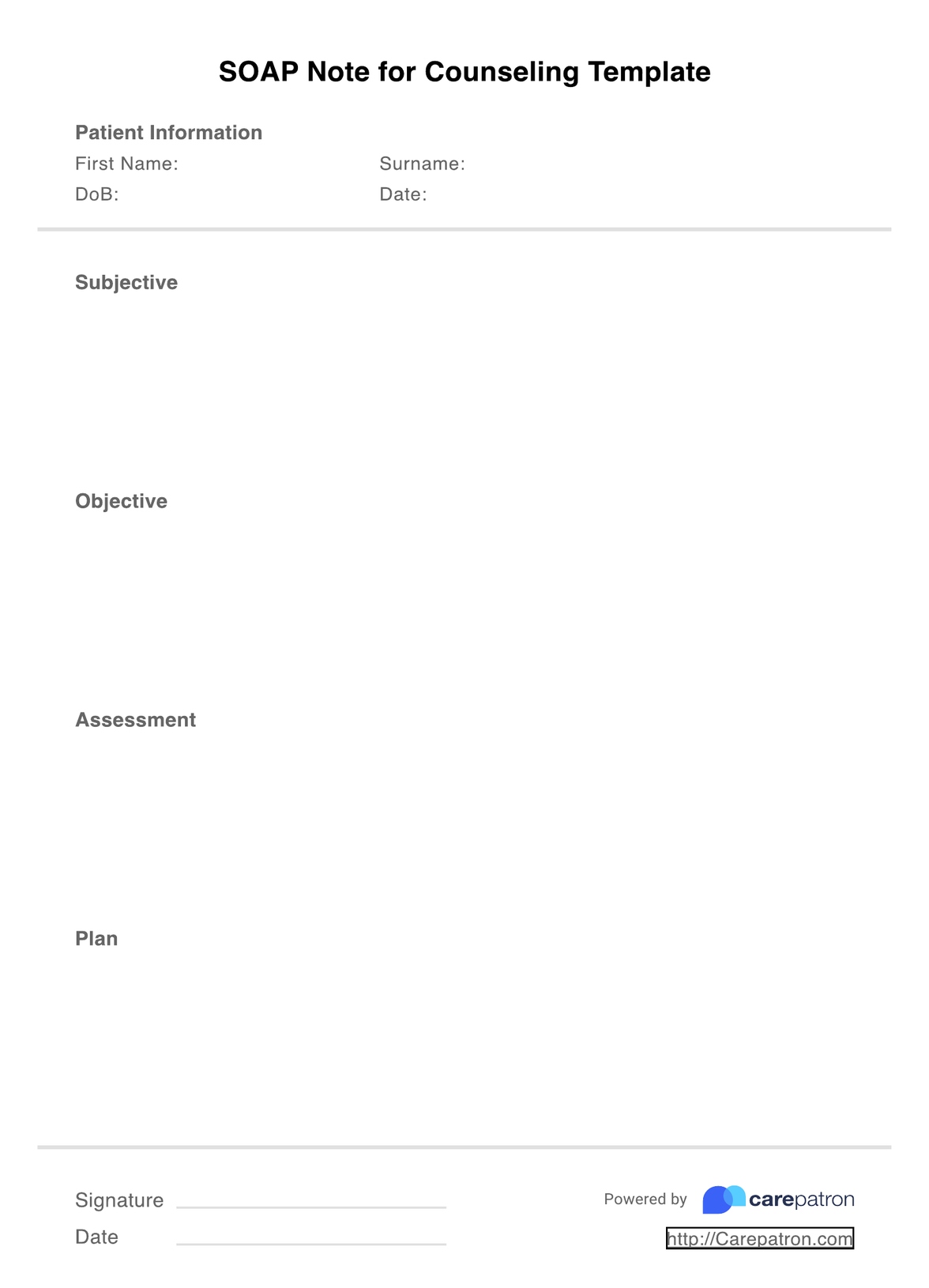
Speech therapy SOAP notes are a form of clinical documentation that speech therapists use in documenting speech therapy sessions and progress of their clients. As one of the most popular ways to organize progress notes, the SOAP format separates information into four sections: subjective, objective, assessment, and plan. These four sections cover different types of information:
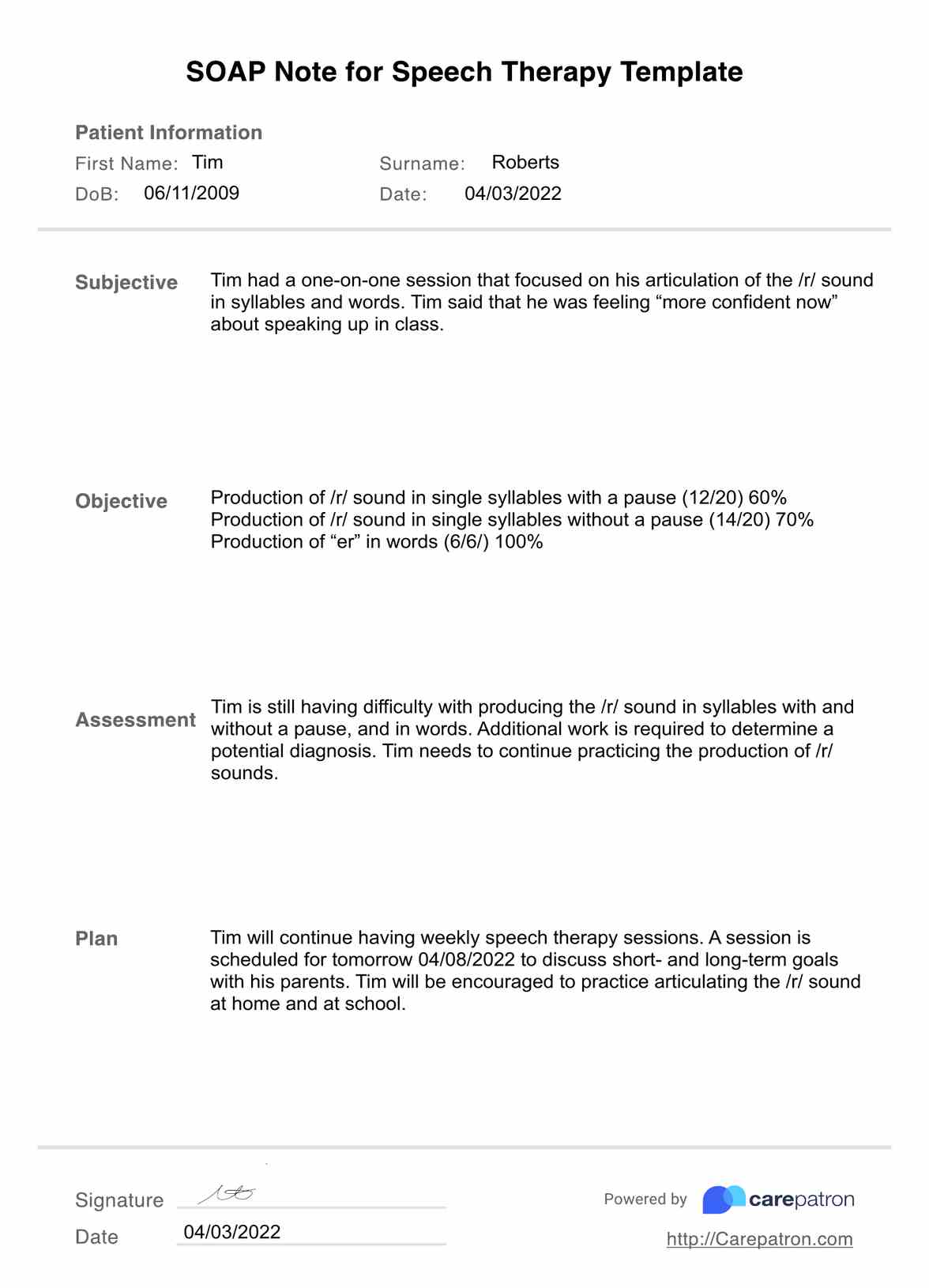
- Subjective: The client's subjective description of their concern, including symptoms and how it affects their day-to-day life. This section often includes direct quotes from the client.
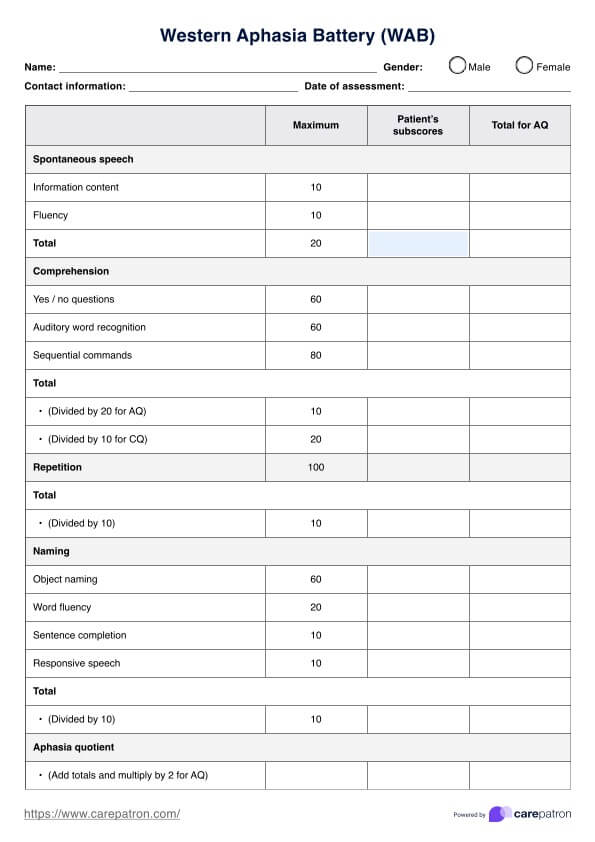
- Objective: Your professional observations about the client's behavior, the interventions you used during the session, and how the client responded. The objective section should also include any tests or assessments that the client completed.
- Assessment: A synthesis of the above sections; your assessment and analysis of the session. This section includes treatment goals and determines progress made by client.
- Plan: The final section outlines the future plan for the client, including any upcoming sessions, goals to be completed, or relevant changes to the treatment plan.
The speech therapy SOAP note template is both intuitive and coherent; it aims to simplify the note-taking process so you can save time without compromising the quality of your documentation.
You can explore the therapy SOAP notes template, which organizes clinical documentation effectively into sections like subjective, objective, assessment, and plan. This structured approach streamlines note-taking, saving time and ensuring quality documentation in therapy settings.
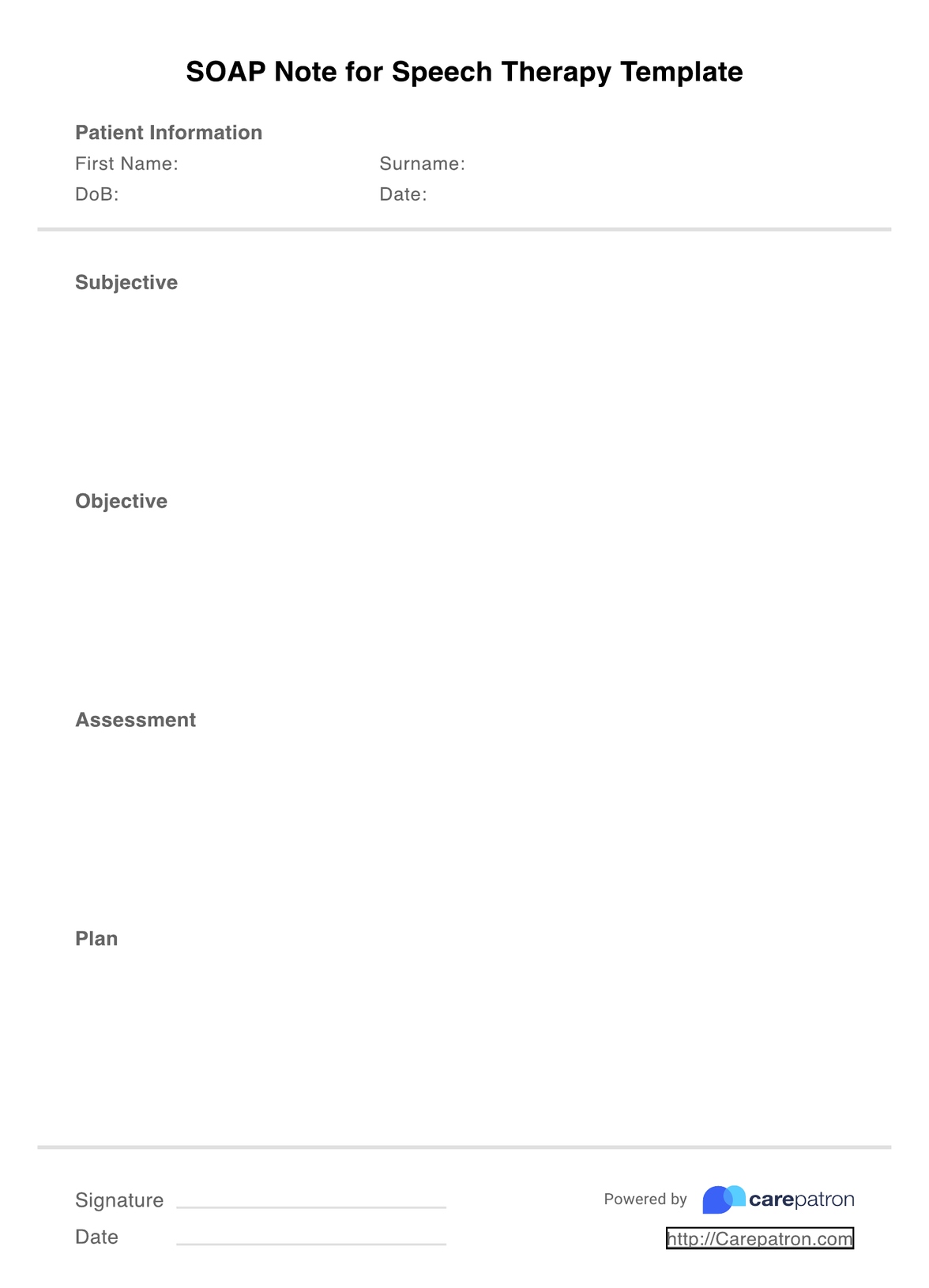
SOAP Notes For Speech Therapy Template
SOAP Notes For Speech Therapy Template Example
How to use this SOAP note template for speech language therapy
Using the speech therapy SOAP note template is very easy. Regardless of whether you are an individual practitioner or work at a speech therapy practice, we have designed this resource with the understanding that most speech therapists lead busy lives and as such, they are on the lookout for simple ways to speed up their documentation. With that in mind, here are four simple steps that can guide your usage of the template:
Step 1: Download the template
The first thing you need to do is click on the link that will take you to the PDF version of the template. From here, you will be able to edit the document where necessary.
Step 2: Fill out the four sections
After you have downloaded the SOAP note template, it's time to fill out the four sections (subjective, objective, assessment, and time). When you are writing your documentation, you want to be as clear and concise as possible, while also including every piece of relevant information based on the patient's response.
Step 3: Don't forget credentials
Every speech therapy SOAP note needs to include certain credentials: your client's name (and ID number where applicable), the date/time of the session, and your own professional credentials. These details are useful when it comes to insurance and billing processes.
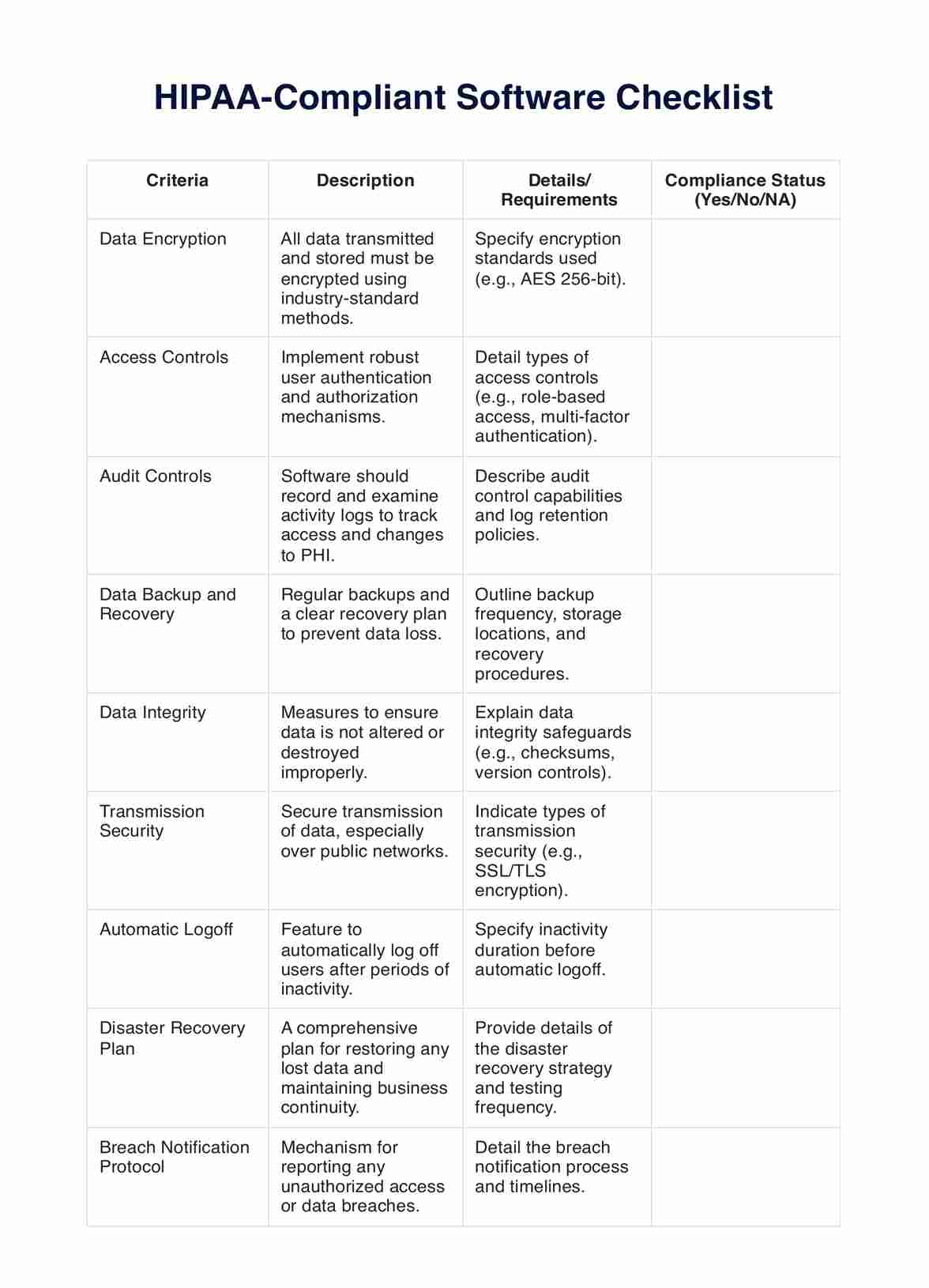
Step 4: Store your SOAP note securely
In order to adhere to HIPAA compliance regulations, you need to store your SOAP notes securely. If you store it online, you need to ensure the platform has suitable electronic safeguards so your client's data is protected at all times.
Who can use this speech therapy template?
One of the best things about the SOAP note template we have used is how customizable it is to different fields of speech therapy. Essentially, this SOAP note template applies to any kind of speech therapist who has sessions with clients, including those who work as solo practitioners and those who work in group practices.
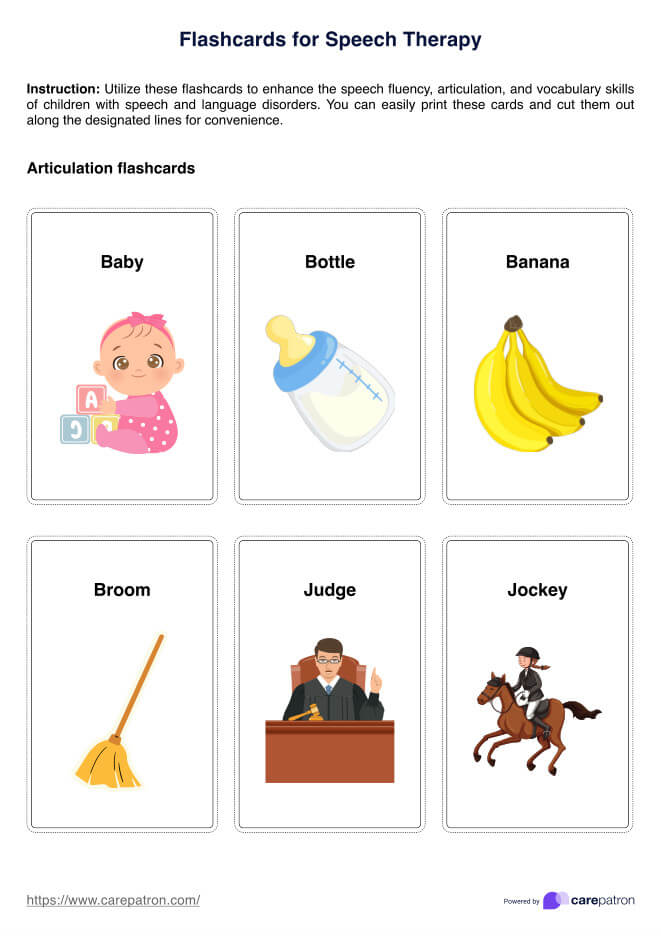
Additionally, speech therapists often work with a range of clients who may all have different problems, disorders, or assessments, including the following:
- Speech therapy for apraxia
- Speech therapy for aphasia
- Speech therapy for stuttering
- Speech therapy for swallowing difficulty
Further, each of these types of speech therapy is applicable to clients of all ages. The specific methods that speech therapists use to treat these disorders may differ depending on their client's age, but the format for writing SOAP notes will remain the same.
As you can see, the speech therapy SOAP note template is able to be used by pretty much every speech therapist, regardless of where they work or what type of therapy they specialize in!
Why is this template useful for speech therapists?
The most important use of a SOAP note template for speech therapists is how effectively it organizes clinical documentation. Writing accurate notes can be a time-consuming process, but with this template, you can streamline this process without reducing the overall quality of the note. Other uses include:
- Consistency: Writing consistent SOAP notes helps with readability. When you check your previous notes, you can extract relevant information faster if they are consistent, which is much easier if you use a SOAP note template.
- Accuracy: The SOAP note template visually separates the four different sections. Using this template will ensure that you don't accidentally forget to fill out all four sections, helping to improve the overall accuracy of your documentation.
- Suitability: As we mentioned, the SOAP note template has been designed to suit various types of speech therapy. This allows you to access an intuitive SOAP note template and use it for all of your clients, regardless of the differences in their specific speech problems.
.png)
Benefits of using the SOAP Notes For Speech Therapy Template
In addition to having various uses, using the speech therapy SOAP note template has many benefits for your private practice. Some of these advantages include:
Track your client's progress effectively
The biggest reason for writing SOAP notes is, of course, to track your patient's progress. Using a template will assist in making this information consistent, so you can easily compare notes and determine how effectively your treatment plan works.
Communication
Effective communication between care providers is an often overlooked aspect of delivering healthcare. With a SOAP note template, you can ensure that all members of a client's care team have access to the relevant information, helping them to make more informed clinical decisions.
Workflow and productivity
SOAP note templates help to improve the workflow and productivity at speech therapy practices. By streamlining the documentation process, you will be able to save countless hours that can instead be spent completing more important tasks.
Insurance
SOAP notes can also be shared with insurance companies. If a client's insurance provider is paying for their services, then the provider may reach out looking for certain details. By using a SOAP note template, you can ensure you have an organized system that allows third-parties to access information quickly.
Legal situations
It's important to remember that progress notes are legal documents - this is one of the reasons why you should always prioritize writing accurate and detailed documents. If a legal situation were to arise, having SOAP notes that utilize a template will ensure they are organized and accurate, with a clear description of why certain clinical decisions were made.
Commonly asked questions
This question doesn’t have a definitive answer, but as a good rule of thumb you should aim for 1-2 pages. You want your SOAP notes to be concise and clear, but without any repetitions.
Yes. SOAP notes are legal documents and every client has the right to access their progress notes. For this reason, it is absolutely essential that the information you include is objective, relevant, and truthful.
Yes, HIPAA has certain regulations that are applicable to SOAP notes. Firstly, HIPAA requires you to keep progress notes for each session with a client. The guidelines also require you to store these notes in a safe and secure way, so confidential information pertaining to your client is protected.





-template.jpg)