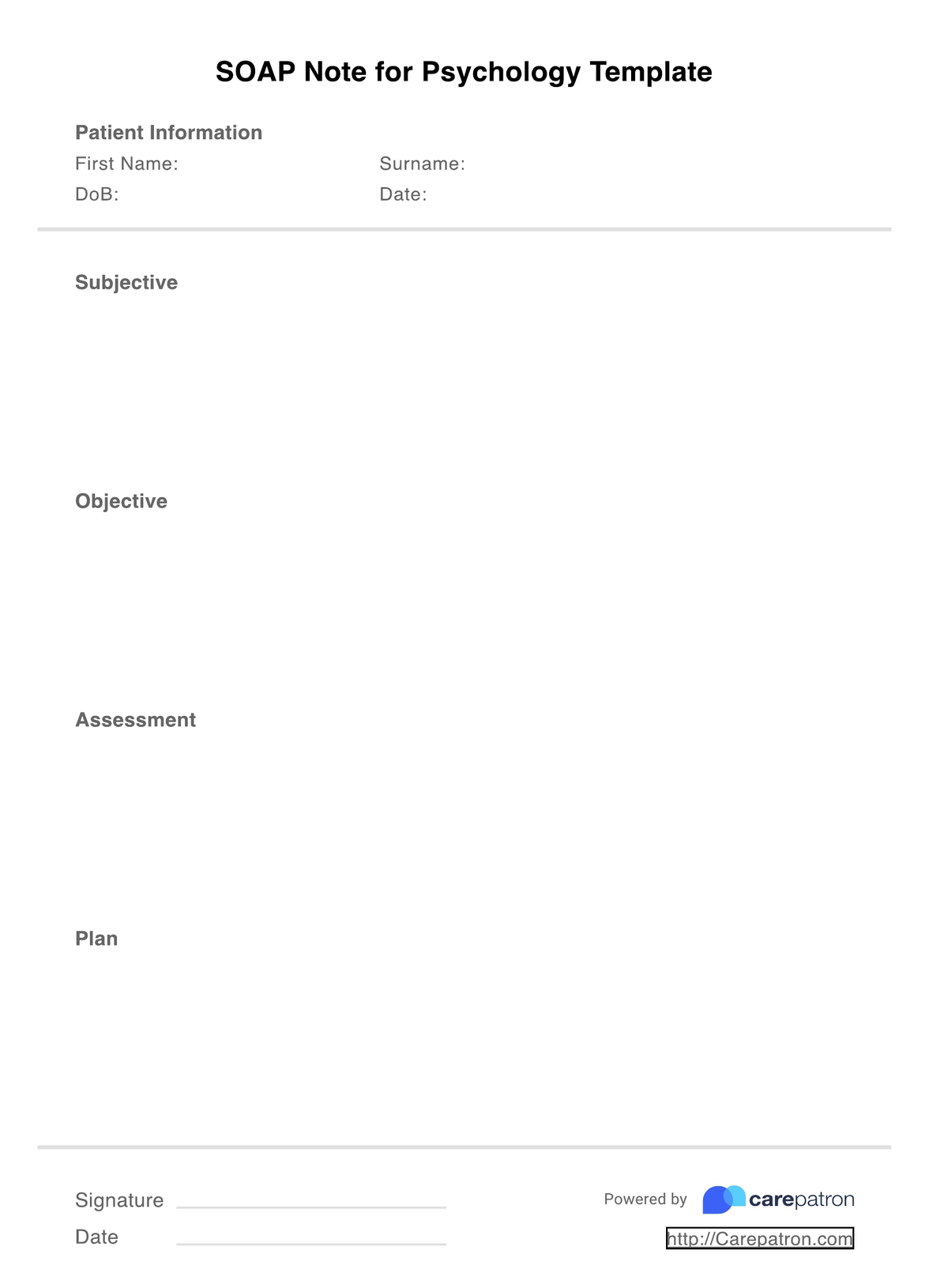
SOAP Notes for Psychotherapy Template
Strengthen clinical outcomes, and boost the quality of your care with high-quality SOAP notes for psychotherapy templates.


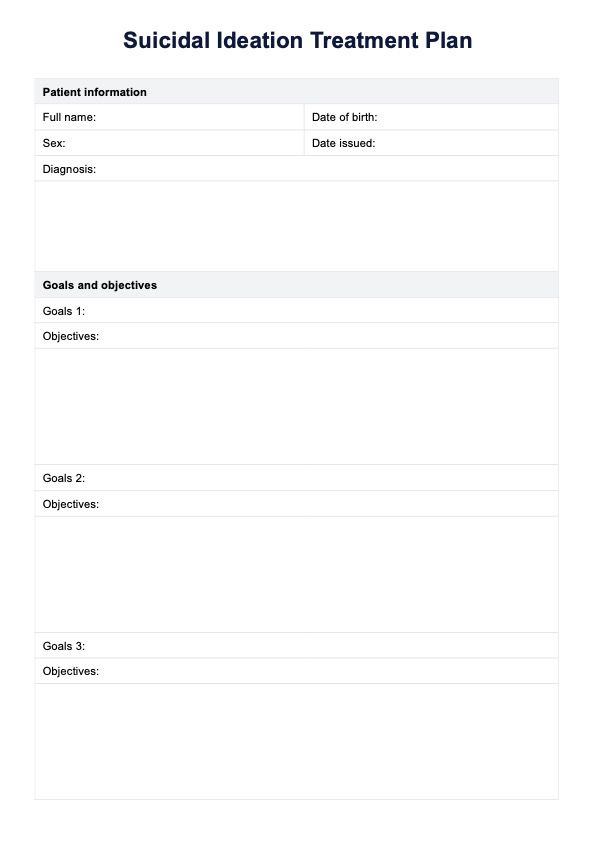
What is a Psychotherapy SOAP Notes Template?
Psychotherapy SOAP note templates are an easy way to boost the credibility of your clinic while ensuring that you provide the highest level of care. You can take effective notes without compromising quality, and ensure that you are representing your client's mental health state to the most accurate degree.
Universally accepted by healthcare professionals worldwide, psychotherapy SOAP notes cover all essential bases when it comes to assessing patient conditions through a holistic lens. No matter your background, specialty, or experience with SOAP, our examples make it super easy to adopt within your business and can be easily understood by fellow professionals.
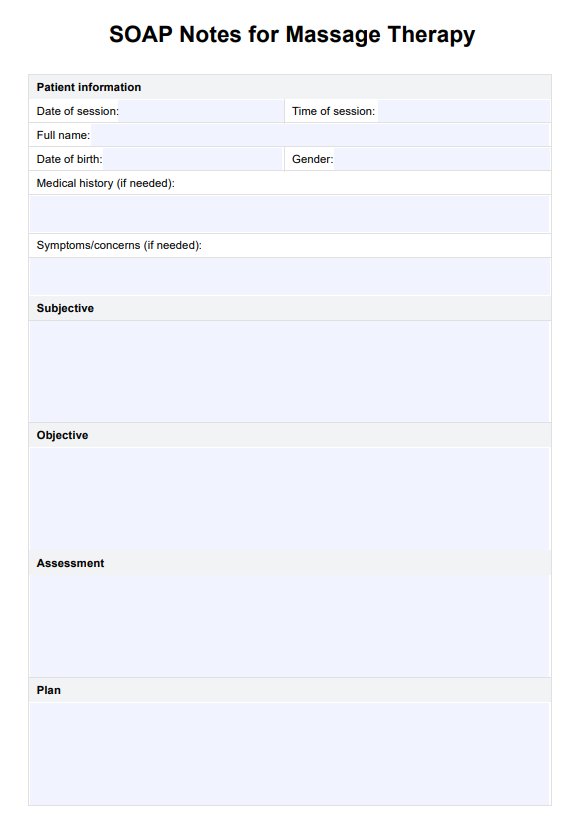
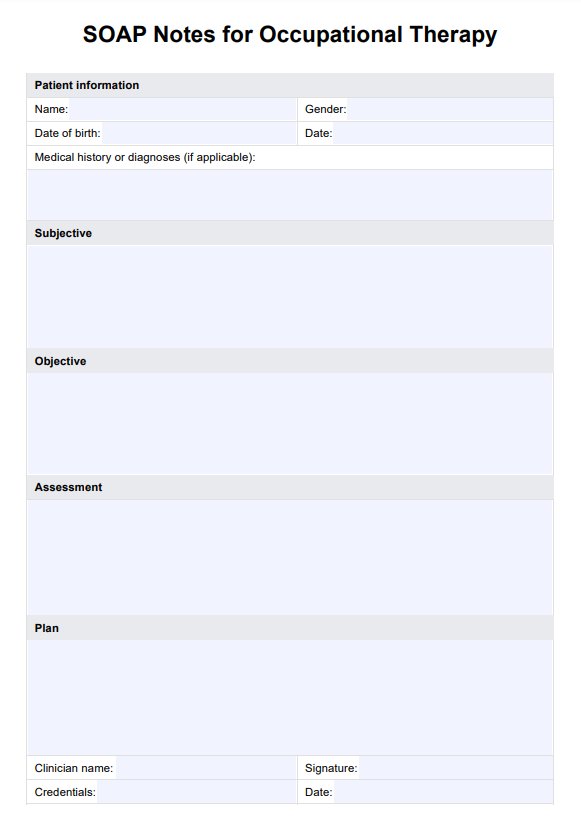
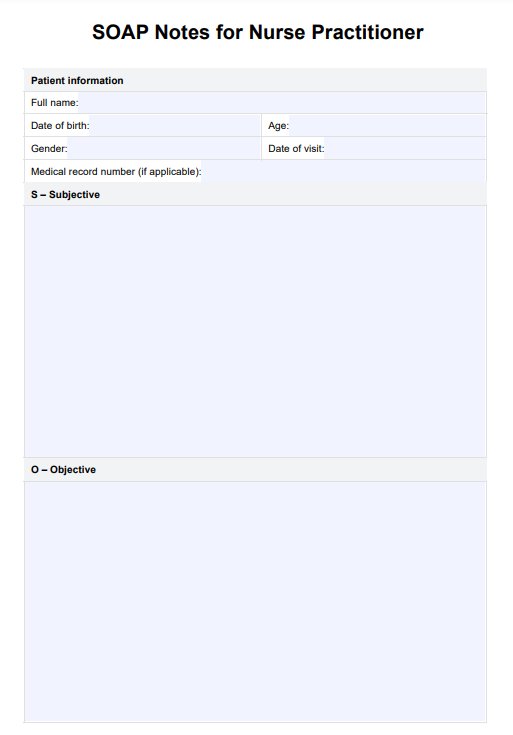
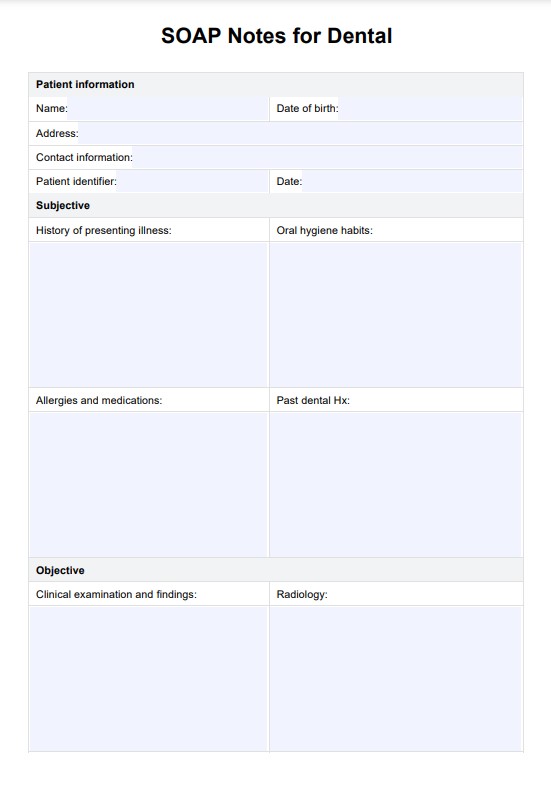
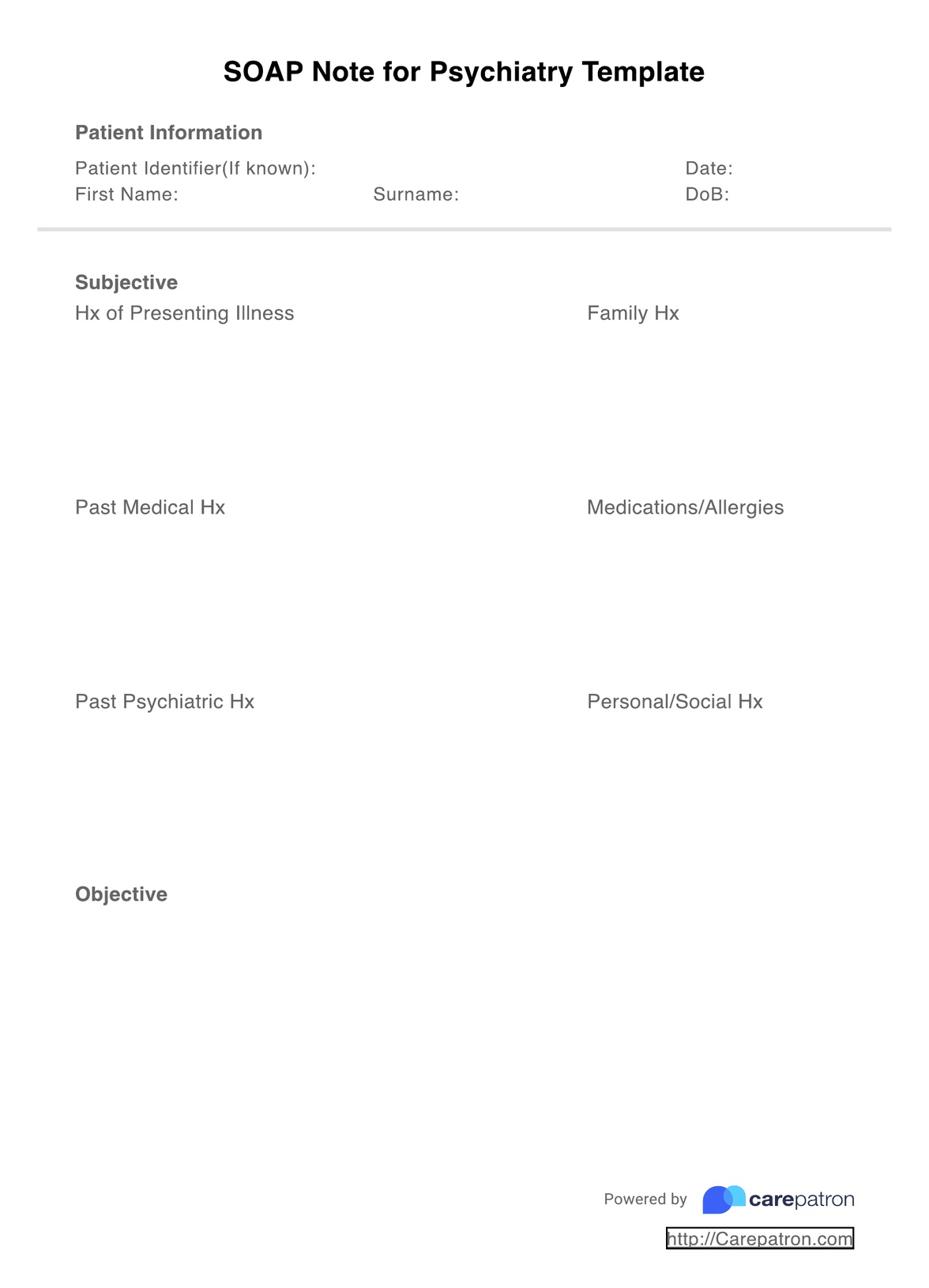
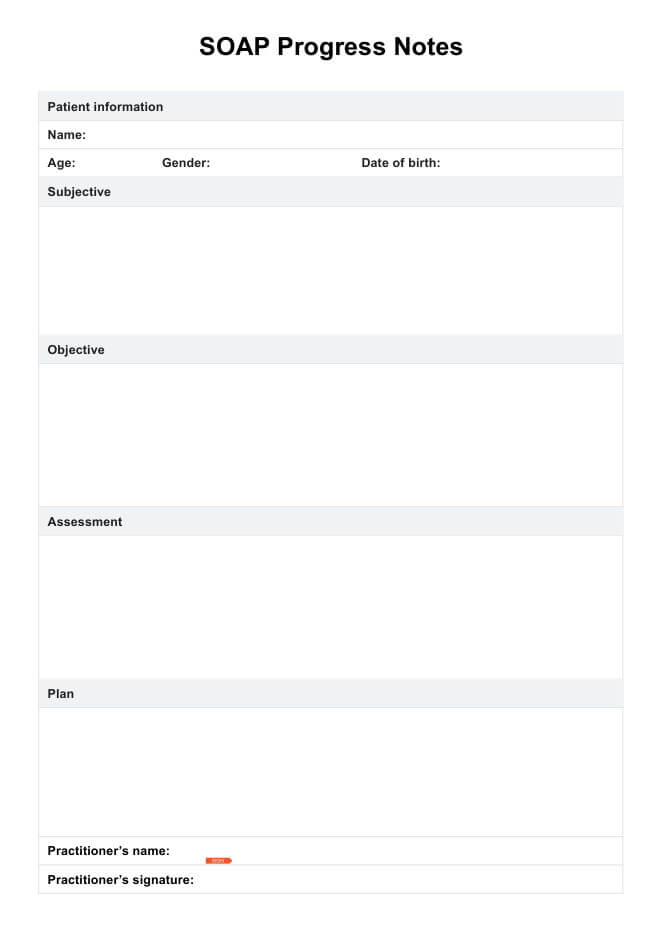
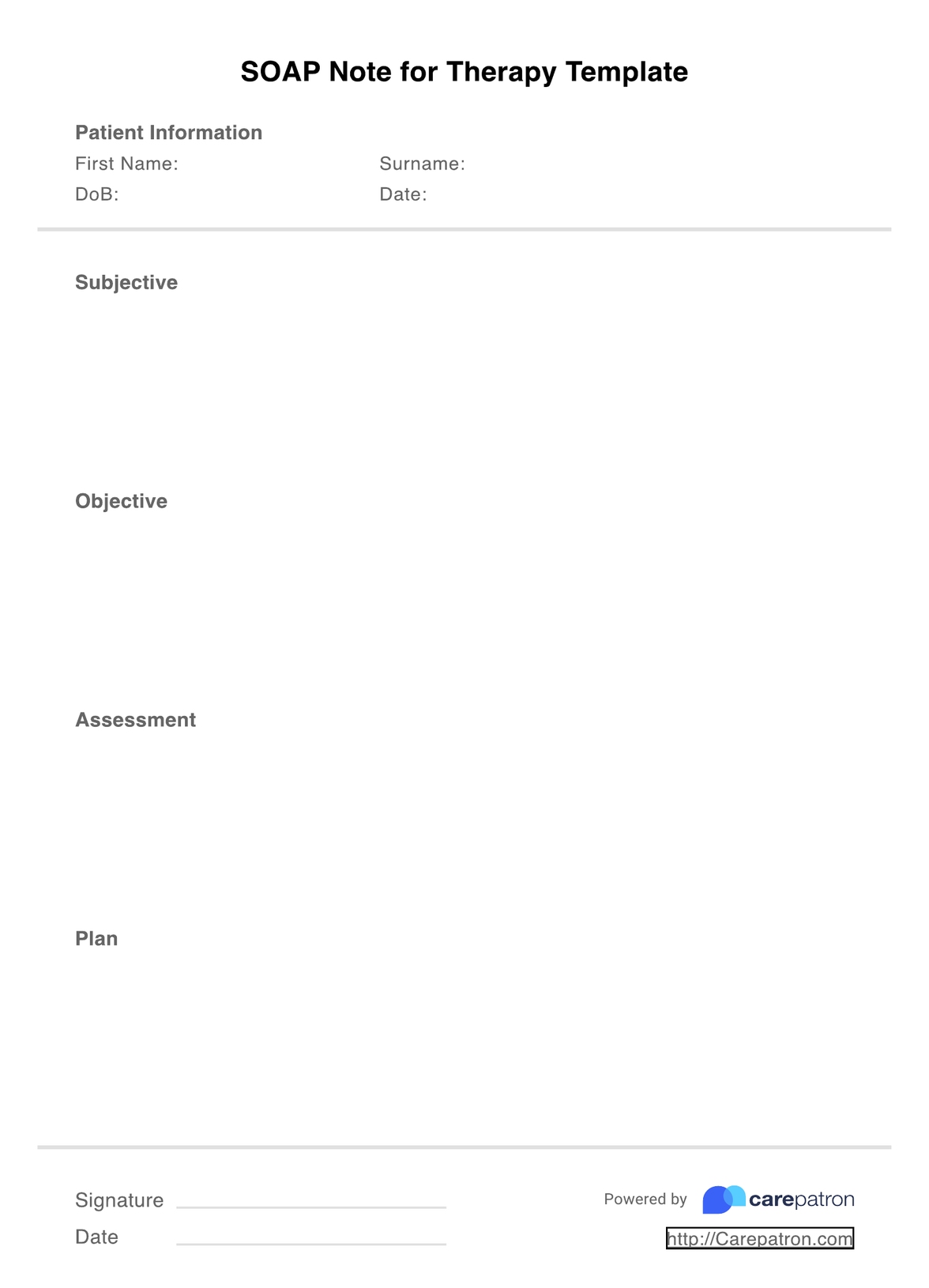
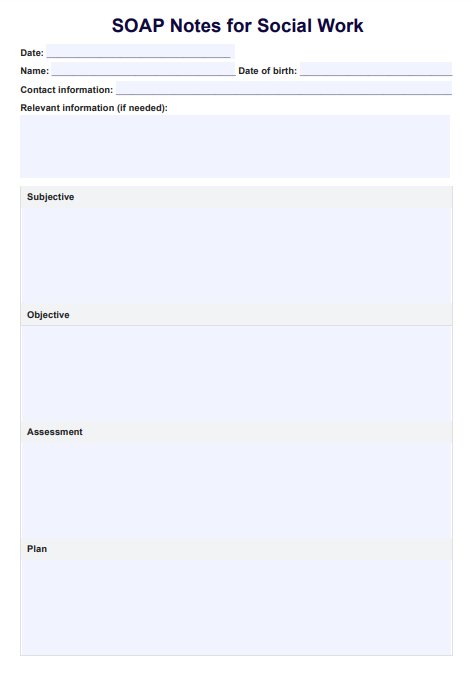
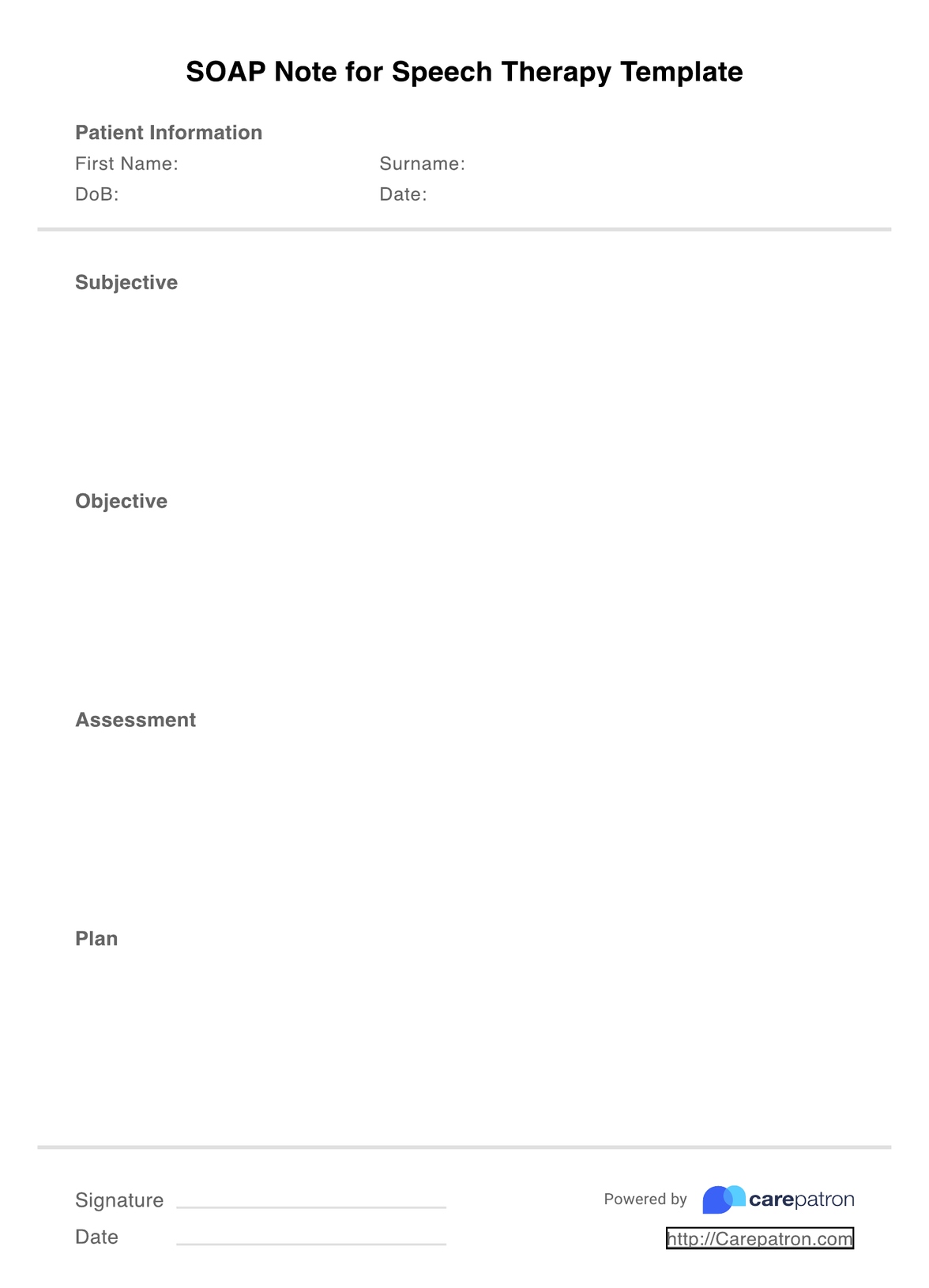
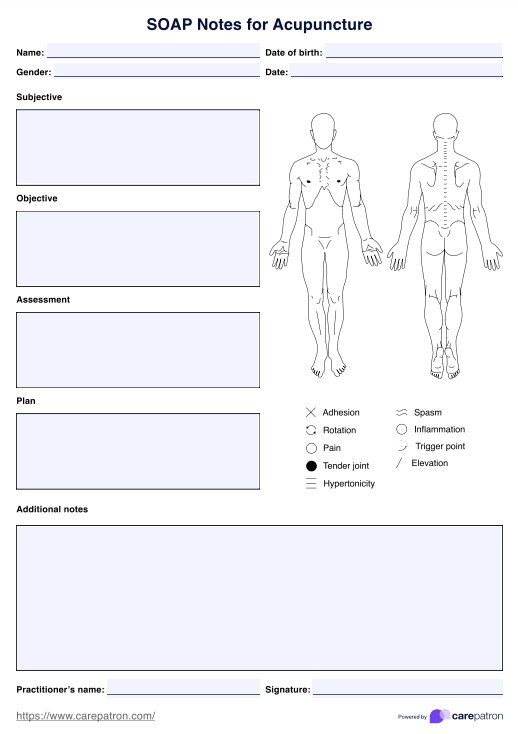
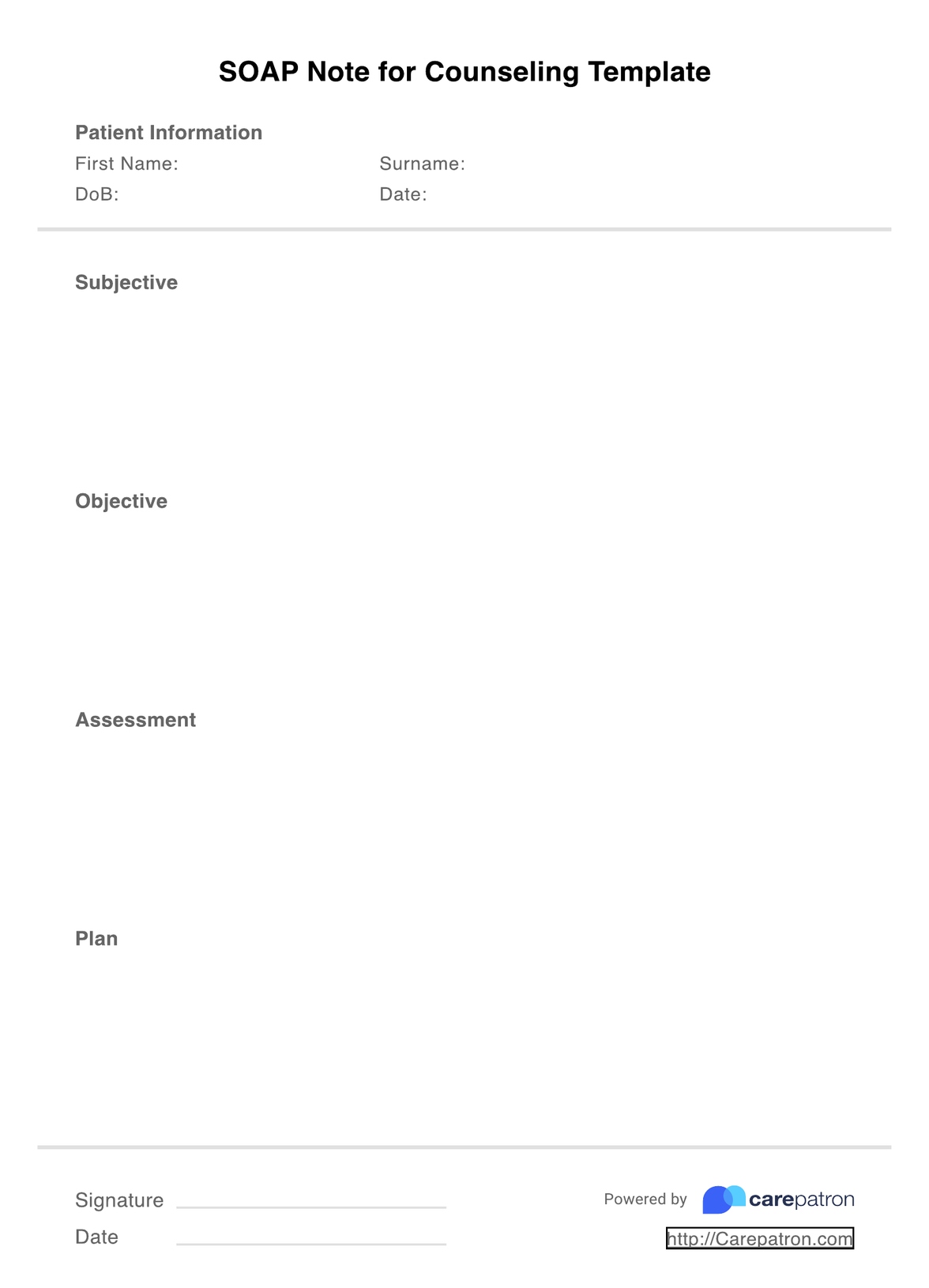
SOAP stands for the four comprehensive subjective, objective, assessment, and plan sections, all of which utilize an evidence-based approach to demonstrate sound judgments. They encompass the following:
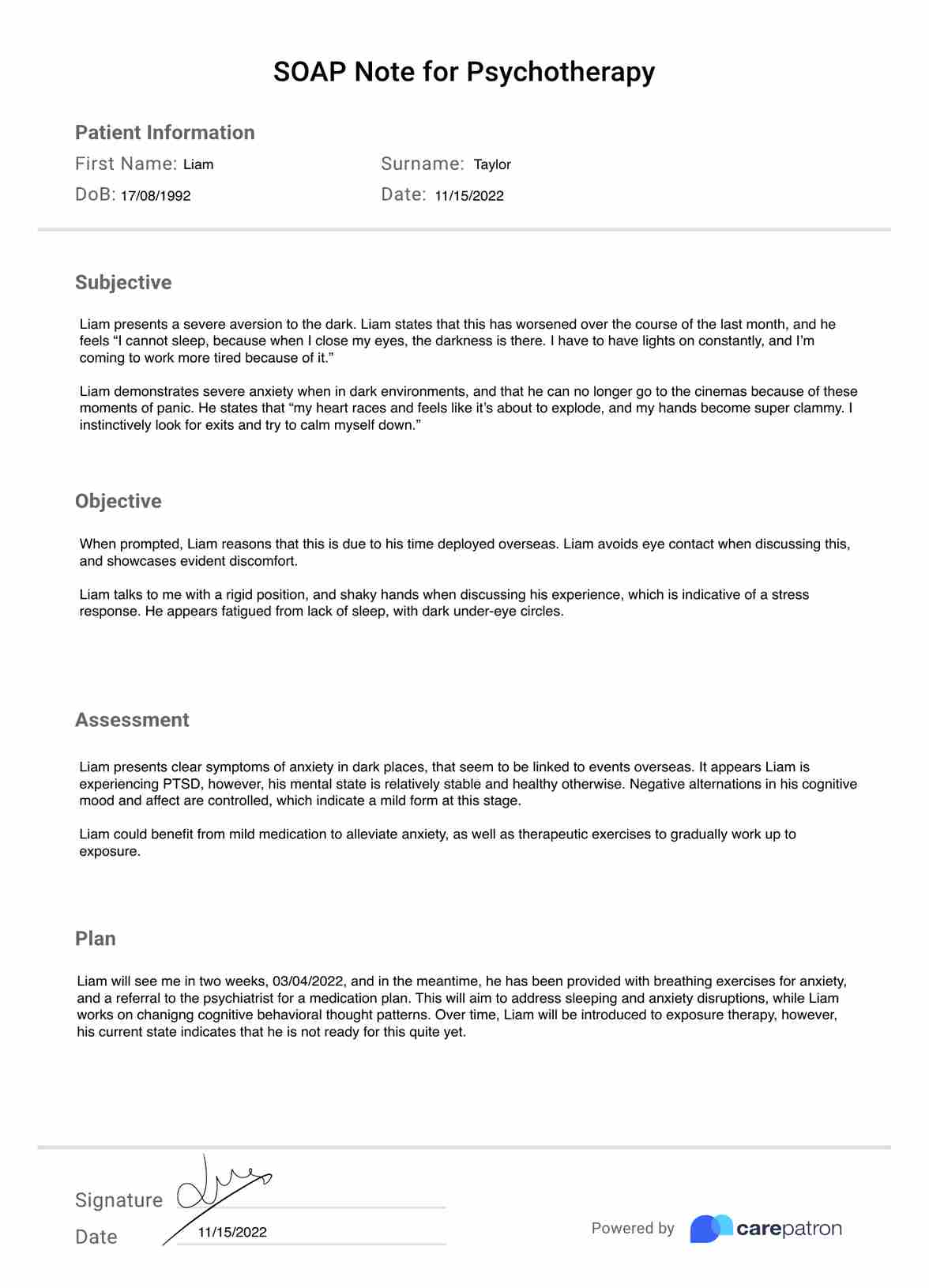
Subjective: The client’s description of their symptoms, experiences, and feelings, which can also be supported by quotes from close relations.
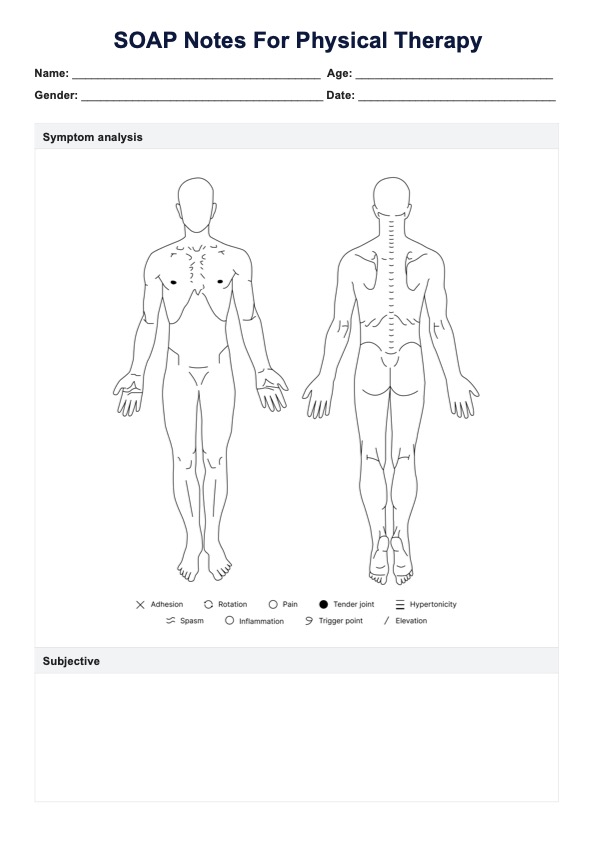
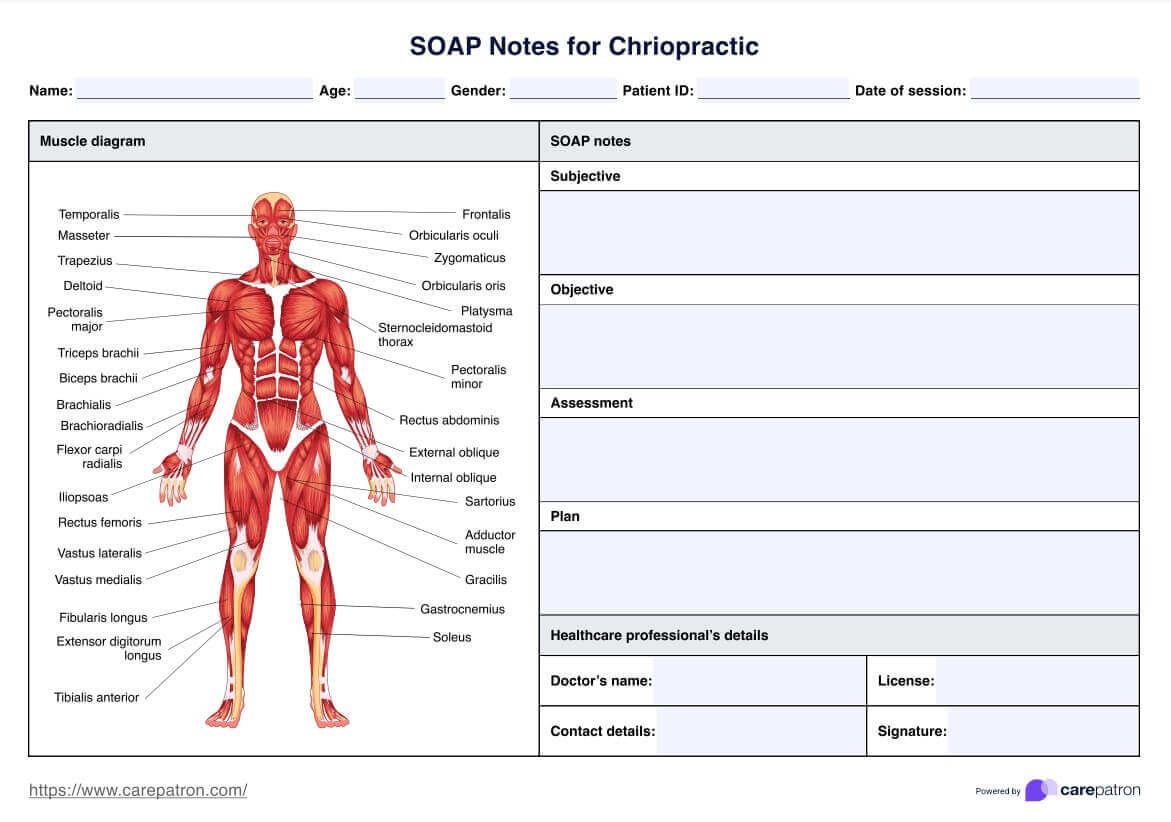
Objective: This includes professional opinions of their condition through quantifiable and measurable data, such as vital signs, medical records, history, and x-rays.
Assessment: This combines the previous two sections, and also includes any treatment goals or current progress made.
Plan: As the final section, this concerns the future course of action for the client, which may entail amendments to the current plan.
You can make more informed decisions when it comes to patient progress, and elevate the quality of care within your practice. Additionally, you can also provide high-quality evidence for potential insurance claims and legal cases.
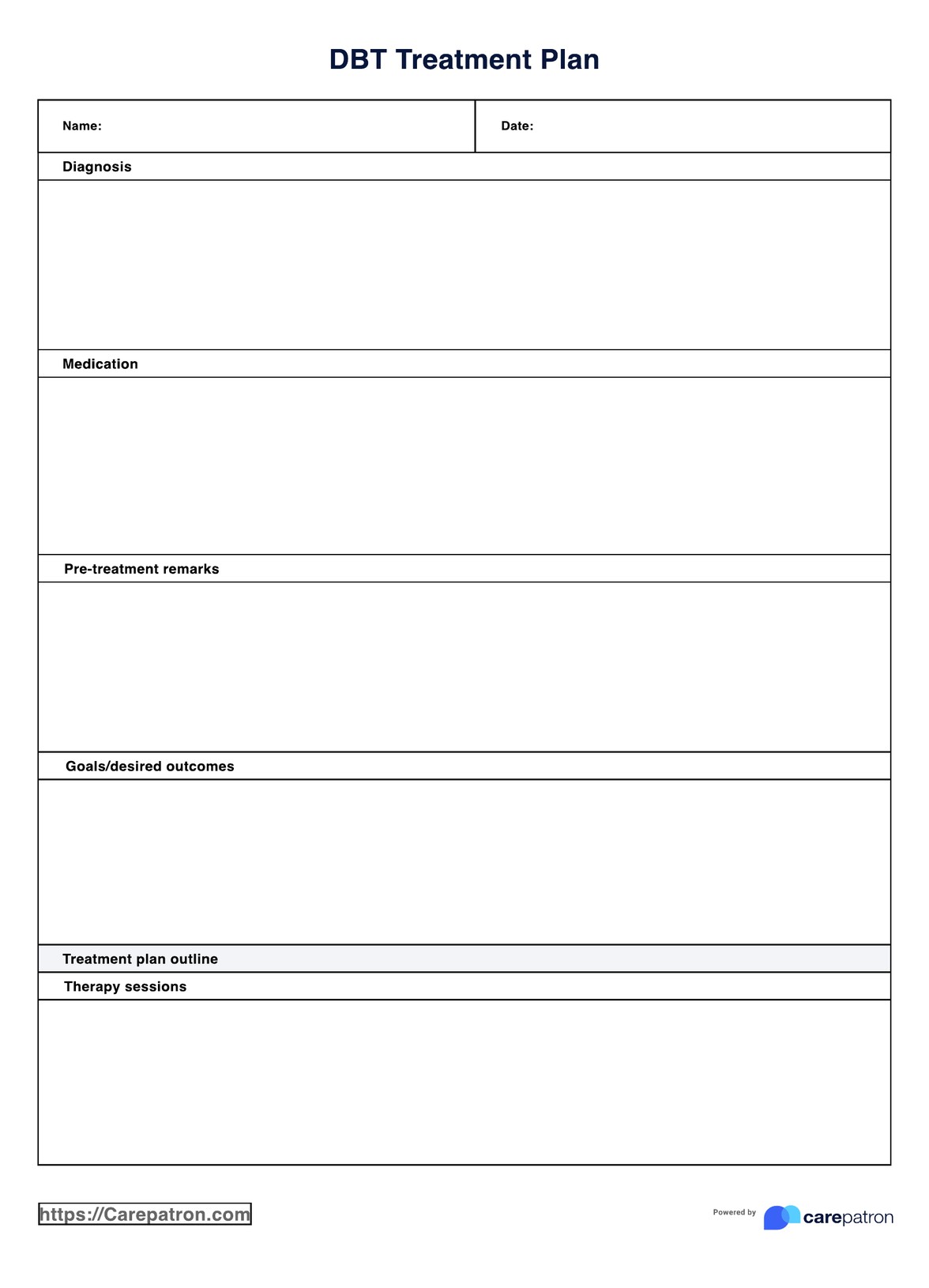
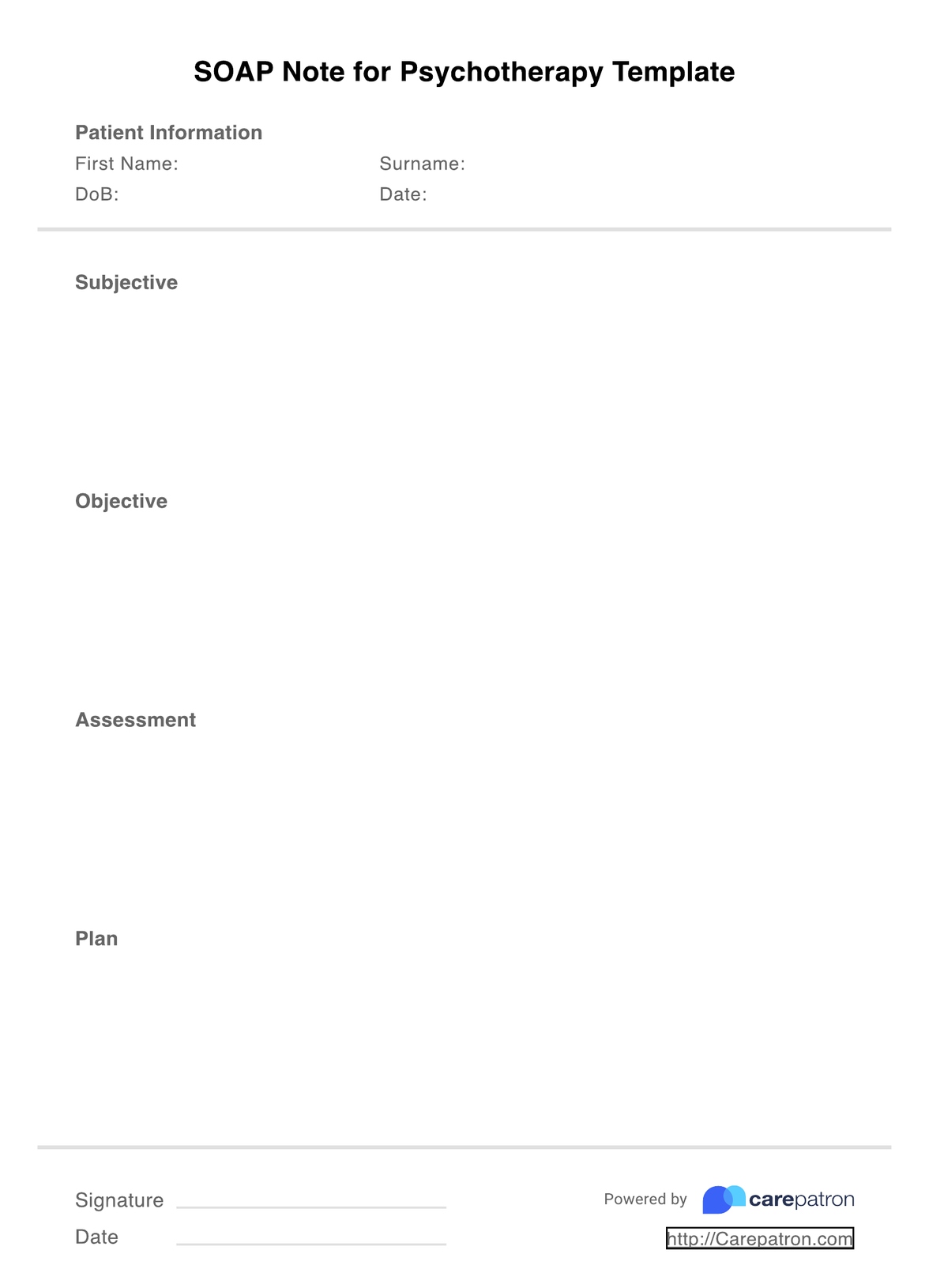
SOAP Notes for Psychotherapy Template
SOAP Notes for Psychotherapy Template Example
How to use this SOAP Note Template for Psychotherapy
As mentioned, SOAP notes for psychotherapy practices cover a broad base of essential information pertaining to the subjective, objective, assessment, and plan areas. The template itself is simple, and focuses on these four sections, with accompanying information added to establish authority. To ensure you’re utilizing them correctly, here’s a step-by-step guide!
Step One: Download the template
Click on the link to download the PDF SOAP note template, and open it up in your PDF software. This should be an automatic process, and your software should also enable you to edit the document.
Step Two: Fill in your credentials
To aid in insurance and billing processes, as well as to establish expertise, you must first fill in the time and date of your session, in addition to the name and ID of your patient (if applicable).
Step Three: Complete the four sections
Fill out the four subjective, objective, assessment, and plan sections in as much relevant detail as possible. However, do remember that conciseness is key, and all parts should be concise in nature.
Step Four: Sign the document
For greater credibility, and to signify completion, it is recommended that you sign the document with your initials. That way, fellow healthcare professionals can attribute the information to exactly who wrote it, including any amendments made.
Step Five: Securely store your SOAP notes
After you complete your SOAP note, keep it in a secure place. Ideally, this is within a practice management platform that provides a place for you to store the documents in a HIPAA-compliant manner. This will significantly protect your business (and your patient’s confidential data) against future hacks and security breaches.
Who Can Use this Psychotherapy Template?
Because psychotherapy is a broad umbrella for a variety of mental health professionals, this means many practitioners can benefit from implementing this template within their business. It is a universal template, so regardless of your exact specialization and if you’re in the psychotherapy or mental health realm, you can elevate the quality and standard of your notes with its structure. With this template, you can better understand the condition, behaviors, and feelings of your clients.
Multiple healthcare professionals in the psychotherapy space can access and take advantage of the benefits this template has to offer:
- Psychologists
- Cognitive behavioral therapists
- Dialectical behavioral therapists
- Holistic therapists
- Psychodynamic therapists
- Humanistic therapists
- Clinicians
- Counselors
- Psychiatrists
- Addiction therapist
- Social counselor
While these areas are highly specialized, because of SOAP’s formatting, all of these professionals can incorporate them within their healthcare spaces. The content of each section is likely to look quite different from the other, especially depending on the level of introspection and assessment needed. Some disciplines may require more technical evidence than others, and that is completely fine. However, it is important to note that as a psychotherapist, you must be clear and concise with your SOAP note, and take care that you’re evaluating the client in all required aspects.
Why is this Template Useful for Psychotherapists
There are multiple reasons why this SOAP note template is useful to psychotherapists. It organizes and structures your clinical information in a way that is easily accessible to other healthcare professionals, and means that you can facilitate more effective treatment plans for patient mental health conditions.
- Greater standardization: SOAP notes provide a more structured format for note-taking across all of your patients. This means that you’re able to approach each case with the same knowledge base, and with the same level of care. You can have a much higher level of consistency with each client, which is always welcome.
- Simplified planning: Because SOAP notes have a dedicated section for each type of assessment and evaluation, you don’t have to put any thought into how you structure your notes. It’s already done for you! All bases are covered, which provides you with the perfect template to build comprehensive clinical documents.
- Easy referencing: SOAP notes are laid out with all personal details displayed for easy access. You can quickly build a library of psychotherapy solutions, and make references to cases whenever needed.
.png)
Benefits of Using the Psychotherapy SOAP Note Template
There are also multiple benefits that can advance your psychotherapy business beyond its current scope, and into the broader clinical context. Incorporating this SOAP note template means that you streamline your administration, and make sure you’re getting it right every time.
Save time
One of the most valuable components of SOAP notes is that you can cut down on time significantly. You don’t have to spend any extra time in the planning process, as all the essential details are there for you! You can save money, and put it towards other operations and increase business value.
Greater accountability
SOAP notes not only are a brilliant way to keep track of a client’s health progress, but they also hold you accountable for your actions. They can serve as excellent evidence for legal and insurance cases, and they result in a great opportunity for you to demonstrate a high level of responsibility and expertise.
Improved communication
Because of SOAP notes’ comprehensive nature, you can ensure that all relevant and critical details are noted down. In turn, you can have more meaningful professional connections with clients, and improved communication. Communication goes a long way in healthcare, and so any chance to build on this asset is a welcome one.
Simplified workflow
As simple as it is, never underestimate an easy workflow. With SOAP notes, you can produce the same level of quality notes, if not more, and at a much faster rate. Creating clinical documents has never been easier, with it leaving you more room to attend to other important business operations.
Effective tracking
Naturally, utilizing SOAP notes in your psychotherapy practice can elevate the monitoring of your patients, which only works towards more effective treatment. You can track their mental health progress over time, and draft specific treatment plans for higher clinical outcomes.
Commonly asked questions
Yes, you can include names if needed, although this is not entirely essential. You should, however, absolutely include the name of the client you’re seeing.
SOAP notes can differ in length, however, a general rule is to keep them to 1-2 pages. Going beyond this isn’t necessary, and remember that you want to keep them concise.
Yes, you can include images if they are relevant to your client's condition. Images may include x-ray results or any other supporting evidence that adds value to your assessment. Being concise is absolutely key, so be sure to only add what is necessary, as an overload of images can be confusing to analyze for other healthcare professionals.

.jpg)












-template.jpg)