SOAP Notes for Nurse Practitioner Template
Download a SOAP Notes for Nursing Template to streamline nursing documentation. Ensure clear and organized records for quality patient care.


What is a nursing SOAP notes template?
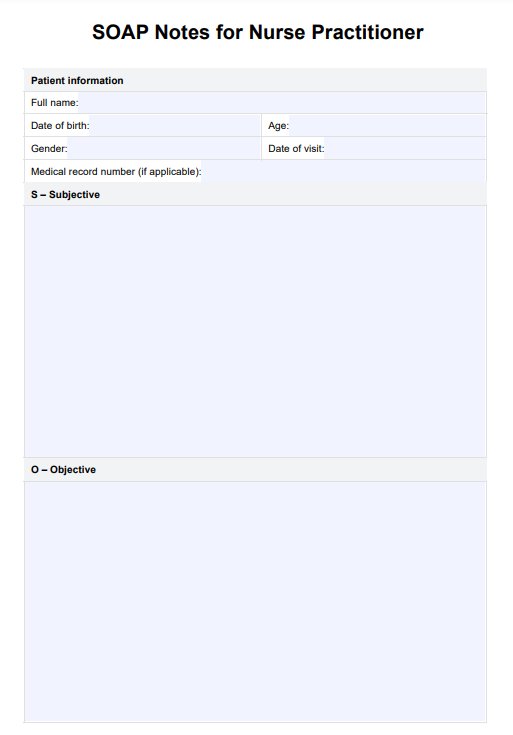
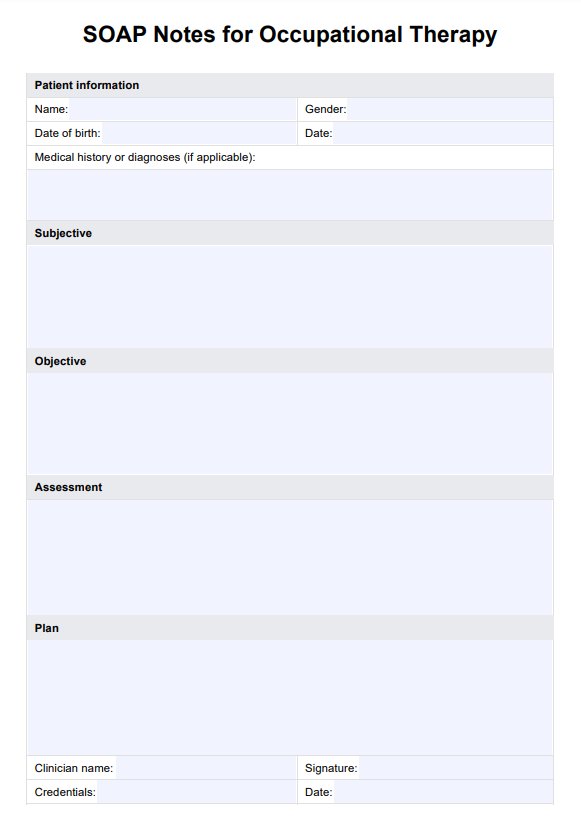
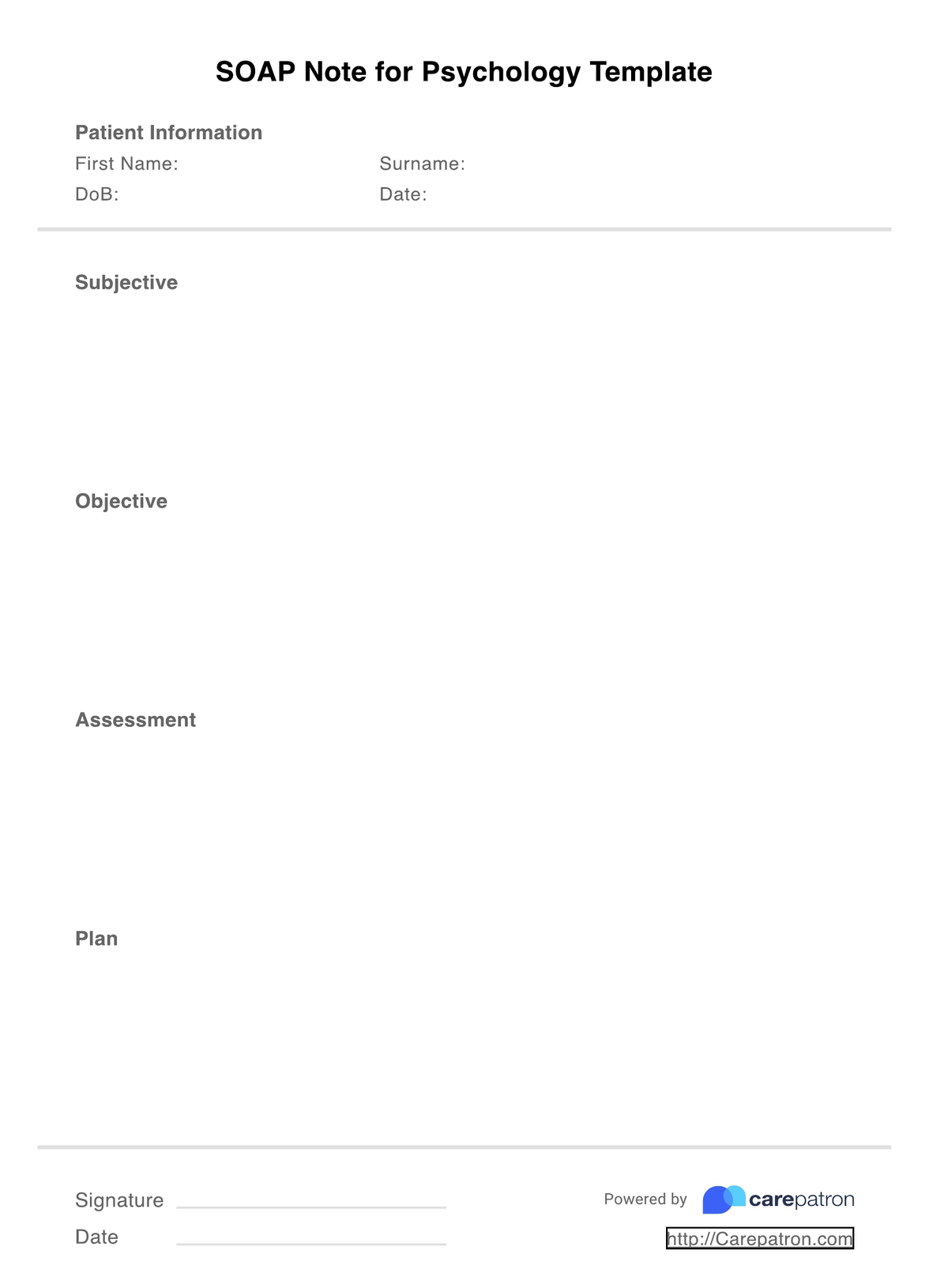
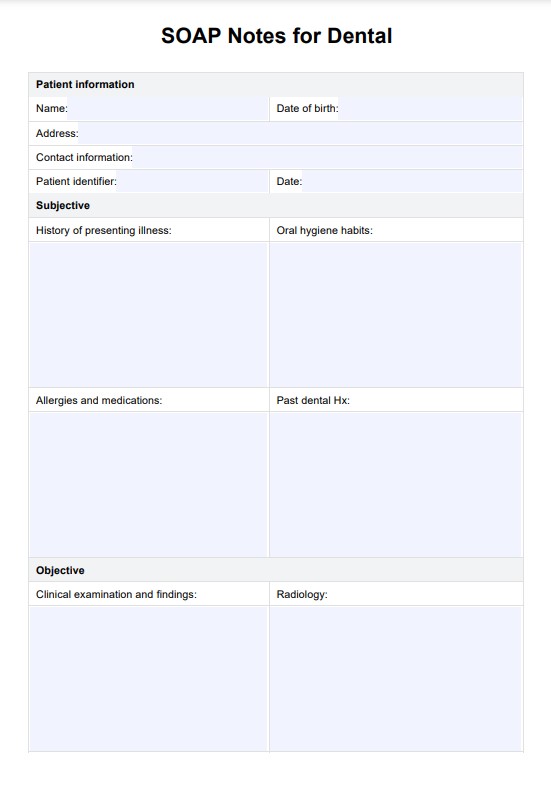
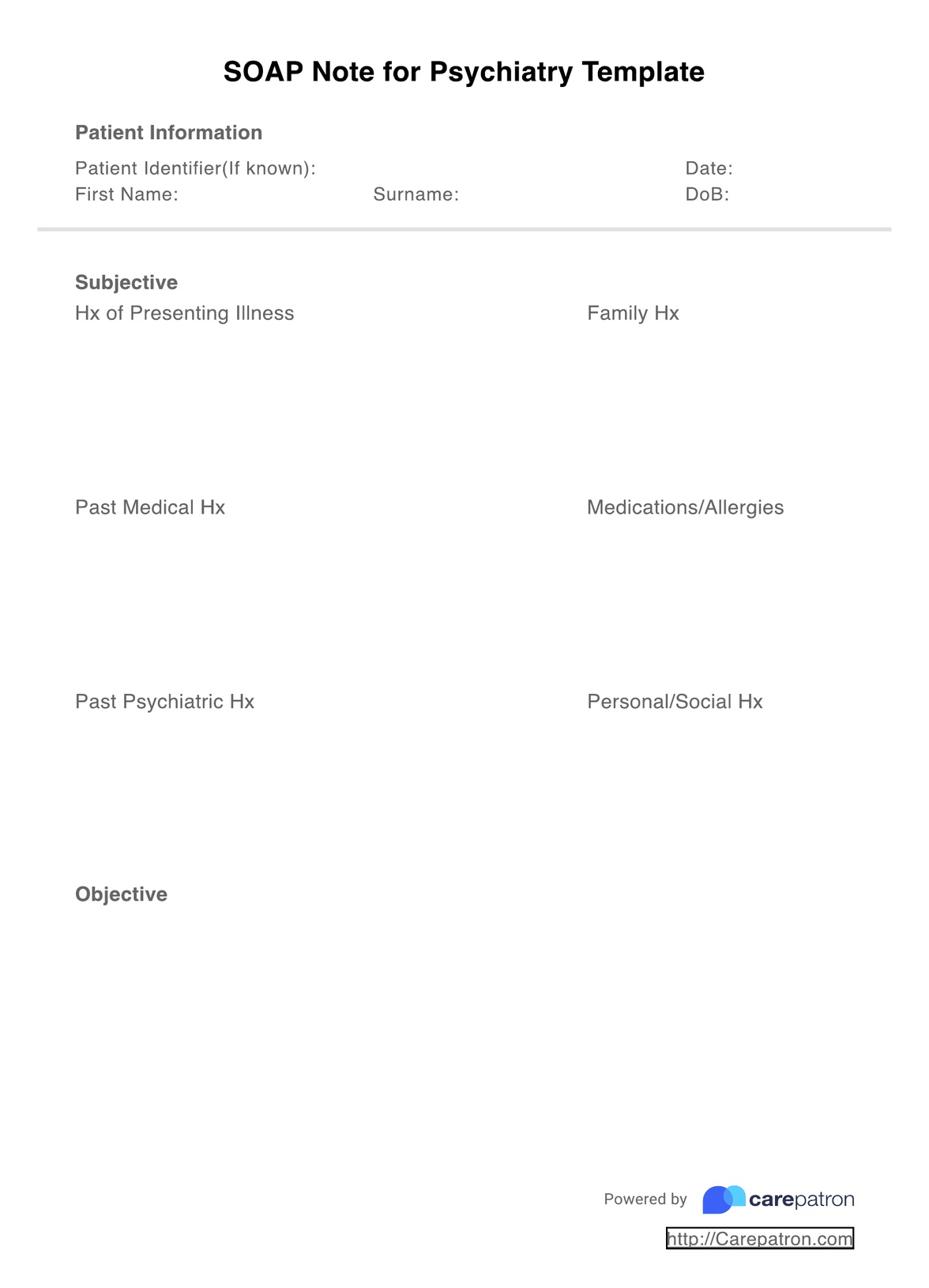
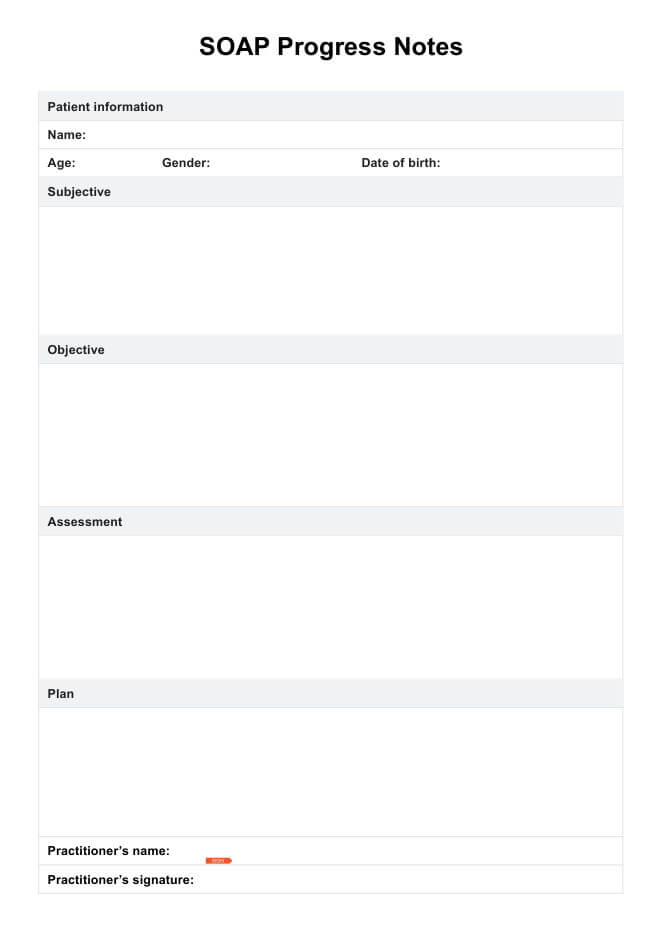
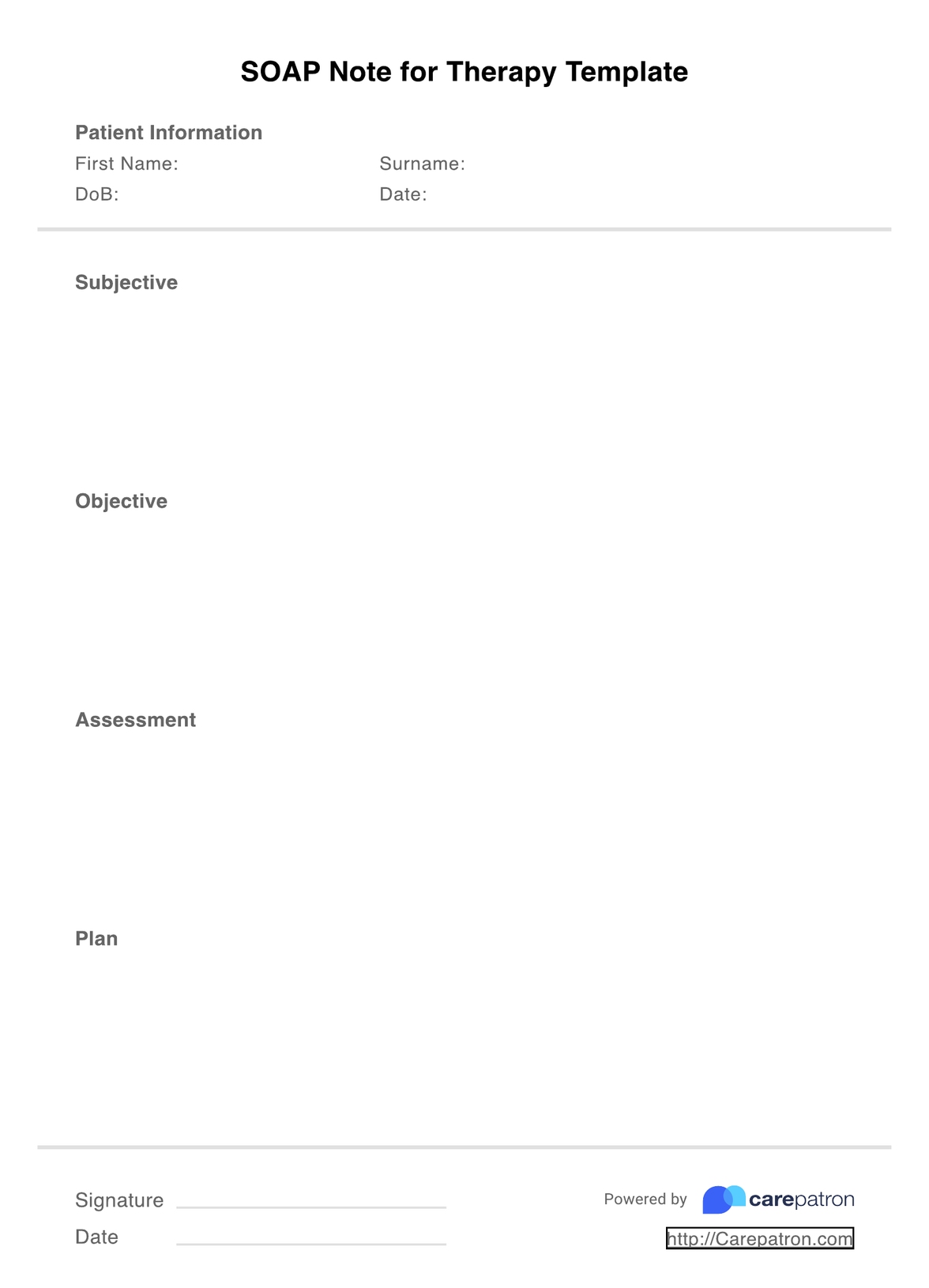
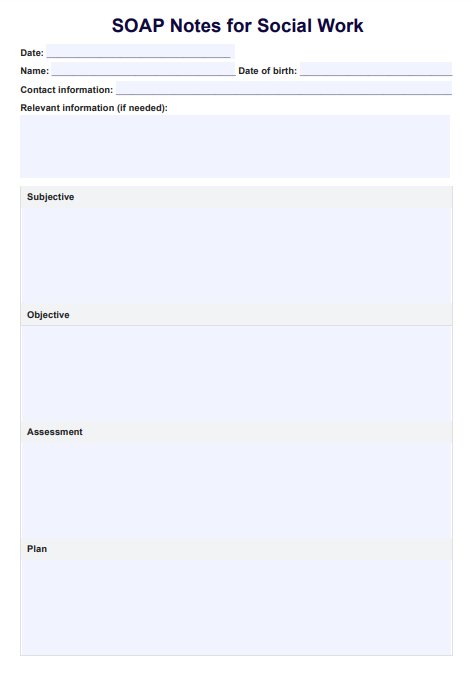
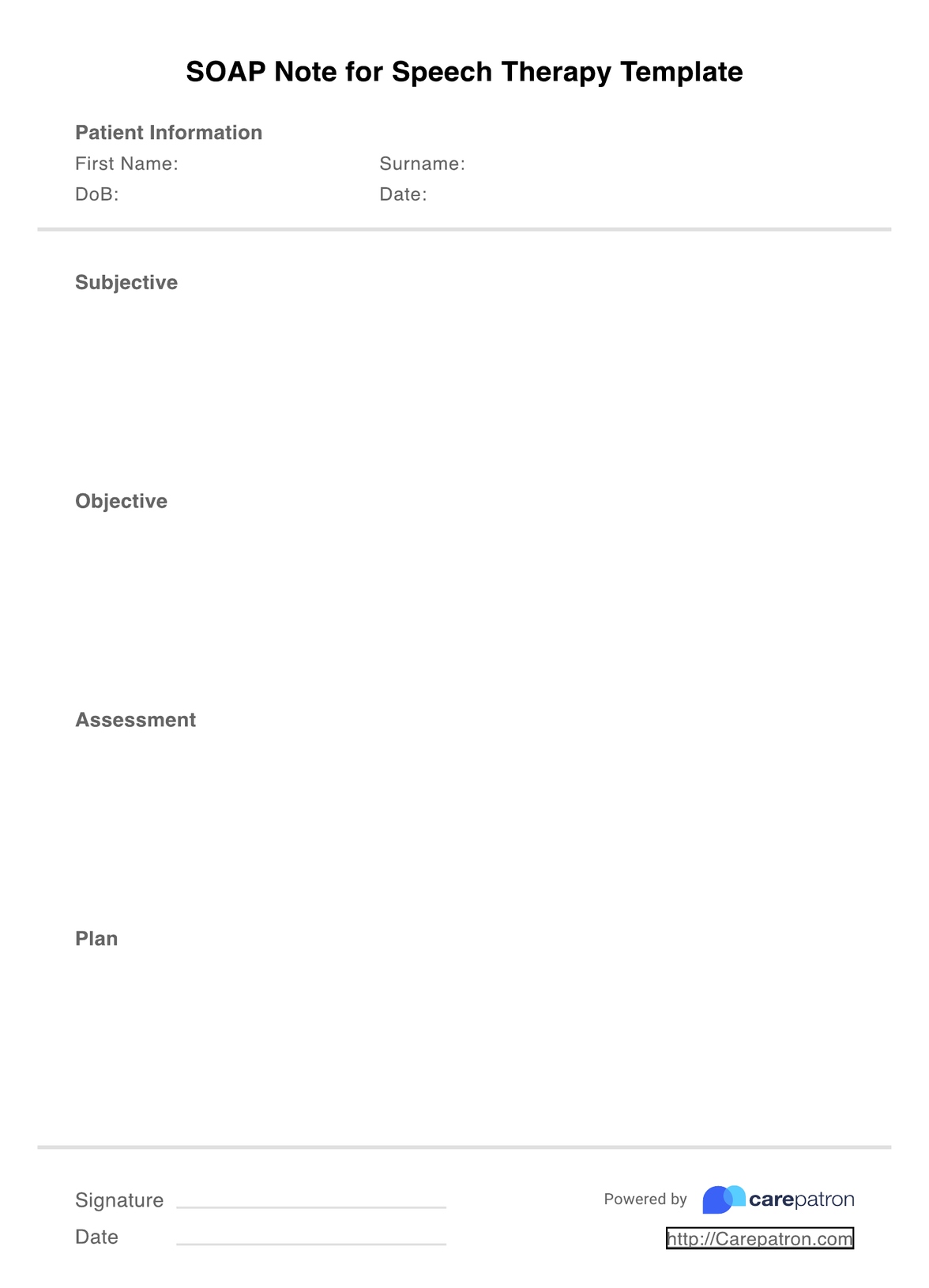
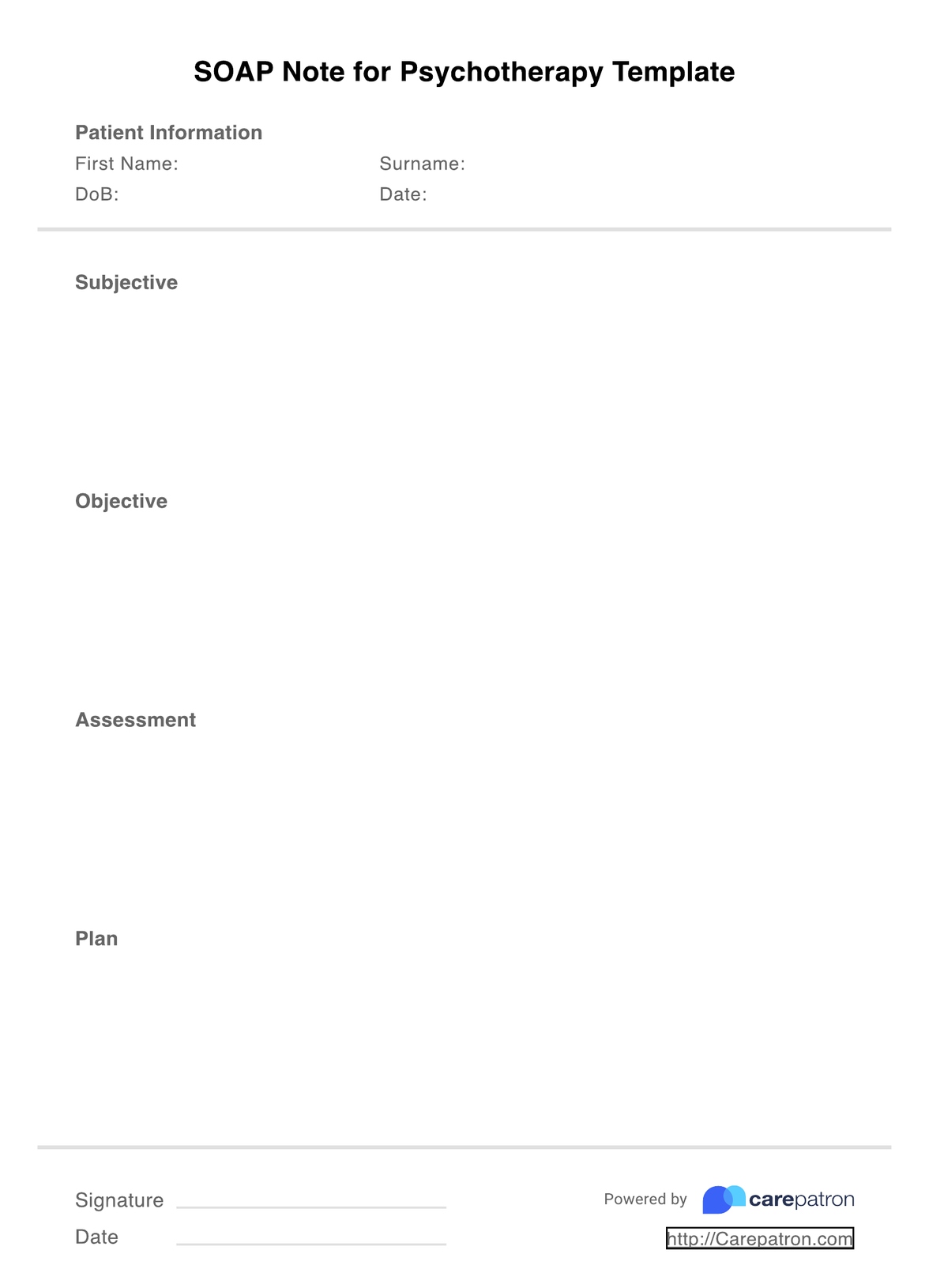
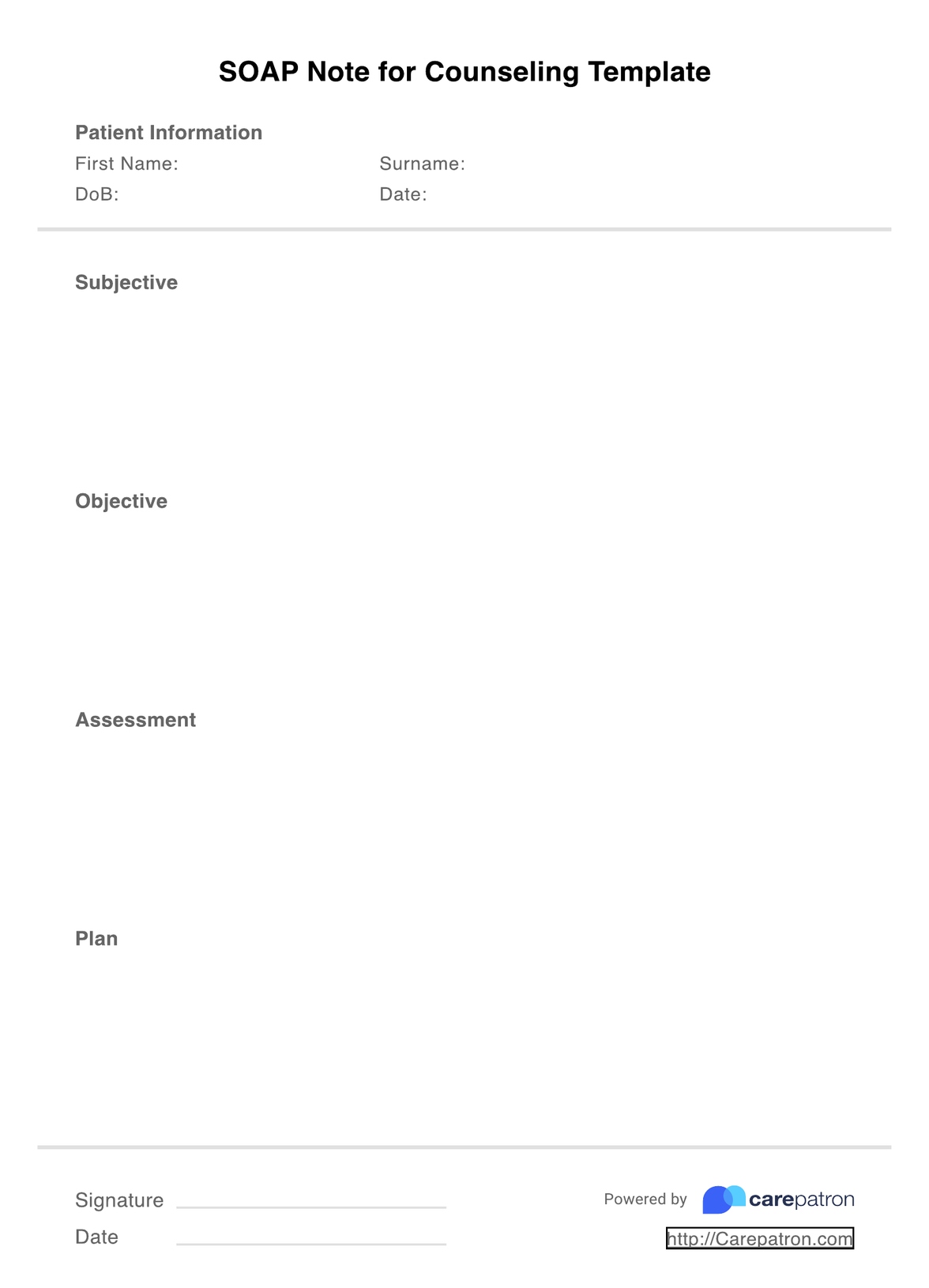
A nurse practitioner commonly uses SOAP notes to record all kinds of clinical documentation during a patient encounter or visit. The SOAP acronym stands for the four sections of the note: subjective, objective, assessment, and plan. Let's take a look at what each section should contain:
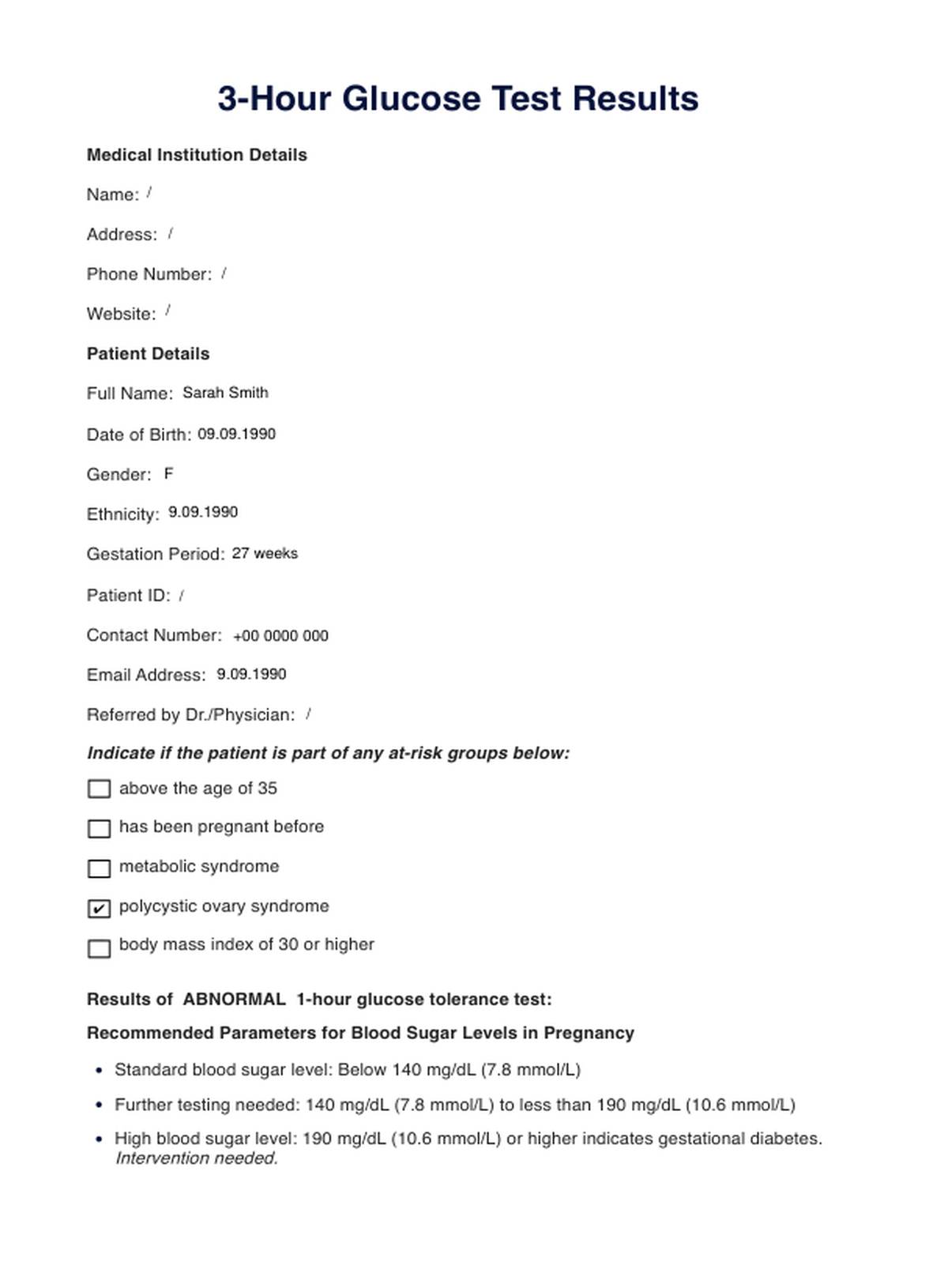
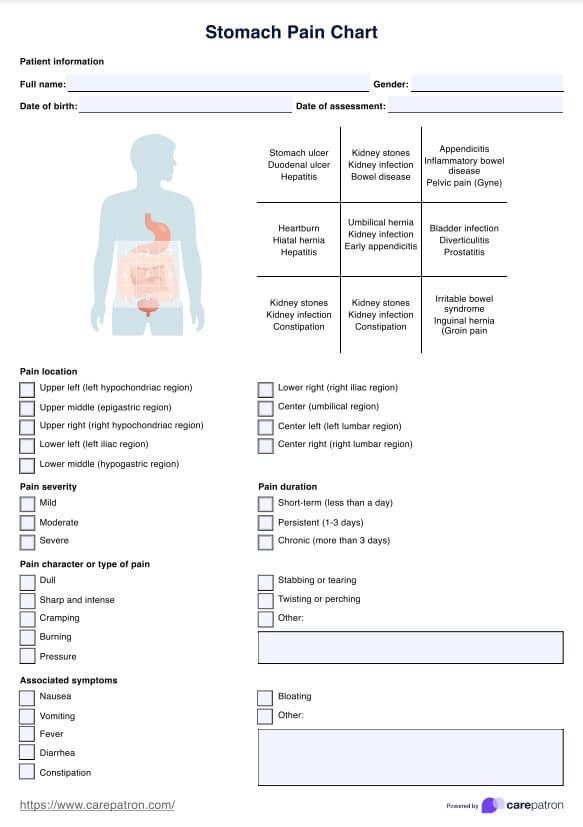
- Subjective: Here, you'll document key points about your patient's subjective experience. This includes what the patient reports, such as their chief complaint (e.g., chest pain or abdominal pain), past medical history, surgical history, social history, allergies, current medications, and any other relevant details they share about their condition or experience.
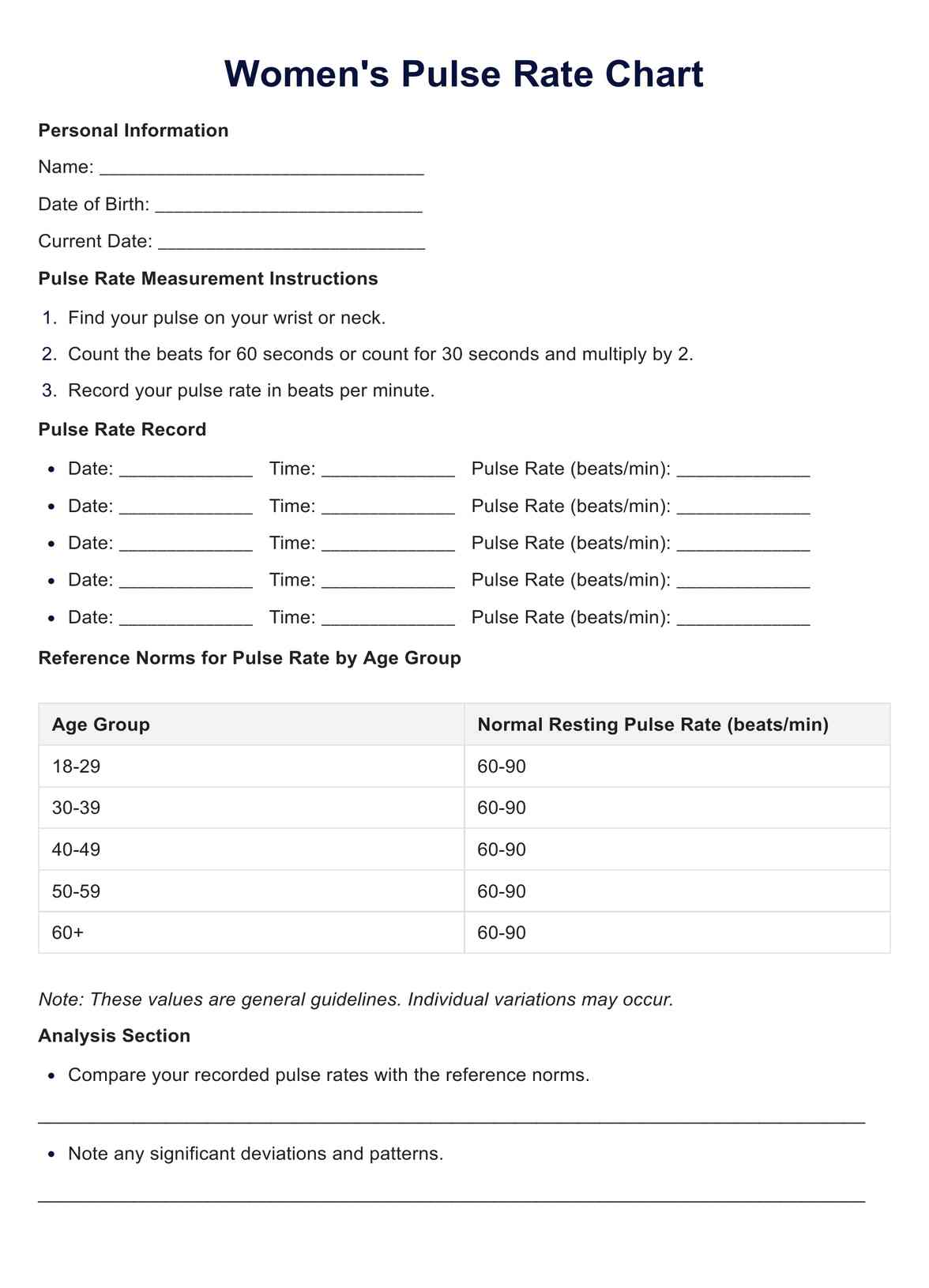
- Objective: The objective section of the SOAP note is for the information you can measure and observe. Objective data on your patient might include their vital signs, appearance, histology, radiology, or physical exam results.
- Assessment: In this section, you'll summarize your conclusions about the patient's current condition based on the subjective and objective information gathered earlier. This could take the form of a primary diagnosis with differential diagnoses or a holistic overview of the patient's issues. Strong clinical reasoning is essential to connect the findings and support your conclusions.
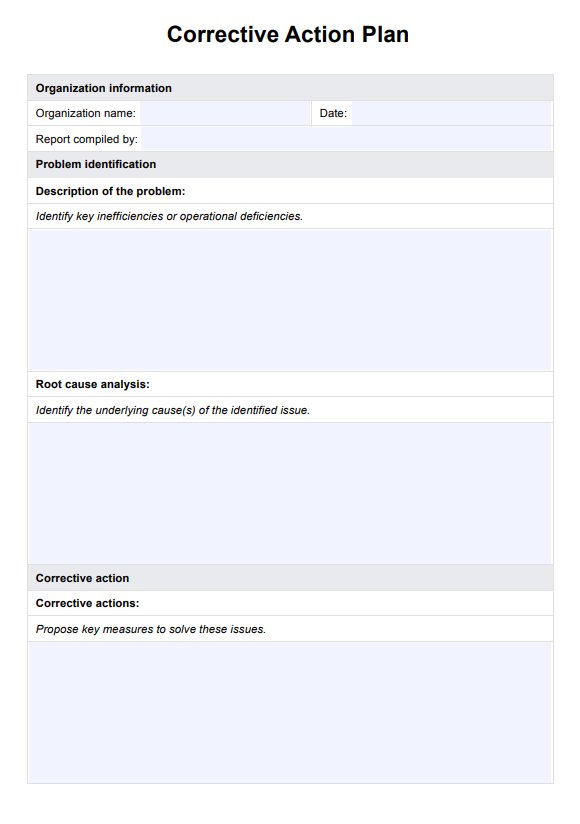
- Plan: Outline the next steps based on the identified issues for your patient. This section should detail immediate actions taken, materials provided, referrals made, prescribed medications, and any patient education offered.
Fortunately, our template already has the four sections of SOAP Notes laid out for you, with space for you to fill them in as you interact with your patient and to write down your patient's details to help them with their present illness.
SOAP Notes for Nurse Practitioner Template
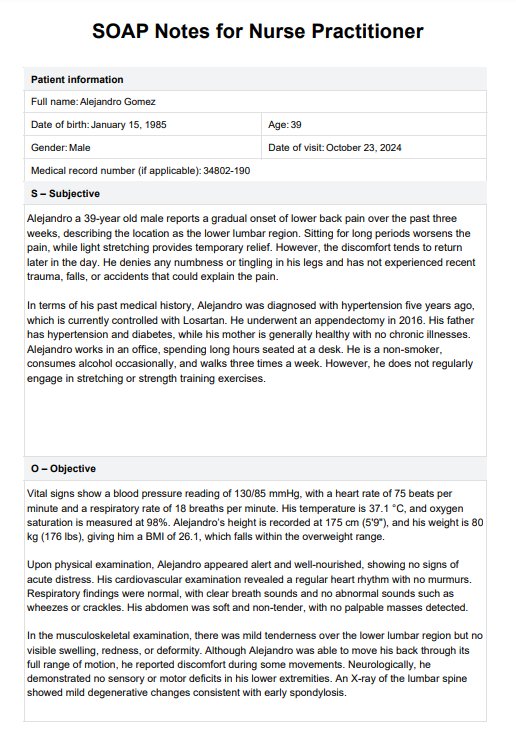
SOAP Notes for Nurse Practitioner Template Example
How to use this SOAP note template for nursing documentation
Just follow these easy steps to start incorporating this handy nursing SOAP Note template into your nursing practice during patient encounters:
Step 1: Get the template
This template can be downloaded as a PDF or used within the Carepatron workspace. If you are using the PDF version, hit download and edit the PDF digitally, or print it out and write a copy on paper by hand.
Step 2: Fill out patient information
As we're sure you know, before you start making your clinical notes, you must ensure you've got the right patient. Write their name, date of birth, and other important information before you get into the rest of the template.
Step 3: Start note-taking
Start with the subjective section and continue working down the body of the template. Your time spent on each section depends on your clinical judgment of what is relevant. It is important to note both subjective and objective data so you can properly provide a diagnosis and a differential diagnosis.
Step 4: File your notes somewhere safe, secure, and accessible
Once you've completed the nurse practitioner soap note template, the final thing to do is ensure you file the finished document somewhere secure, as it is required under HIPAA. This place should also be easily accessible by the rest of your patient's team. By using the PDF in its digital version or in the Carepatron workspace, you can be sure your notes will be secure, accessible, and safely stored.
Benefits of this SOAP note template for nurse practitioners
Here are some of the benefits of using our SOAP Notes for Nursing Template:
Makes your note-taking more efficient
Nurse practitioners are under huge pressure to keep consistent records of the care they provide. Some nurses or nurse practitioners also need to keep records of the medications they administer or prescribe and any essential results from all their interactions with their patients throughout what can be hectic and long shifts. With all that note-taking to do, using a premade template can help ensure that your notes are consistent, comprehensive, and accurate.
Aids in risk management
With the amount of work nurses are often expected to get through in a shift, it can be challenging to remember the details of every patient interaction. Additionally, when you are under time pressure in a busy clinic, it can be easy to forget to ask a specific question that might be useful in the future. A template that includes the commonly used SOAP sections and spaces for patient information is a great way to help ensure you're covered legally if any problems arise.
Makes document-sharing easy
Using a pre-formatted and laid-out notes template like our nursing SOAP notes template makes sharing notes with others in your patient's care team easy. The next time someone needs information from your clinical notes, they'll be able to find what they're looking for quickly.
Improves communication in your team
It is very important for the quality of your patient's care that other members of your team can easily interpret your notes. Using a template like our nursing SOAP notes template keeps your notes readable and easy for other nurses and healthcare providers to understand and pick up where you left off.
Commonly asked questions
SOAP is an acronym taught around the world because it is simple enough to remember (however, there is no need to memorize it if you have a nursing SOAP note template with the headings all there for you) and comprehensive enough that if you fill out those four sections thoroughly with key information, you'll have great clinical notes.
The four parts of SOAP are subjective, objective, assessment, and plan. These sections help organize patient information and clinical findings for clear communication.
To write a good assessment SOAP note, clearly summarize your clinical findings and thoughts about the patient's condition, linking the subjective and objective information. Use concise language and focus on key points to make your assessment clear and effective. You can find many examples of SOAP notes for nurse practitioner online.















-template.jpg)