Treatment Guidelines for Hip Fracture in Elderly Handout
Discover comprehensive treatment guidelines for hip fractures in older people. Download a free PDF handout and example for healthcare professionals.


What are hip fractures?
Hip fractures occur when the upper part of the femur breaks near the hip joint. These fractures are particularly prevalent in the elderly due to weaker bones and a higher risk of falls. Understanding the causes, symptoms, and types of hip fractures is crucial for effective treatment and recovery.
Causes
Hip fractures in elderly patients are primarily caused by falls, often from a standing height. Osteoporosis, a condition that weakens bones, significantly increases the risk of most hip fractures anyway. Additional factors contributing to hip fractures include:
- Poor balance
- Impaired vision
- Medications that affect bone density
- Environmental hazards (e.g., loose rugs, poor lighting)
- Muscle weakness and frailty
Symptoms
Symptoms of a hip fracture include:
- Severe pain in the hip or groin
- Inability to put weight on the affected leg
- Bruising and swelling around the hip area
- Deformity or abnormal positioning of the leg
- Shortened or outwardly rotated leg on the affected side
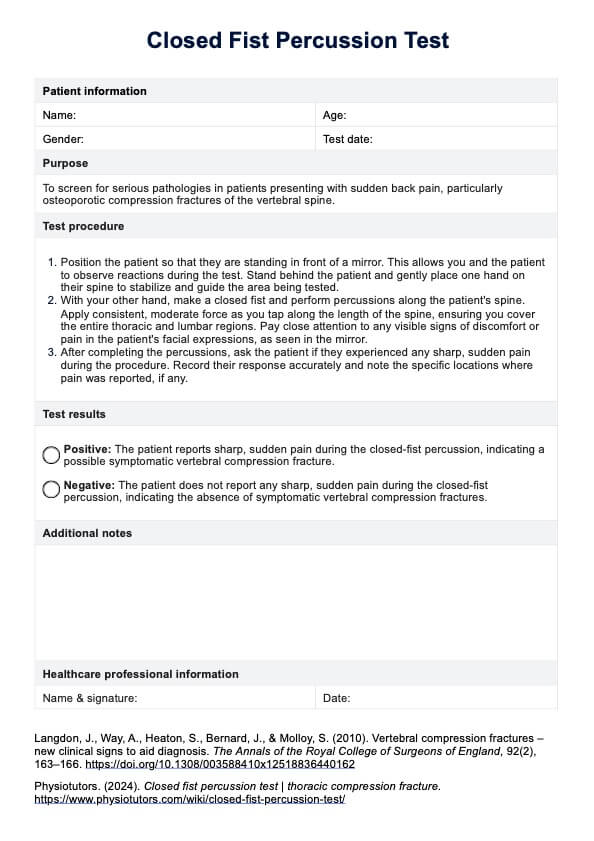
Treatment Guidelines for Hip Fracture in Elderly Handout Template
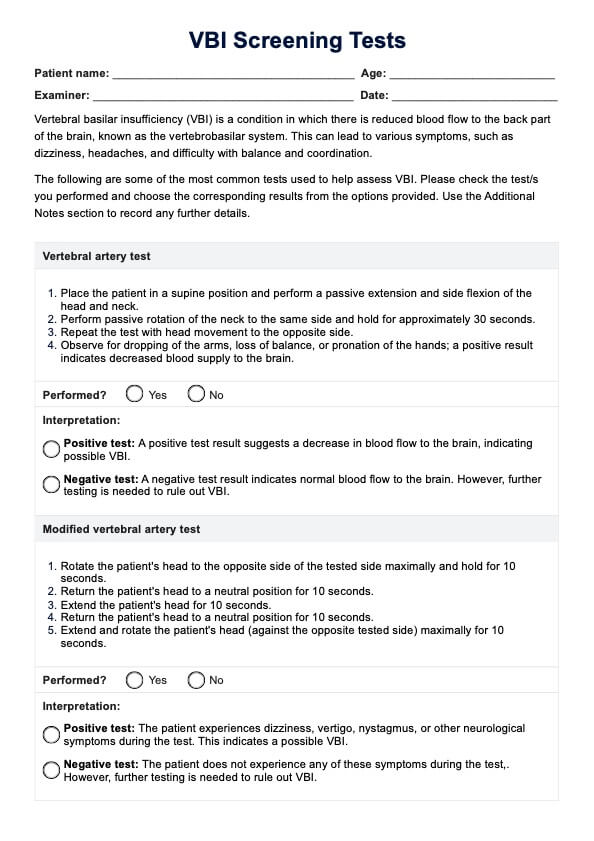
Treatment Guidelines for Hip Fracture in Elderly Handout Example
How to manage and treat hip fractures in elderly
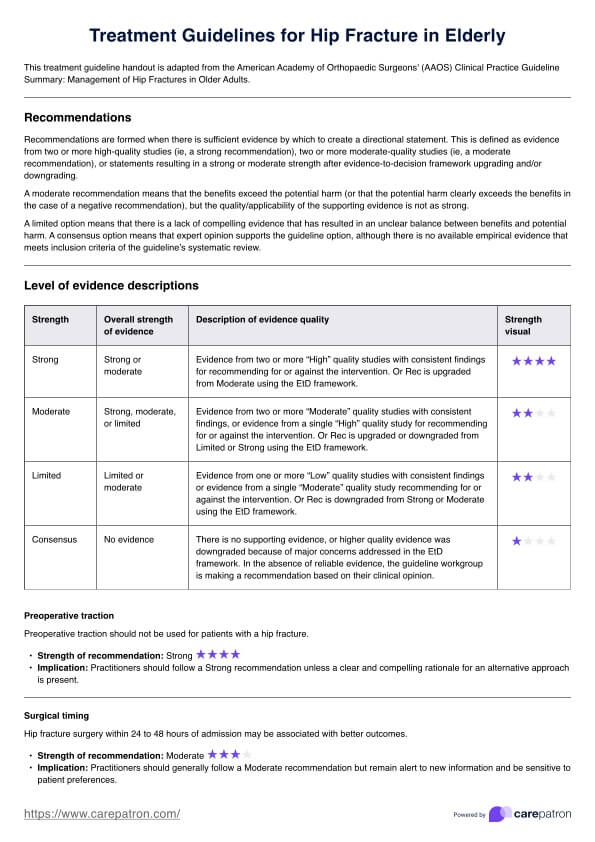
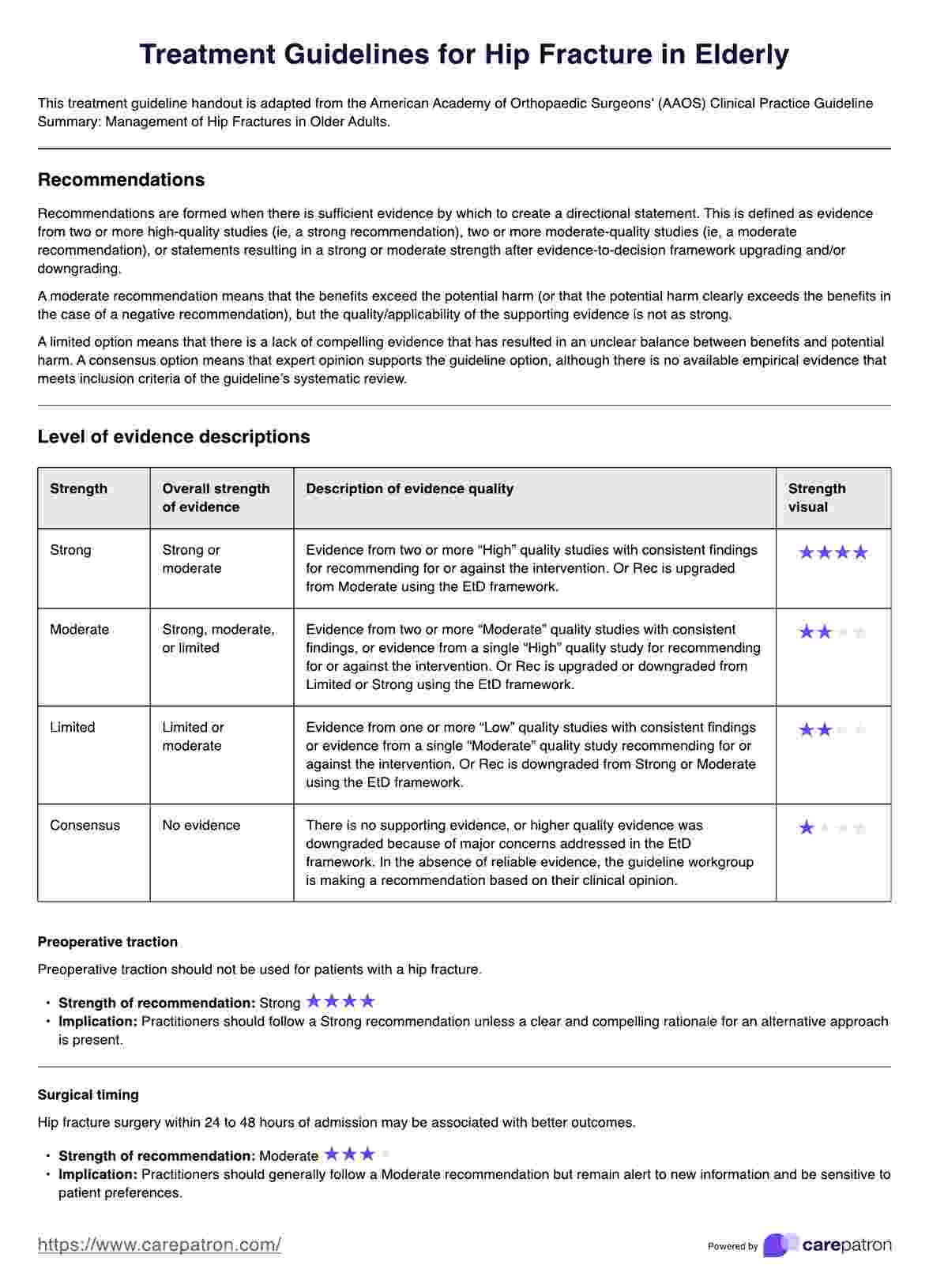
Hip fractures in elderly patients are a significant health concern that requires prompt and effective management to minimize complications and enhance recovery. Given the complexity of treating these fractures, the American Academy of Orthopaedic Surgeons (2021) recommends an approach involving timely surgery, appropriate anesthesia, postoperative care, rehabilitation, and preventive measures is crucial.
Surgical management
Timely surgical intervention is critical for elderly patients with hip fractures. Surgery for hip pain should ideally be performed within 48 hours of hospital admission to reduce the risk of complications such as mortality, prolonged pain, and extended hospital stays. Delaying surgery beyond this window can significantly increase these risks, making early surgical intervention a priority.
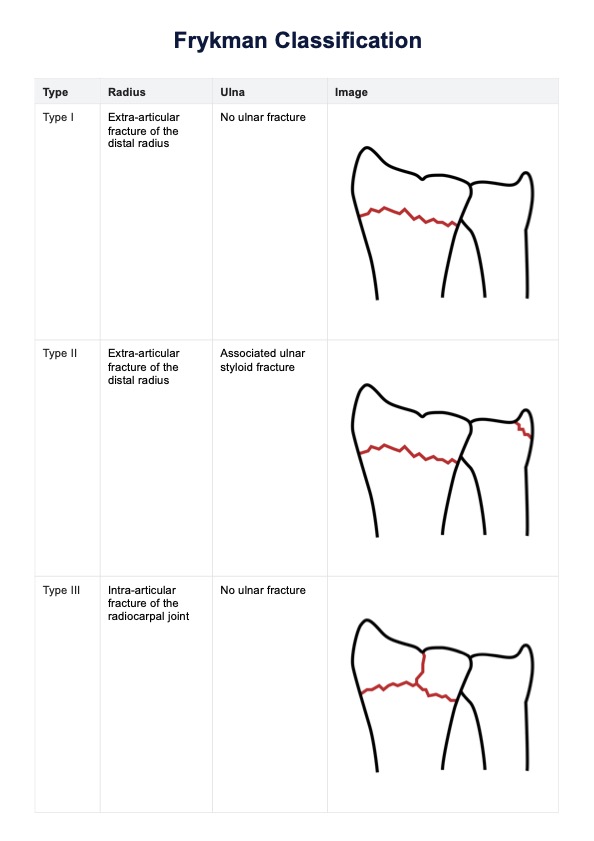
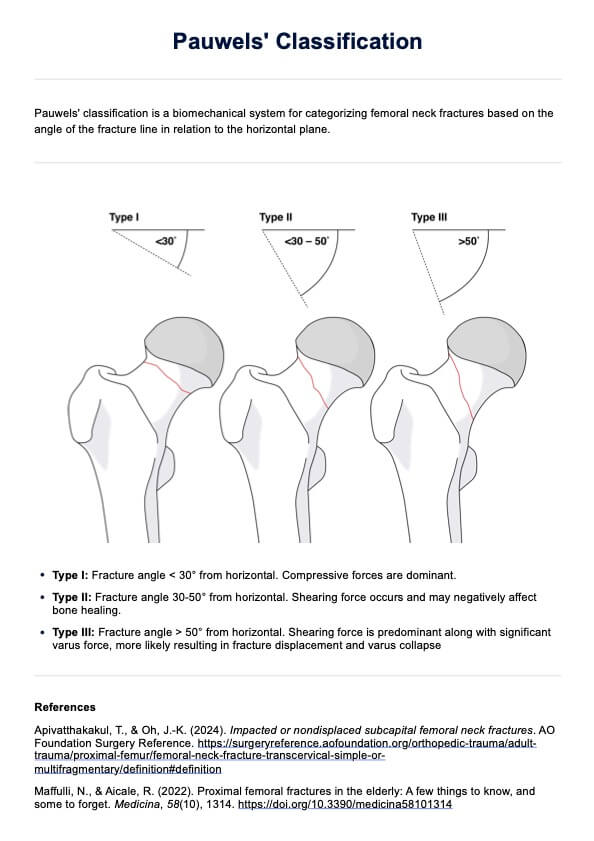
The type of surgery performed depends on the specific nature of the hip fracture:
- Femoral neck fractures: Hemiarthroplasty, preferred for patients with significant comorbidities or lower activity levels, involves replacing the femoral head with a prosthesis. Total Hip Arthroplasty (THA), on the other hand, may provide better functional outcomes for healthier and more active patients but carries a higher risk of complications. Internal fixation, considered for younger patients or those with non-displaced fractures, involves stabilizing the fracture with screws or plates.
- Intertrochanteric fractures: Ephalomedullaryy nail is recommended for both stable and unstable fractures due to its ability to provide better stability and facilitate early mobilization.
- Subtrochanteric and reverse obliquity fractures: Cephalomedullary devices are strongly recommended for providing high stability and effectiveness in treatment.
For elderly patients undergoing hip fracture surgery, regional anesthesia (such as spinal or epidural anesthesia) is generally preferred over general anesthesia due to the lower risk of postoperative complications and better pain management associated with regional anesthesia.
Postoperative management
Effective pain management is essential for recovery after hip fracture surgery. A multimodal analgesia approach, including the use of preoperative nerve blocks and various postoperative pain management strategies, is recommended to control pain and improve recovery outcomes.
Managing blood levels is vital for patient recovery:
- Blood transfusion: A threshold of 8g/dL is suggested for asymptomatic postoperative patients to balance the risks and benefits of transfusions.
- Tranexamic acid: Administered during and after surgery to reduce blood loss and the need for transfusions, minimizing risks associated with significant blood loss.
Rehabilitation and interdisciplinary care
Encouraging early weight bearing as tolerated is crucial for improving mobility and reducing complications postoperatively. This approach helps hip fracture patients regain their independence and accelerates rehabilitation. Physical therapy is vital in restoring mobility and strength in elderly patients following hip fracture surgery. A tailored rehabilitation program should be initiated soon to facilitate recovery and improve outcomes.
Implementing interdisciplinary care programs involving orthopedic surgeons, geriatricians, physiotherapists, and nurses can significantly decrease complications and improve overall outcomes. This collaborative approach ensures comprehensive care and addresses the multifaceted needs of elderly patients.
Preventive measures and follow-up
Assessing and treating osteoporosis is essential to prevent future fractures. This may involve pharmacologic treatments such as bisphosphonates and ensuring adequate calcium and vitamin D intake to strengthen bones and reduce fracture risk. Implementing measures such as removing tripping hazards, installing grab bars, and improving lighting to prevent falls is crucial for elderly patients.
Moreover, regular follow-up appointments are necessary to monitor recovery progress, adjust rehabilitation plans, manage pain, and promptly manage complications. Continuous monitoring ensures that patients receive appropriate care throughout their recovery journey.
How to use our treatment guidelines handout template
Our treatment guidelines handout template for hip fractures in the elderly is designed to provide a structured and comprehensive approach to managing this severe injury. Here's a brief guide on how to use it effectively:
Step 1: Download the template
Download a copy of the Treatment Guidelines for Hip Fracture in Elderly Handout using the link on this page or via the Carepatron app.
Step 2: Use in your practice
Use the handout as a reference guide for managing hip fractures in elderly patients. It includes evidence-based recommendations from the American Academy of Orthopaedic Surgeons.
Step 3: Share with patients and caregivers
Share the handout with your patients and their caregivers to help them understand the treatment options for hip fractures. This will also empower them to play an active role in their own care.
Step 4: Keep it in your file
Keep a copy of the handout in your patient's file for future reference and to help ensure continuity of care.
Reference
American Academy of Orthopaedic Surgeons. (2021). Management of hip fractures in older adults evidence-based clinical practice guideline. https://www.aaos.org/globalassets/quality-and-practice-resources/hip-fractures-in-the-elderly/hipfxcpg.pdf
Commonly asked questions
Hip fractures in the elderly are primarily caused by falls due to osteoporosis, poor balance, and impaired vision.
Diagnosis involves a physical examination and imaging tests such as X-rays, MRI, or CT scans to confirm the fracture and its severity.
Hip fracture treatment options include surgical interventions like internal fixation, partial hip replacement, and total hip replacement, as well as non-surgical options for those who cannot undergo surgery.