How is excoriation disorder diagnosed?
To diagnose excoriation disorder, mental health professionals follow these steps:
Gather information
During the initial consultation, you may need to ask detailed questions about the individual's skin-picking behaviors. This includes inquiring about the frequency, duration, and severity of the picking episodes and any associated feelings of distress or impairment in daily functioning. You may also ask about the individual's motivations for skin-picking, such as seeking to remove perceived skin imperfections or relieve tension.
Physical examination
Following the information-gathering stage, you will conduct a thorough physical examination to assess the presence and severity of any skin lesions or damage resulting from the recurrent skin-picking behavior. This will rule out any underlying medical conditions, such as dermatological disorders or neurological conditions, that may be contributing to the individual's skin picking.
Psychological assessment
In addition to the physical examination, you will conduct a comprehensive psychological assessment to evaluate the individual's mental health history and identify any co-occurring conditions that may be related to or causing the recurrent picking behavior. This may include screening for obsessive-compulsive disorder (OCD), body dysmorphic disorder (BDD), anxiety disorders, depression, or other mental health conditions.
Diagnostic criteria
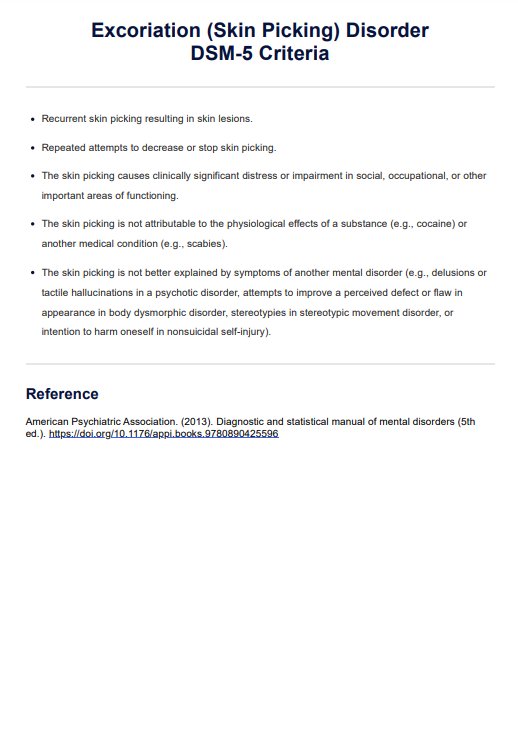
Finally, you will carefully evaluate the individual's symptoms against the diagnostic criteria for excoriation disorder as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
By following this comprehensive assessment process, mental health professionals can accurately diagnose excoriation disorder and develop an appropriate treatment plan tailored to the individual.