Pediatric Fever Guidelines
Explore our Pediatric Fever Guidelines for managing fever in children under three years, including causes, symptoms, and effective treatments.


What's considered a fever in children?
A fever in children is typically considered when they fail to maintain normal body temperature, and it rises above the normal range. Here’s an overview of a fever's causes, complications, and other signs and symptoms.
Temperature considered a fever
For children aged 1 year and older, a fever is usually defined as a body temperature of:
- 100.4°F (38°C) or higher when measured with a rectal or ear thermometer.
- 100°F (37.8°C) or higher when measured with an oral thermometer.
- 99°F (37.2°C) or higher when measured with an armpit (axillary) thermometer.
Causes of fever in children
Fevers in children can be caused by various factors, including:
- Infections: The most common cause, including viral and bacterial infections like the flu, colds, ear infections, and urinary tract infections.
- Immunizations: Some children may develop a mild fever after receiving vaccinations.
- Overheating: Excessive clothing, hot weather, or intense physical activity can sometimes raise body temperature.
- Inflammatory conditions: Conditions like rheumatoid arthritis or other inflammatory diseases can also cause fevers.
Complications of fever
While fevers are typically a sign of serious bacterial infection or viral upper respiratory infection, they can lead to complications if not managed properly:
- Febrile seizures: Some children between the ages of 6 months and 5 years may experience seizures triggered by fever, which can be alarming but are generally not harmful.
- Dehydration: Fever can lead to increased fluid loss, raising the risk of dehydration, especially if the child is not drinking enough fluids.
- Underlying conditions: Persistent or very high fevers can sometimes indicate more serious underlying health issues that require medical attention.
Other signs and symptoms
Besides an elevated temperature, other signs and symptoms that may accompany a fever in children include:
- Sweating: Increased sweating as the body tries to cool down.
- Chills and shivering: The body may shiver as it attempts to raise its temperature.
- Headache: Fever often comes with a headache.
- Muscle aches: Generalized body aches are common.
- Loss of appetite: Children with fever may eat less than usual.
- Irritability: Increased irritability or fussiness, especially in younger children.
- Fatigue: Feeling more tired or lethargic than usual.
- Dehydration: Signs include dry mouth, sunken eyes, and reduced urine output.
When to seek medical attention
Parents should seek medical attention if their child:
- Is younger than 3 months old with a fever of 100.4°F (38°C) or higher.
- Has a fever of 104°F (40°C) or higher at any age.
- Shows signs of dehydration, persistent vomiting, or a severe headache.
- Has a fever that lasts more than 3 days.
- Experiences a febrile seizure or has difficulty breathing.
- Appears unusually drowsy, unresponsive, or has a stiff neck.
Pediatric Fever Guidelines Template
Pediatric Fever Guidelines Sample
Pediatric Fever Guidelines
Pediatric Fever Guidelines offer structured approaches to evaluate and manage fever in children under three years of age. These guidelines are crucial as fever is a common symptom in children and can sometimes indicate serious health issues.
Younger than one month
A high-risk assessment requires an inpatient evaluation and is recommended for infants younger than one month. This includes blood tests such as CBC with differential, blood culture, PCT, and CRP if available. Urine tests are conducted, including urinalysis and urine culture. A lumbar puncture analyzes CSF components like WBC count, protein, glucose, and culture. Chest radiography is recommended for all neonates, and empiric antibiotics are initiated after cultures have been obtained.
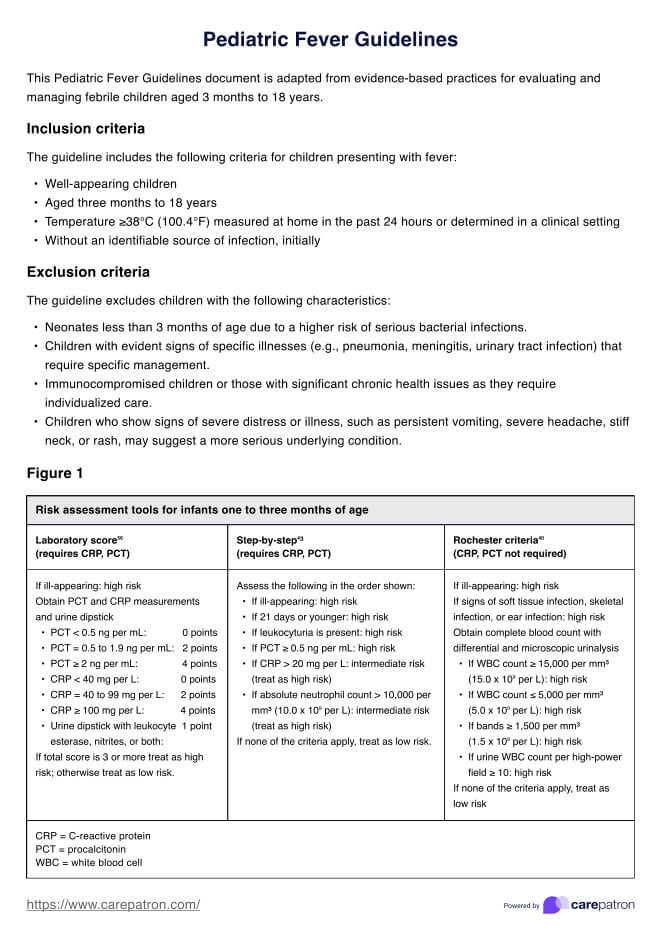
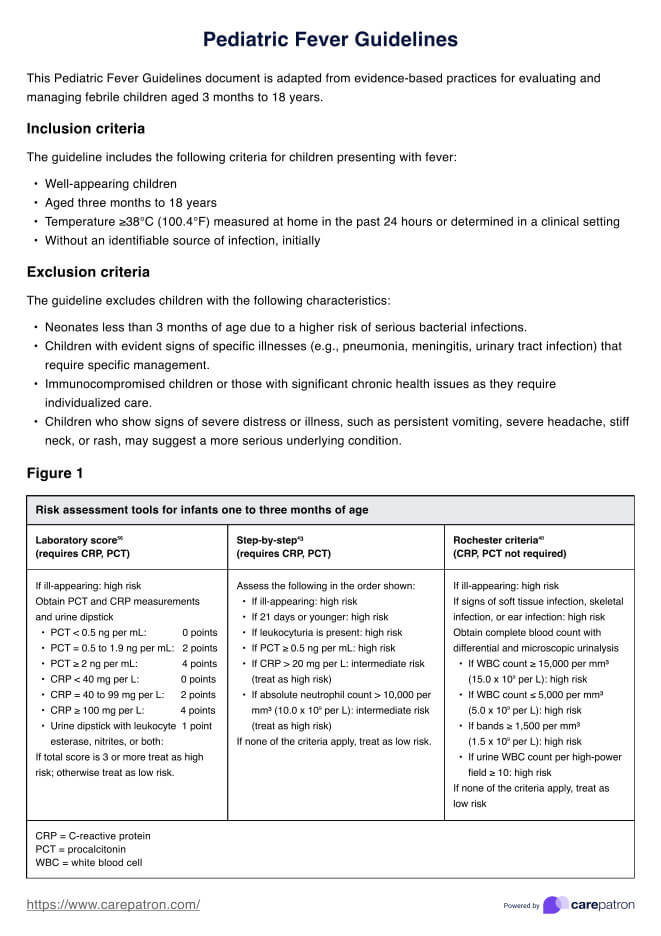
One to three months of age
Management varies for children aged one to three months based on their appearance and test results. This age group undergoes blood and urine tests similar to those of neonates. A lumbar puncture is recommended if the whole child has a fever or appears ill. Based on the specific circumstances and test results, empiric antibiotics may be started after obtaining cultures.
Three months to three years of age
Children within this age bracket are assessed for risk depending on the presence of signs of serious illness. If neurologic or meningeal signs are present, they undergo comprehensive blood and urine tests and a lumbar puncture. Chest radiography is advised if respiratory symptoms suggest pneumonia, and antibiotics are considered based on the specific diagnosis and lab results.
How to use our Pediatric Fever Guidelines handout
The Pediatric Fever Guidelines handout is designed to provide healthcare professionals with a clear and accessible guide for managing febrile conditions in children. Here’s how to effectively utilize this resource:
Step 1: Understand what is included in the handout
The handout includes detailed evaluation and management protocols for febrile children younger than three years, segmented by age groups: younger than one month, one to three months, and three months to three years. Each section details necessary tests such as blood tests, urine tests, lumbar puncture, and when to consider antibiotics.
Step 2: Download a copy of the handout
To download a copy of the Pediatric Fever Guidelines handout, scroll down this article until you see the "Download" button. To view the document, ensure you have PDF reading software installed on your device.
Step 3: Implement the guidelines in clinical practice
Use the handout as a reference tool in clinical settings when assessing and managing fever in children. The step-by-step structure helps make informed decisions based on age-specific risk assessments and clinical signs. Keep the handout accessible in digital format on a device or as a printed copy in your practice area.
Benefits of using this handout
Here are the benefits of using the Pediatric Fever Guidelines handout:
- Enhanced consistency and accuracy: The handout provides standardized procedures and recommendations, ensuring consistent care across different providers. This standardization helps reduce errors and variations in the treatment of pediatric fever.
- Improved diagnostic precision: With detailed guidelines on assessing and interpreting symptoms and fever patterns, healthcare providers can more accurately diagnose the underlying causes of fever in children. This leads to more effective and targeted treatments.
- Efficient communication: The handout is a quick reference tool that facilitates clear and efficient communication among healthcare team members. It ensures that everyone involved in a child's care is on the same page regarding treatment plans and expectations.
- Parental reassurance and education: It can be used to educate parents and caregivers about the significance of fever, proper temperature measurement, and when to seek medical attention. This knowledge can alleviate parental anxiety and promote appropriate care practices at home.
- Evidence-based care: The guidelines are typically based on the latest evidence and best practices, which helps ensure that the care provided is up-to-date and effective, leading to better health outcomes for pediatric patients.
Commonly asked questions
In pediatric guidelines, a fever is typically defined as a rectal temperature of 100.4°F (38°C) or higher, indicating the normal body temperature that is a response to an infection or illness.
To manage a pediatric fever, it's important to monitor the child's fever closely, keep them hydrated, and use age-appropriate antipyretics like acetaminophen or ibuprofen as recommended by healthcare guidelines, ensuring correct dosing based on the child's weight and age.
When children have a fever, precautions should include avoiding over-bundling to prevent overheating, monitoring for signs of serious illness such as difficulty breathing or extreme lethargy, and consulting a healthcare provider if the fever persists for more than 24 hours in a child under 2 or more than 72 hours in older children.