Canadian C Spine Rules
The Canadian C-Spine Rules guide healthcare professionals in assessing neck injuries, reducing unnecessary imaging, and ensuring efficient, evidence-based patient care.


What are cervical spine injuries?
Cervical spine injuries involve the seven vertebrae in the neck. These injuries range from mild strains and sprains to severe dislocations like a cervical spine fracture. Cervical fractures are particularly serious and can significantly impact a person's health and mobility.
Causes
In emergency medicine, cervical fractures often result from blunt trauma due to high-energy incidents such as car accidents, falls from significant heights, sports injuries, or diving accidents. Conditions like osteoporosis, which weakens bones, can also make individuals more susceptible to fractures from minor falls or movements.
Symptoms
Symptoms can vary widely depending on the severity and location of the injury. Common symptoms include severe neck pain, tenderness, and swelling. Affected individuals may experience limited neck motion, muscle weakness, and numbness or tingling in the arms or legs.
In severe cases, cervical fractures can lead to spinal cord injuries, resulting in partial or complete paralysis, difficulty breathing, and loss of bladder or bowel control.
Treatment and management
Prompt medical evaluation and treatment are crucial to prevent further damage and optimize recovery. Treatment may include immobilization with a cervical collar, pain management, physical therapy, and possibly surgical intervention to stabilize the spine and prevent neurological complications.
Canadian C Spine Rules Template
Canadian C Spine Rules Example
What is cervical spine imaging?
Cervical spine imaging refers to techniques used to visualize the structures of the cervical spine, which includes the neck's seven vertebrae. Common methods include X-rays, CT scans, and MRIs.
X-rays provide clear images of the bones, helping detect fractures, dislocations, and degenerative changes like arthritis. CT scans offer more detailed cross-sectional images, which are useful for identifying complex fractures and bone alignment.
MRIs are crucial for evaluating soft tissues such as intervertebral discs, spinal cord, nerves, and ligaments. Unlike X-rays and CT scans, MRIs use magnetic fields and radio waves, making them effective in detecting herniated discs, spinal cord injuries, infections, and tumors.
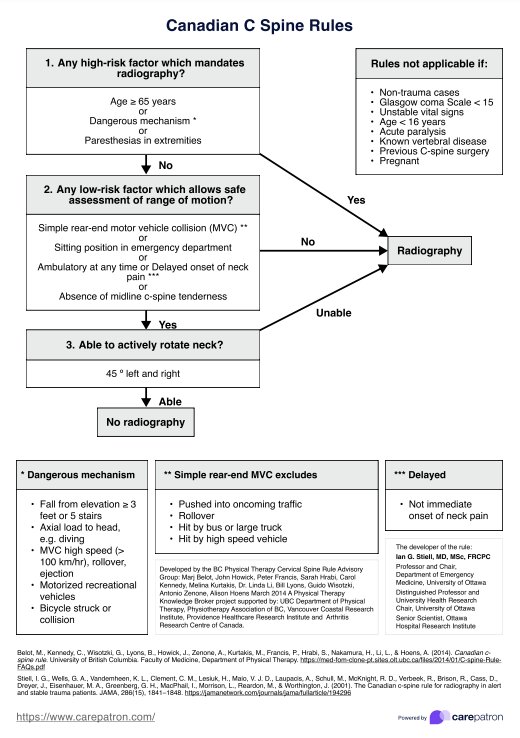
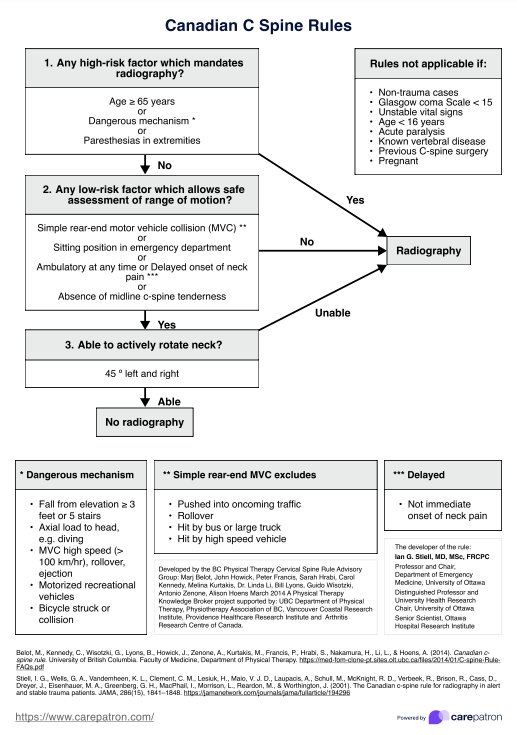
What is the Canadian C Spine Rule?
The Canadian C Spine Rule is specifically designed to assess the need for cervical spine imaging in alert and stable trauma patients who have experienced incidents that could lead to neck injuries. Developed to reduce unnecessary radiography, the rule applies specifically to alert and stable patients who have experienced trauma that could result in a cervical spine injury.
The rule evaluates three main criteria:
- The presence of high-risk factors such as age over 65, dangerous mechanism of injury (e.g., falls from significant heights, high-speed motor vehicle collisions), or paresthesia in the extremities.
- The absence of low-risk factors that allow safe assessment of range of motion, such as a simple rear-end motor vehicle collision, sitting position in the emergency department, ambulatory status, delayed onset of neck pain, or absence of midline cervical spine tenderness.
- The patient’s ability to actively rotate their neck 45 degrees to the left and right.
The Canadian C Spine Rule does not apply to patients with a Glasgow Coma Scale score below 15, those under 16 years old, patients with known vertebral disease, or those with previous cervical spine surgery.
How does our Canadian C Spine Rules template work?
Our Canadian C Spine Rules template guides healthcare providers systematically in determining the necessity of cervical spine imaging for trauma patients. The decision-making process is divided into three parts, each assessing specific criteria.
Step 1: Access the template
First, access the template via the Carepatron app or the download button on this page to help guide you through the decision-making process. You can open it on your device or print a copy of it.
Step 2: Assess high-risk factors
Begin by evaluating the patient for any high-risk factors. Check if the patient's age is above 65, the mechanism of injury was dangerous (e.g., fall from height, high-speed motor vehicle collision), or if there is paresthesia in the extremities.
If any of these high-risk factors are present (answered "Yes"), proceed with cervical spine imaging.
If all answers are "No," move to the next step.
Step 3: Assess low-risk factors
Check for the presence of low-risk factors that may allow for a safe assessment of the neck's range of motion. These include being in a simple rear-end motor vehicle collision, sitting position in the emergency department, being ambulatory at any time, delayed onset of neck pain, and absence of midline cervical spine tenderness.
If any of these low-risk factors are present (answered "Yes"), proceed to the next step.
If all answers are "No," cervical spine imaging is required.
Step 4: Assess neck rotation
Finally, assess whether the patient can actively rotate their neck 45 degrees to the left and right.
If the patient can perform this motion (answered "Yes"), imaging is not required.
If the patient cannot perform this motion (answered "No"), proceed with cervical spine imaging.
Applicability
This rule does not apply to patients under 16 years old, those with a Glasgow Coma Scale score below 15, patients with known vertebral disease, or those with previous cervical spine surgery.
Benefits of using our template
Using our Canadian C Spine Rules template offers several benefits for healthcare providers and patients. It ensures a standardized approach to assessing cervical spine injuries, enhancing diagnostic accuracy and reducing the likelihood of missed injuries. By following clear, evidence-based criteria, clinicians can make informed decisions about the necessity of imaging, avoiding unnecessary radiographic procedures.
The template also promotes efficiency in clinical settings. With its straightforward step-by-step process, healthcare providers can quickly determine the appropriate course of action, saving valuable time. The use of this template can improve patient outcomes by ensuring timely and appropriate intervention for significant cervical spine injuries, leading to better recovery and fewer complications.
Management and treatment of cervical spine injuries
The management and treatment of cervical spine injuries depend on the severity and specific nature of the injury. Initial assessment and stabilization are critical to prevent further damage and complications.
Conservative treatments are typically effective for minor injuries such as strains and sprains. These include rest, immobilization with a cervical collar, physical therapy, and pain management with medications like nonsteroidal anti-inflammatory drugs (NSAIDs).
More severe injuries, such as fractures or dislocations, often require more intensive interventions. Immobilization using a rigid cervical collar or a halo vest is essential to prevent further injury. In some cases, traction may be used to realign the spine. Surgical options, such as spinal fusion or decompression, may be necessary to stabilize the spine, relieve pressure on the spinal cord, or repair damaged vertebrae and discs.
Rehabilitation plays a crucial role in recovery, focusing on restoring function, mobility, and strength. This can include physical therapy, occupational therapy, and pain management strategies. Early and appropriate treatment significantly improves outcomes and reduces the risk of long-term complications for individuals with cervical spine injuries.
Commonly asked questions
The Canadian C Spine Rule includes additional high-risk factors and evaluates the ability to rotate the neck, while Nexus Criteria focuses on the absence of specific clinical findings like tenderness and neurological deficits.
In emergency and clinical settings, the Canadian C Spine Rule can be applied by trained healthcare professionals, including physicians, nurses, and paramedics.
Cervical spine imaging should be avoided in patients who meet low-risk criteria according to clinical decision rules and have no signs of significant injury or neurological deficits.