Diabetic Foot Ulcer Treatment Guidelines
Learn about the latest diabetic foot ulcer treatment and Carepatron's free PDF download with examples of effective treatment plans. Fight diabetes with the right information.


What are diabetic foot ulcers?
Diabetic foot ulcers are open sores or wounds that commonly occur in individuals with insulin dependent diabetes mellitus, particularly those with diabetic neuropathy or vascular complications. These ulcers typically develop on the bottom of the feet or toes and are caused by a combination of factors, including poor circulation, nerve damage, and pressure from shoes or walking.
For diabetic patients, these ulcers pose significant risks due to reduced sensation in the feet and impaired healing. Prompt treatment and prevention of infected diabetic foot ulcers are crucial to avoid complications such as a severe infection, which can lead to more severe diabetic foot problems.
Diabetic Foot Ulcer Treatment Guidelines Template
Diabetic Foot Ulcer Treatment Guidelines Example
Treatment for diabetic foot ulcers
Treating diabetic foot ulcers requires a multifaceted approach to address the various underlying factors and promote wound healing effectively. Here are the primary treatment methods for wound care and ensuring complete wound healing.
Wound care and dressing
Proper wound dressing is essential for managing diabetic foot ulcers. This involves cleaning the wound, removing dead or infected tissue, and applying appropriate wound dressings to protect the moist wound environment and promote healing. Regular monitoring and changing of dressings are crucial to prevent diabetic foot infections and promote wound healing.
Offloading pressure
Reducing pressure on the foot ulcer is vital for recovery. This can be achieved using special footwear, braces, or orthotic devices that redistribute weight and alleviate stress on the affected area. In some cases, patients may need to use crutches or a wheelchair to keep weight off the ulcer.
Surgical interventions
Surgical treatments may be necessary for severe or non-healing diabetic ulcers. Procedures such as debridement, which involves removing dead or necrotic tissue, can help promote wound healing. Achilles tendon lengthening is another surgical option that can relieve pressure on the foot, aiding in the treatment of diabetic foot complications. In other cases, a vascular surgeon may perform procedures to improve blood flow and enhance healing.
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy involves breathing pure oxygen in a pressurized chamber, which can enhance the body's natural healing processes. This treatment can be particularly effective for infected wounds and diabetic foot infections, as it increases oxygen supply to the damaged tissues and promotes faster recovery.
Growth factors and advanced therapies
Using growth factors and other advanced therapies can accelerate the healing of foot wounds. These treatments stimulate the body's repair mechanisms and can be especially beneficial for chronic or non-healing ulcers. Combining these therapies with other treatment modalities can lead to improved outcomes.
Managing peripheral arterial disease and venous leg ulcers
Peripheral vascular disease and venous leg ulcers are common conditions associated with diabetic foot disorders. Addressing these conditions is crucial for successful foot ulcer treatment. Vascular interventions, medication, and lifestyle modifications can improve blood flow and support overall healing.
Effective treatment of diabetic foot ulcers requires a collaborative effort among healthcare professionals, including foot ulceration surgeons, vascular surgeons, and wound care specialists.
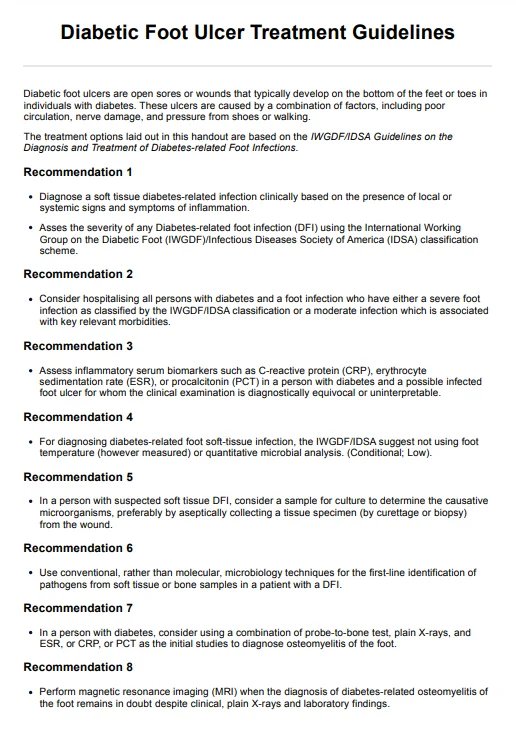
How to use our treatment guidelines handout
Using Carepatron's treatment clinical practice guideline handout can help healthcare professionals, like foot and ankle surgeons, manage diabetic foot ulcers more effectively. This comprehensive resource offers evidence-based options from the IWGDF/IDSA Guidelines on the Diagnosis and Treatment of Diabetes-related Foot Infections.
Access and download the handout
First, access the treatment guidelines handout template on this page. Download the document to ensure you have the most up-to-date version, which reflects the latest clinical practice guidelines for managing diabetic wounds and preventing foot ulcers.
Introduce the handout to the patient
During consultations, introduce the handout to your patients with diabetic foot ulcers. Highlight sections that are particularly relevant to the patient's affected foot, such as treatments for chronic wounds and antibiotic therapy for infected bone and surrounding skin.
Educate the patient about treatment options
Discuss preventive measures for foot ulcers, such as proper footwear and daily foot inspections. Educate them on wound repair techniques, the significance of maintaining a moist wound bed, and the potential use of skin grafts for severe cases.
How can healthcare professionals benefit from our template?
Healthcare professionals can greatly benefit from Carepatron's Diabetic Foot Ulcer Treatment Handout template. This comprehensive tool streamlines the treatment process by providing clear, evidence-based guidelines that enhance the consistency and quality of patient care.
Practitioners can efficiently identify and address diabetic foot wounds, implement appropriate dressing of wound techniques, and monitor for potential complications such as diabetic foot infections and chronic wounds. The template also facilitates patient education, helping individuals understand their condition and the necessary steps for healing and prevention.
Commonly asked questions
The healing time for a diabetic foot ulcer can vary widely, typically ranging from a few weeks to several months, depending on factors such as the severity of the ulcer, patient compliance with treatment, and underlying health conditions. Proper wound care, pressure offloading, and diabetes management are crucial to expedite healing.
There is no single "best" ointment for diabetic foot ulcers, as treatment should be tailored to the individual patient's needs. However, antimicrobial ointments and those promoting moisture balance are commonly recommended to prevent infection and aid healing.
The 5 P's of diabetic foot ulcer prevention are: Proper footwear, Protecting feet from injury, Performing regular foot inspections, Promoting good blood flow, and Promptly addressing any foot issues.