ICU Mobility Scale
Check the highest mobility level of your patient in the intensive care unit with the ICU Mobility Scale.


What is the ICU Mobility Scale (IMS)?
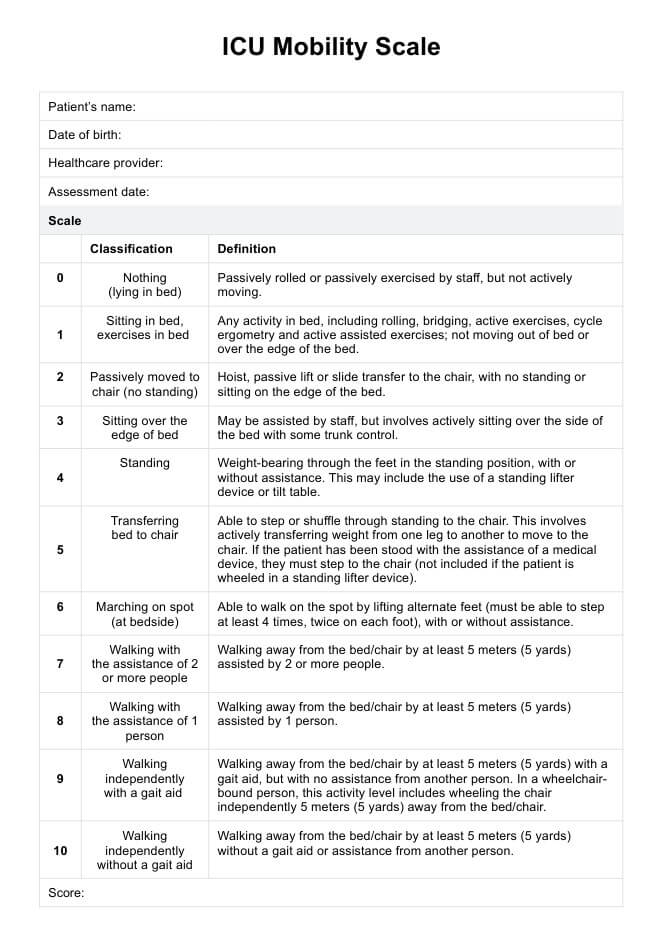
The ICU Mobility Scale is an 11-item categorical scale designed to measure the highest level of functional mobility patients achieve in the intensive care units (ICU). It is a critical tool for healthcare professionals, providing a standardized method to assess and monitor the mobility and functional abilities of critically ill patients and patients with ICU-acquired weakness, including those with acute respiratory failure and mechanically ventilated patients.
The IMS delineates various patient activity levels, ranging from Level 0 (complete inactivity) to Level 10 (independent ambulation). Each level is precisely defined, offering a clear framework for evaluating patient progress:
- Level 0: Nothing (lying in bed): The patient remains passively in bed with any movement, including passive rolling or exercises, facilitated by the staff.
- Level 1: Sitting in bed, exercises in bed: The patient engages in any bed-based activity, including physical therapy exercises. However, the patient does not move out of or over the edge of the bed.
- Level 2: Passively moved to chair (not standing): The patient is transferred to the chair through housing, passive lifting, or slide transfers.
- Level 3: Sitting over the edge of the bed: The patient actively sits on the side of the bed with some degree of trunk control. possibly with assistance from the staff.
- Level 4: Standing: The patient bears weight through the feet in a standing position with or without assistance.
- Level 5: Transferring bed to chair: The patient actively transfers from the bed to a chair, stepping or shuffling through standing and shifting weight from one leg to another.
- Level 6: Marching on the spot (at bedside): The patient performs on-the-spot marching by lifting alternate feet at least four times (twice per foot), with or without assistance.
- Level 7: Walking with assistance of 2 or more people - The patient walks at least 5 meters away from the bed or chair, assisted by two or more individuals.
- Level 8: Walking with assistance of 1 person - The patient walks at least 5 meters away from the bed or chair, assisted by one person.
- Level 9: Walking independently with a gait aid - The patient walks at least 5 meters away from the bed or chair using a gait aid, but without assistance from another person. This level also includes wheelchair-bound patients who wheel themselves independently.
- Level 10: Walking independently without a gait aid - The patient walks at least 5 meters away from the bed or chair without a gait aid or any assistance.
The IMS is essential in managing ICU patients by enabling precise and consistent mobility assessment. Categorizing patients’ functional abilities aids in tailoring individualized rehabilitation plans, facilitates progress monitoring, and ultimately contributes to improved patient outcomes during their stay in the intensive care unit.
ICU Mobility Scale
ICU Mobility Scale
How does our ICU Mobility Scale template work?
The ICU Mobility Scale (IMS) template is designed to systematically assess and document the highest level of functional mobility achieved by patients in the ICU. Once you’ve accessed a copy of the ICU Mobility Scale PDF, follow this step-by-step guide to ensure accurate and consistent use of the template:
Step 1: Patient preparation
Firstly, the patient should be informed about the purpose of the assessment and what it will entail, such as physical and occupational therapy exercises. Afterward, verify that the patient's medical condition is stable, all necessary medical equipment is secure, and there are no contraindications for mobilization.
Step 2: Initial assessment
Review the patient's medical history, condition, and previous mobility assessments. Observe the patient in their current state without intervention to establish a baseline level of mobility.
Step 3: Mobility assessment
Begin the assessment at Level 0 of IMS and progress to each scale level sequentially. Assess the patient's ability to perform the activities described at each level.
Step 4: Documentation
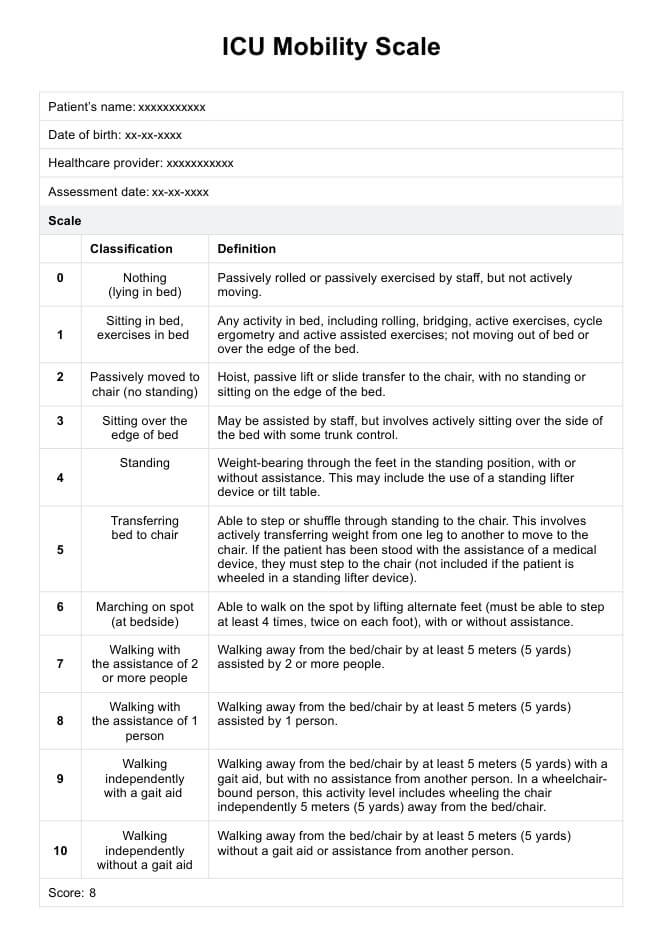
On the ICU Mobility Scale template, document the following:
- Highest level of mobility the patient achieved during the assessment
- Assistance provided or devices used
- Relevant observations like the patient's endurance, balance, and any difficulties encountered
- Date, time, and the name of the assessing healthcare professional
Step 5: Plan and reassess
Based on the assessment, create a tailored mobility plan that aligns with the patient's current capabilities and short-term and long-term recovery goals. Remember to conduct regular reassessments using the IMS template and update the document to use it to monitor progress, adjust the mobility plan as necessary, and maintain an accurate patient mobility status record.
Scoring of the ICU Mobility Scale
The scoring and interpretation of the ICU Mobility Scale are pretty straightforward. Healthcare professionals assess and score a patient's mobility based on their capabilities. For instance, a patient who can sit on the edge of the bed scores a 3, while one can walk with assistance from one person scores an 8.
This scoring system facilitates the monitoring of patient progress during their ICU stay and aids in predicting critical outcomes, such as survival rates, hospital discharge, and hospital mortality.
Next steps
After conducting the ICU Mobility Scale, healthcare professionals should screen patients for eligibility for early mobility interventions, such as early physical therapy treatments and occupational therapy, based on their IMS results. In addition, providers must follow an early mobility guideline that outlines appropriate interventions and assists patients with mobility activities that align with their assessed level.
They must also evaluate and learn from their implementation process periodically, measure performance metrics, and adapt as necessary to improve outcomes. By incorporating these new signs and evolving best practices, they further refine and enhance their early mobility protocol.
Doing these two faithfully should ensure enhanced patient care, improve mobility outcomes, and improve patients' quality of life.
Commonly asked questions
Early mobilization is when physical activity is applied or incorporated after the start of critical illness/injury as early as the 2nd day.
Early mobility, especially its programs, shortens the stay at the ICU and the hospital.
One can mobilize patients in the ICU through activities such as bedside sitting, active side-to-side turning, host therapy, and exercising in the bed to name a few.