CRIES Pain Scale
Download the CRIES Pain Scale PDF to assess pain levels in a postoperative newborn child and determine the next steps.


What is the CRIES Pain Scale?
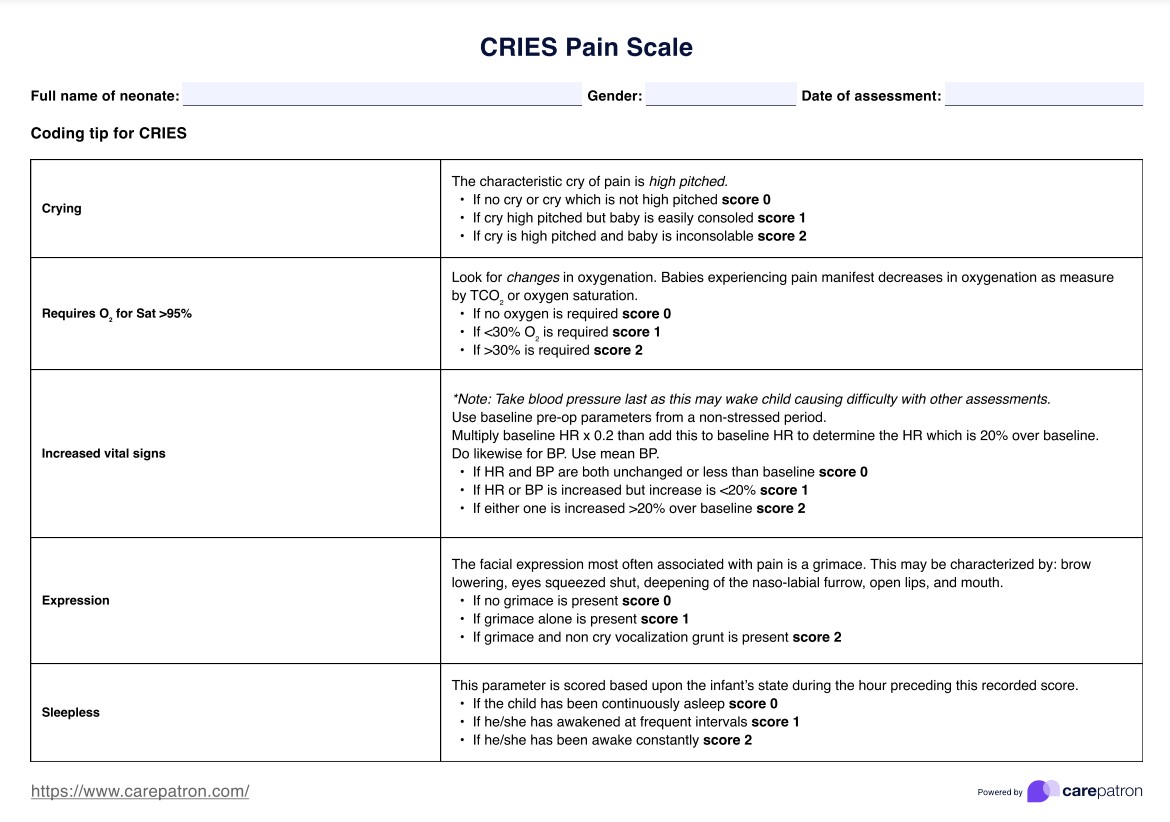
The CRIES Pain Scale is a valuable tool doctors use for neonatal postoperative pain measurement. CRIES stands for crying, requires oxygen, increased vital signs, expression, and sleeplessness). Developed to address the unique challenges of pain assessment in the neonatal population, the CRIES scale incorporates both physiological and behavioral indicators. It was first introduced by Krechel and Bildner in 1995 and has since been validated as a reliable method for assessing neonatal postoperative pain level (Krechel & Bildner, 1995).
Given that newborns and infants cannot express themselves through speech, they typically show that they are in pain and experiencing discomfort through facial expressions and crying. The CRIES Pain Scale is then used to put a number on the level of pain that the child is feeling by looking at how they cry, what their facial expressions are like, what their vital signs are like, and if they can sleep.
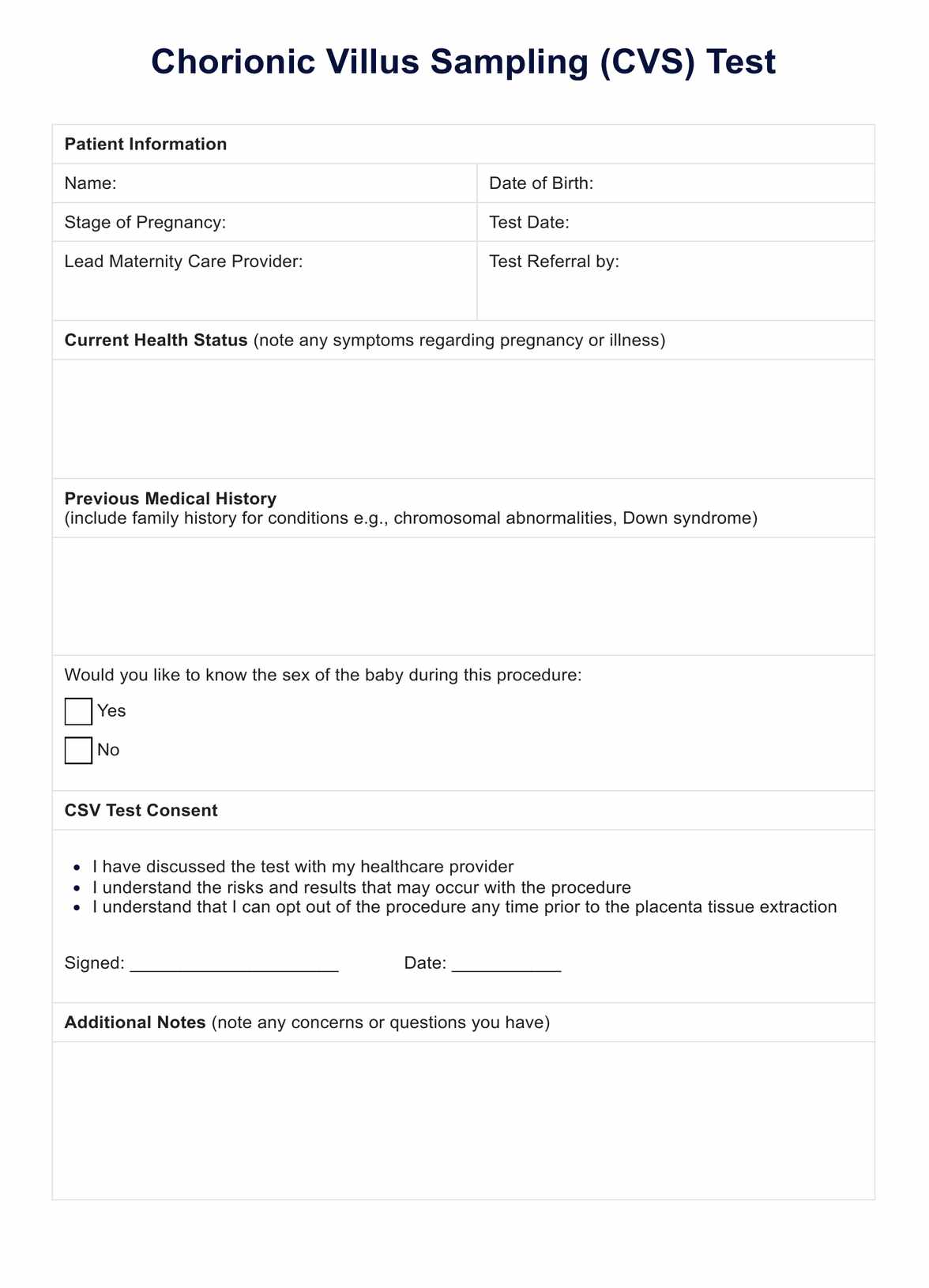
CRIES Pain Scale Template
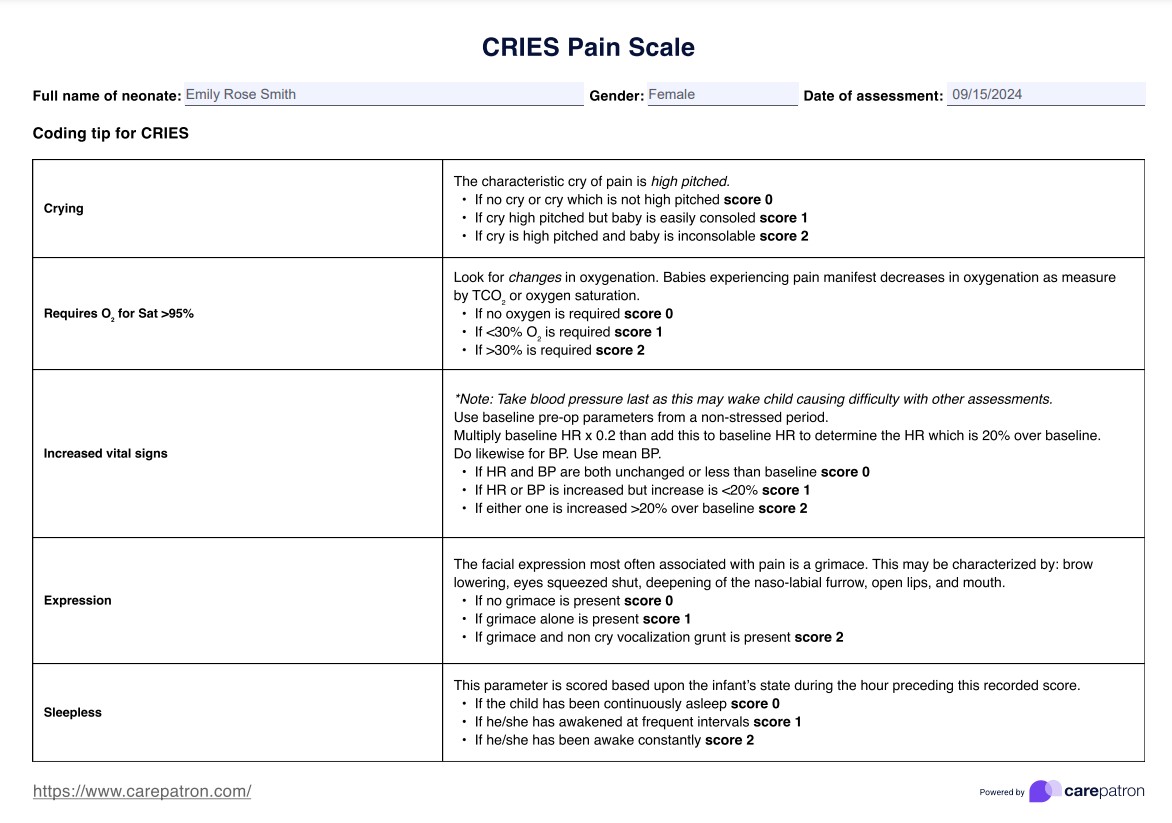
CRIES Pain Scale Example
How to use the CRIES Pain Scale
The CRIES Pain Scale is a valuable tool for determining postoperative pain measurement score in neonates. Here's a step-by-step guide on how to use this CRIES assessment tool in practice.
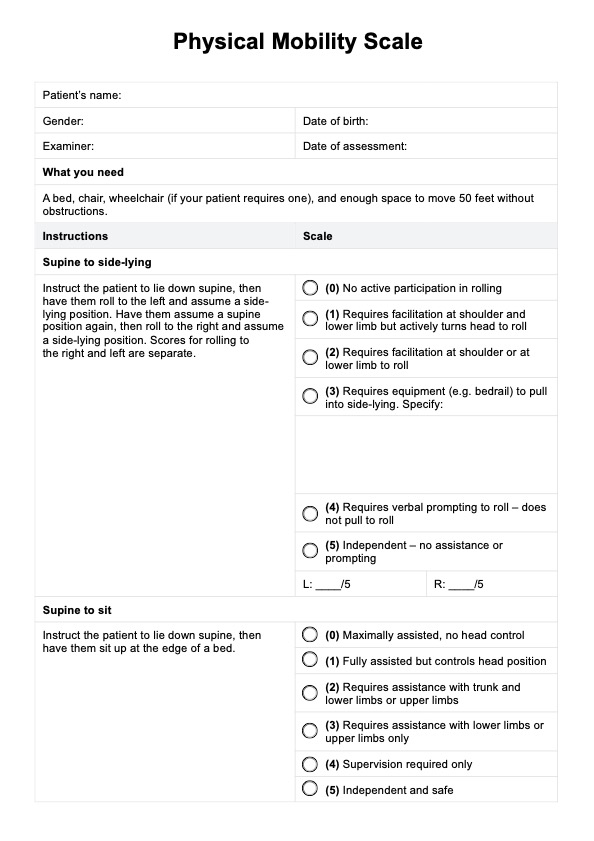
Step 1: Assess the five parameters
Evaluate the neonate for crying, requires oxygen for saturation >95%, increased vital signs, expression, and sleeplessness. Each parameter is scored from 0 to 2 based on specific criteria outlined in the scale.
Step 2: Record scores
Document the score for each parameter at regular intervals or as needed. This allows for tracking pain levels over time and evaluating the effectiveness of interventions.
Step 3: Calculate total score
Sum up the scores from all five parameters. The total score ranges from 0 to 10, with higher scores indicating greater pain intensity.
Step 4: Interpret and plan
Conduct a further pain assessment if the total score is 4 or higher. For scores of 6 or higher, analgesic administration is indicated. You can also adjust pain management strategies based on the scores, the results of multiple pain assessment tools, and your clinical judgment.
Scoring and interpreting the CRIES scale
The CRIES pain assessment is a helpful tool for assessing postoperative pain in neonates born at or after 38 weeks of gestation. Understanding how to score and interpret this scale is crucial for effective pain management in these vulnerable patients.
Each of the five parameters (Crying, Requires oxygen, Increased vital signs, Expression, and Sleeplessness) is scored from 0 to 2, with specific criteria for each score level. The scores for all five parameters are then summed to give a total score ranging from 0 to a maximum score of 10.
It's important to note that a score of 4 or higher should prompt a more thorough pain assessment. This might involve observing the infant for longer periods, consulting with colleagues, or considering other factors influencing the infant's behavior or physiological state.
Analgesic administration is typically indicated for scores of 6 or higher. The choice of analgesic and its dosage should be based on the infant's specific needs, medical history, and the type of surgery performed.
When is it best to use the CRIES Pain Scale?
Since this is primarily for postoperative neonates, it's best to use it as soon as they start to express discomfort through crying or facial expressions so that they can be treated accordingly and immediately.
While this is meant for newborns, it can also be used for infants undergoing operational procedures. You can assess postsurgical pain in neonates and determine the kind of care to give them to relieve their pain.
What are the benefits of using the CRIES Pain Scale?
Speaking of benefits, here are some reasons you should include this assessment for your neonatal-related work:
It's a good tool that helps practitioners gauge neonates and infants.
Since newborns and infants can't speak to convey their feelings of pain and discomfort, the CRIES instrument sets the parameters for practitioners to assess a newborn or infant's pain.
It can help shape what goes into a pain management plan for the child.
Once you have completed the sheet, you should be able to determine what you need to include in the care plan. This will allow you to facilitate the intervention and actionable steps needed to curb the newborn or infant's pain and ensure it does not worsen under your care.
It can be used to monitor the child's pain over time.
Even if you have implemented a pain management plan for newborns or infants, it does not mean they will not experience pain or discomfort again while under your care. So, reusing this pain scale is a good way to monitor them for any signs of pain and discomfort.
It can also be used to determine if your pain management plan needs tweaking.
To jump off the point that using the scale is a good way to monitor the child over time, reusing it should also help you see if your pain management plan is working. If they still experience pain after implementing a pain management plan, adjustments may be needed.
Reference
Krechel, S. W., & Bildner, J. (1995). CRIES: a new neonatal postoperative pain measurement score: Initial testing of validity and reliability. Pediatric Anesthesia, 5(1), 53–61. https://doi.org/10.1111/j.1460-9592.1995.tb00242.x
Commonly asked questions
Each of the five items is scored from 0 to 2, with the total score ranging from 0 to 10. Higher scores indicate more severe pain.
The CRIES Pain Scale should be used regularly to assess and monitor infants' pain, particularly after painful procedures or during ongoing pain management.
The CRIES Pain Scale relies on observable behaviors, which may be influenced by factors such as gestational age, temperament, and underlying medical conditions.















-template.jpg)