Vagus nerve damage can be identified by symptoms like gastrointestinal issues, difficulty swallowing, breathing irregularities, irregular heart rate, voice changes, mood swings, and episodes of fainting or dizziness, often linked to dysfunction in the parasympathetic nervous system and autonomic nervous system.
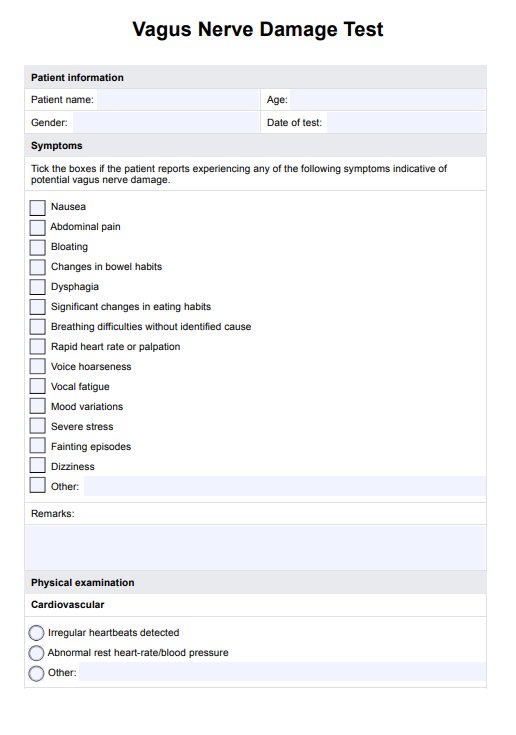
Vagus Nerve Damage Test
Explore how to conduct a vagus nerve damage test and learn how to document the results and your insights.
Vagus Nerve Damage Test Template
Commonly asked questions
Signs of vagus nerve damage include gastroparesis, rapid heart rate, low blood pressure, irregular electrical activity in the heart, difficulty swallowing, and voice alterations, which affect bodily functions controlled by the vagus nerve branches.
If you experience heart palpitations, breathing difficulties, digestive issues like bloating, or changes in voice and swallowing, these could be signs of vagal nerve dysfunction or vagus nerve damage affecting the gastrointestinal tract and cardiovascular system.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











