Headache Charts
Access a comprehensive Headache Chart to understand headache types, locations, and meanings. Download your free PDF here.


What is a Headache Chart?
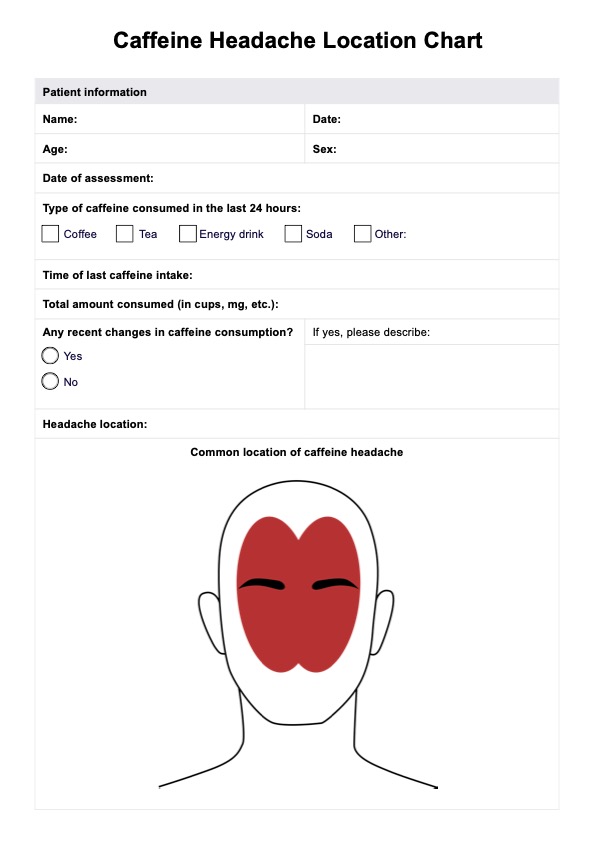
A Headache Chart, also known as a headache diary, headache map, types of headaches diagram, or headache log, is a valuable tool for tracking the patterns, triggers, and symptoms associated with headaches over time. This comprehensive approach helps individuals experiencing headaches, and healthcare providers understand the frequency, duration, intensity, and potential causes of headache episodes.
Maintaining an accurate and detailed Headache Chart allows patients to participate actively in their care by allowing them to easily discuss their symptoms. It also provides healthcare practitioners with valuable information to develop and detect patterns, identify potential triggers, monitor the headache's frequency and severity, and monitor the effectiveness of interventions.
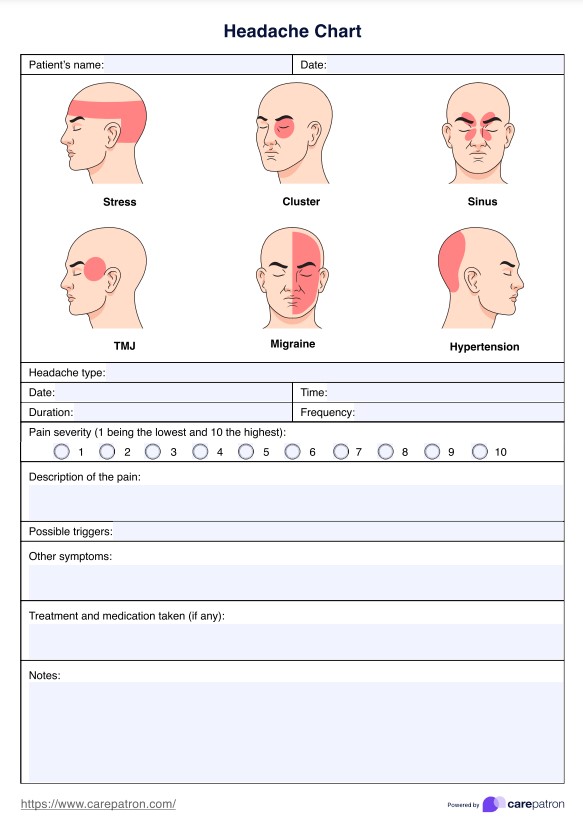
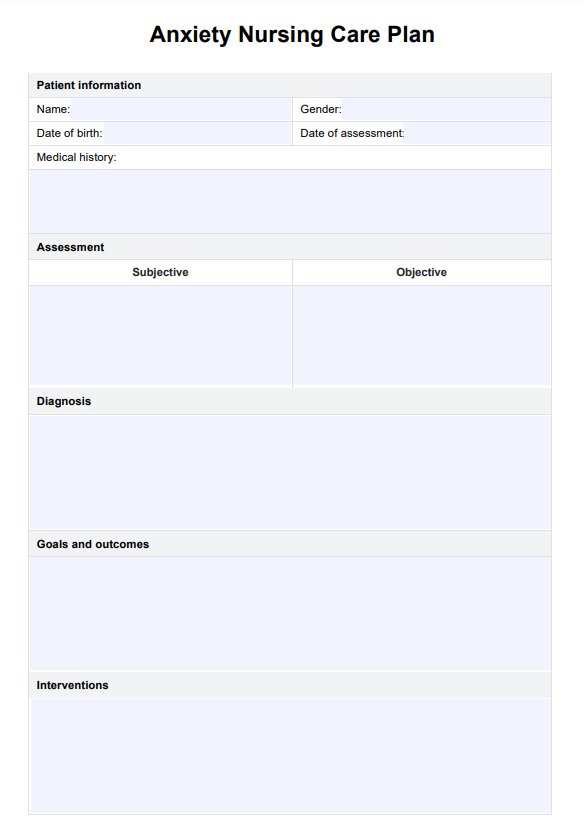
Headache Charts Template
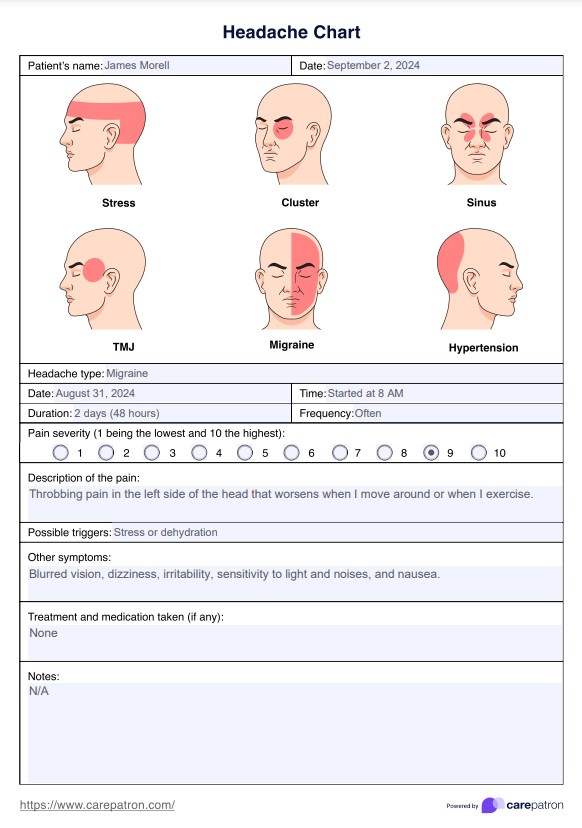
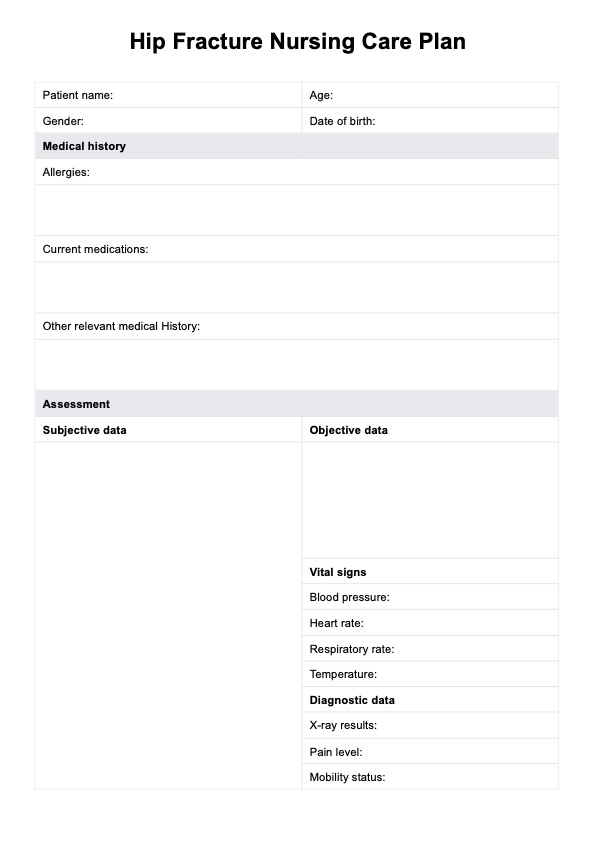
Headache Charts Example
How to use a Headache Chart
A Headache Chart is a useful tool for tracking how often headaches occur, identifying triggers, and helping healthcare providers diagnose and treat headaches effectively. Here’s a step-by-step guide on how to use a Headache Chart:
Step 1: Fill out the initial information
Once you have a copy of the headache location chart, aside from filling out the patient's information, also note down the different details you must know before finalizing the type of headache a patient may have like the date and time, duration, frequency, pain intensity, type of pain, pain location, possible triggers, main headache symptoms, and other symptoms. It may also help if you record any medication the patient took or at-home treatment that the patient tried and its corresponding effectiveness.
Step 2: Review and analyze
Review the chart of headaches to identify the headache type based on the information you obtained. At this point it's best to also interview the patient to ask for any additional details that might be relevant such as the patient's mood, menstrual cycle, or significant events. If a single, completed headache meaning chart isn't enough for a diagnosis or formulation of treatment, you can provide your patient with multiple copies of the template to fill out when they get a headache.
Step 3: Store and update regularly
Even after you've provided treatment or relieved the patient's headache pain, it's best to store and update the headaches chart for accurate tracking and assessing whether the intervention or treatment is effective.
What are the different types of headaches?
Headaches are a common and often debilitating condition that affects people of all ages and backgrounds. They can range from mild and occasional to severe and chronic, significantly impacting an individual's quality of life. Understanding the different types of headache disorders, their causes, and effective management strategies is crucial for healthcare practitioners to provide comprehensive patient care.
Tension headache
Tension headaches are the most prevalent form of primary headache, characterized by a dull, non-pulsating pain that often feels like a tight band around the head. A tension-type headache is typically caused by stress, poor posture, neck, shoulders, and scalp muscle tension or condition, triggering a sudden increase in blood pressure and rapid expansion of blood vessels, resulting in dull, non-pulsating pain.
Migraines
Migraine headaches are a severe form of primary headache disorder characterized by throbbing pain, typically on one side of the head. A migraine headache is often accompanied by nausea, vomiting, and sensitivity to light and sound triggered by various factors like hormonal changes, stress, and certain foods.
Cluster headache
A cluster headache is relatively rare but excruciatingly painful and occurs in cyclical patterns or "clusters." It is characterized by intense, severe pain typically concentrated around one eye or temple and is often accompanied by additional symptoms such as tearing, nasal congestion, and facial flushing.
Sinus headache
Sinus headaches are caused by inflammation and congestion in the sinus cavities. Pain and pressure are usually felt around the eyes, cheeks, and forehead. They are often associated with a sinus infection or allergies and may be accompanied by nasal discharge or fever. Sometimes, nasal polyps (benign growths in the nasal passages) can contribute to sinus headaches and related symptoms.
Medication overuse headache
A medication overuse headache, or rebound headache, is a chronic daily headache that can result from the overuse of pain relief medications, including over-the-counter drugs like ibuprofen and acetaminophen.
Secondary headache
An underlying medical condition or injury, such as head or neck trauma, brain tumors, stroke, or infectious diseases like meningitis, causes secondary headaches. These headaches may have distinct features and require prompt medical attention to address the underlying cause.
Thunderclap headache
While most headaches are not life-threatening, intensely painful headaches, often described as the "worst headache of one's life," may indicate a serious underlying condition. This type of severe headache, known as thunderclap headaches, requires immediate medical attention to rule out potentially dangerous causes, such as subarachnoid hemorrhage or cerebral venous sinus thrombosis.
Occipital neuralgia and cervicogenic headaches
Occipital neuralgia is a condition characterized by intense, shooting, or electric-shock-like pain that originates from the occipital nerves, which run from the base of the skull to the shoulder muscles. The pain is often described as sharp, jabbing, burning, or piercing pain and can radiate from the back of the head to the neck, shoulders, or behind the eyes.
A cervicogenic headache, on the other hand, originates from disorders or injuries in the cervical spine (neck) region. These headaches can cause unilateral (one-sided) pain radiating from the neck to the back of the head, forehead, or around the eye. Cervicogenic headaches are often accompanied by stiff neck or tenderness in the neck muscles.
Commonly asked questions
Headaches can provide clues about their type based on their location. For instance, tension headaches often cause tightness around the forehead or sides of the head, while migraines typically involve throbbing pain on one side. Cluster headaches are characterized by severe pain around one eye, and sinus headaches usually cause pressure around the forehead, nose, and eyes.
Identifying your headache involves paying attention to symptoms and location. Tension headaches may present as a constant ache in the back of the head with muscle stiffness. At the same time, a migraine episode often involves throbbing pain on one side, nausea, and sensitivity to light and sound. Consulting a healthcare professional for a detailed evaluation and diagnosis is essential for appropriate treatment.
The four most common types of headaches are tension, migraines, cluster, and sinus. Understanding these common headache types based on their symptoms and locations can aid in proper diagnosis and management.