Nursing Skin Assessment Checklist
Download a free Nursing Skin Assessment Checklist for accurate skin health evaluation. Get the PDF template and example here.



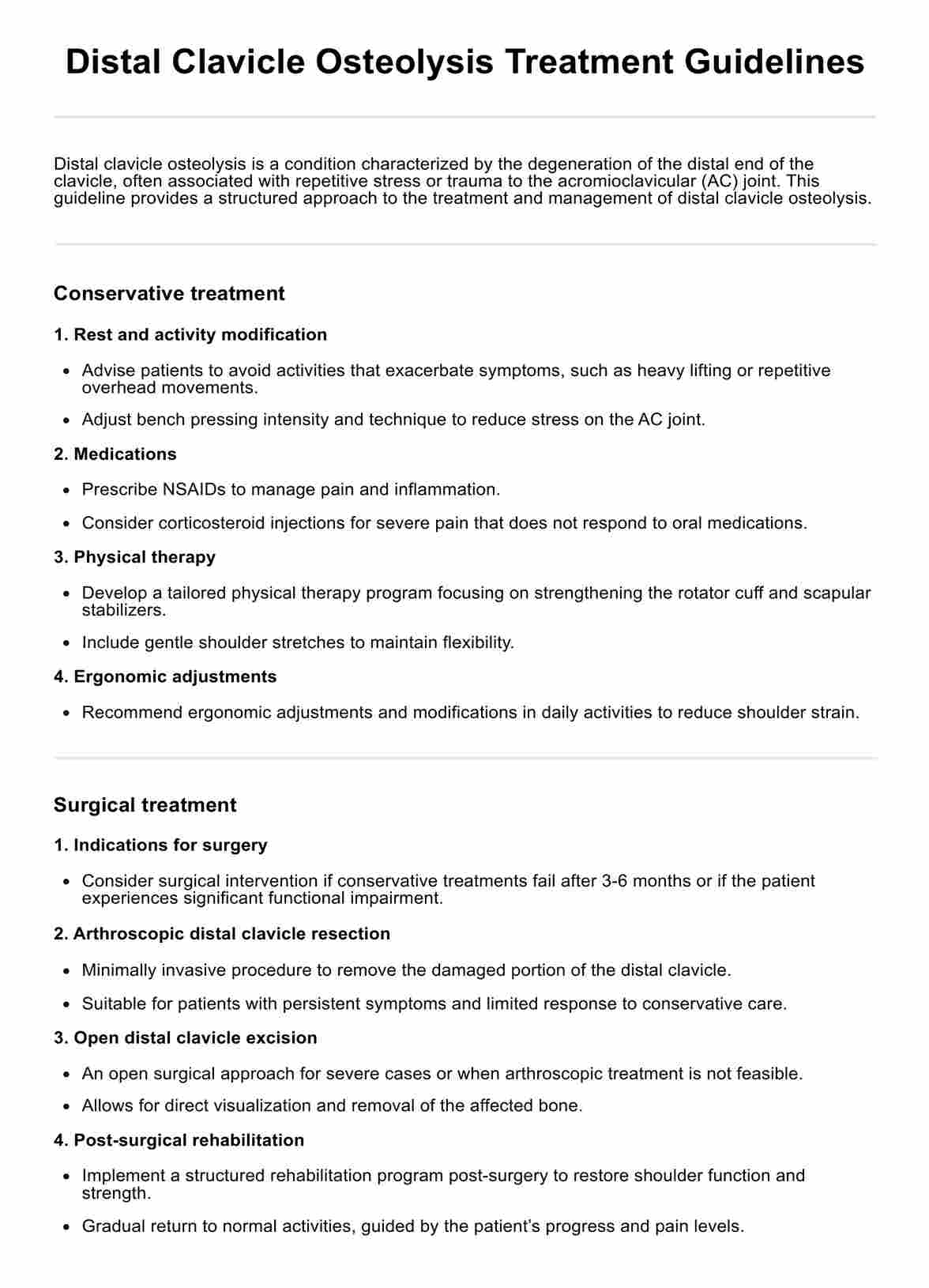
Understanding the skin and its functions
The skin is the largest organ of the human body and is an essential part of our immune system. It covers and protects everything inside our body, including muscles, bones, and organs. The skin not only acts as a barrier against external threats (Cleveland Clinic, n.d.) but is also crucial in regulating body temperature, sensation, and vitamin D synthesis.
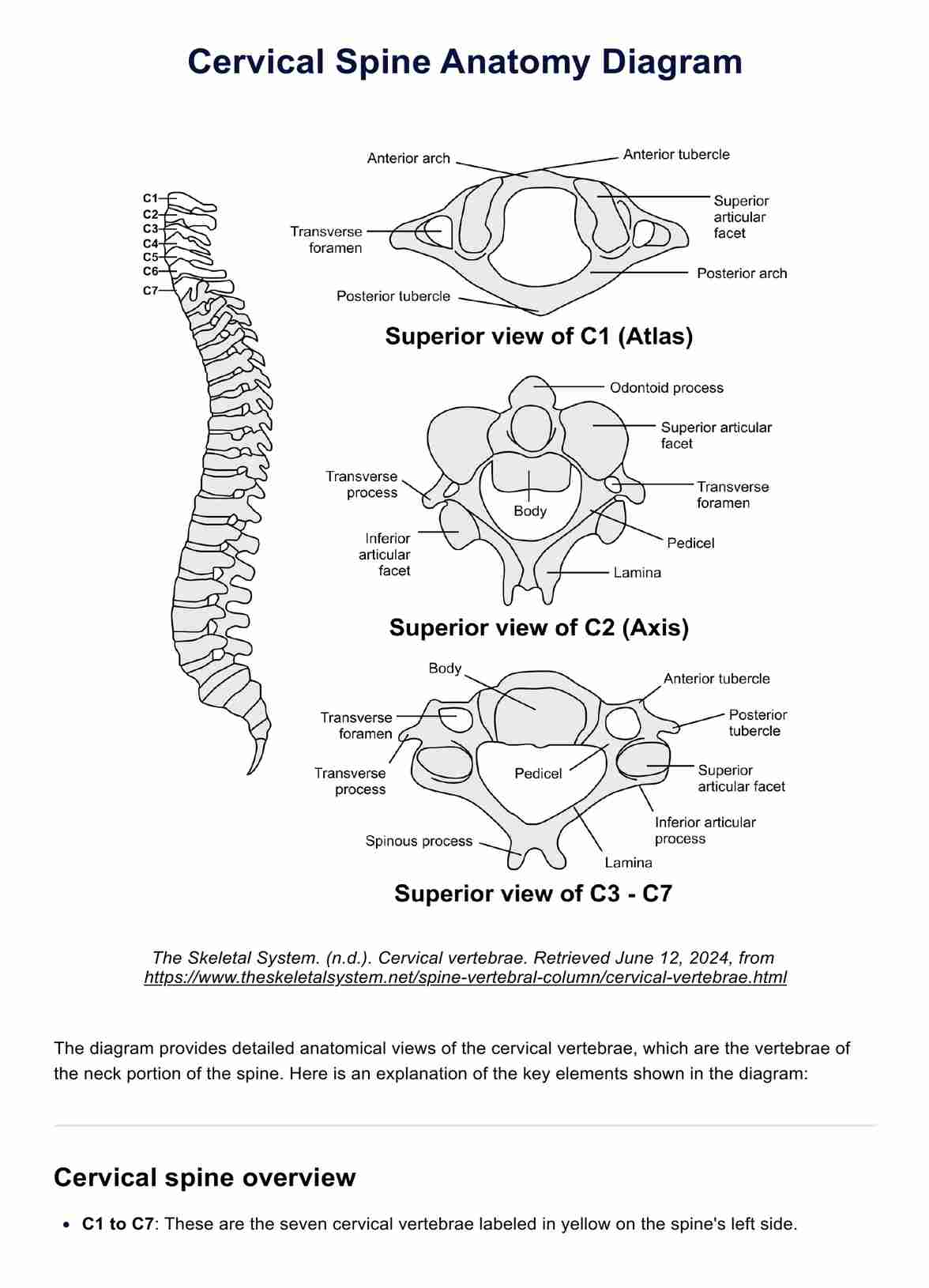
The skin comprises three layers: the epidermis, dermis, and hypodermis (Yousef, Alhajj, & Sharma, 2022). Each layer has its specific functions and is composed of different types of cells:
Epidermis
The epidermis is the outermost layer of the skin and acts as a protective barrier against environmental factors such as bacteria, UV radiation, and chemicals. It consists of five sublayers: stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale.
Dermis
The dermis is the middle layer of the skin and contains blood vessels, nerve endings, hair follicles, sweat glands, and sebaceous glands. It provides structural support to the skin and helps maintain its elasticity and strength.
Hypodermis
The hypodermis is the innermost layer of the skin and primarily consists of fat cells, connective tissue, and blood vessels. It acts as an insulator by regulating body temperature and provides padding to protect internal structures from external trauma.
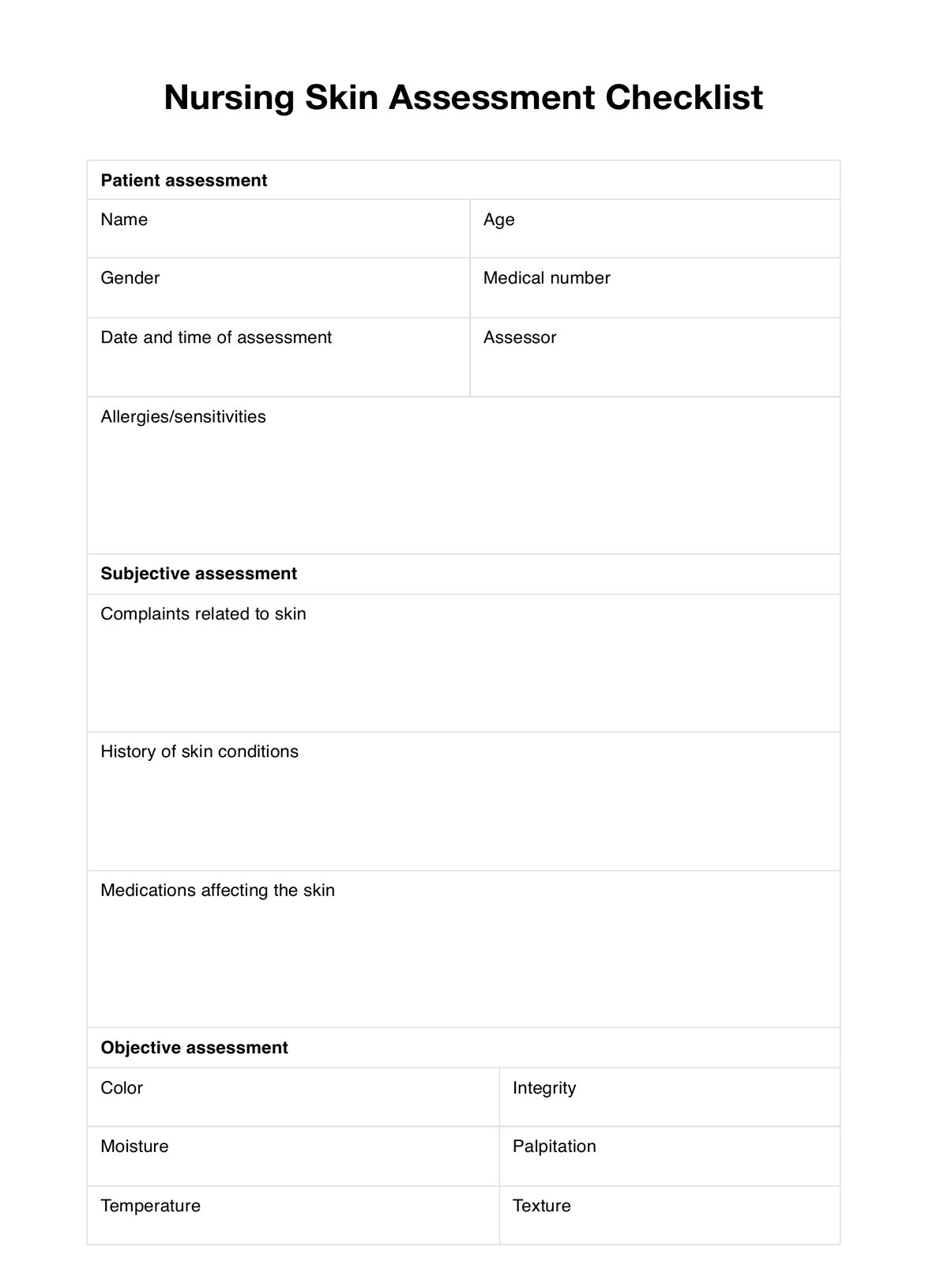
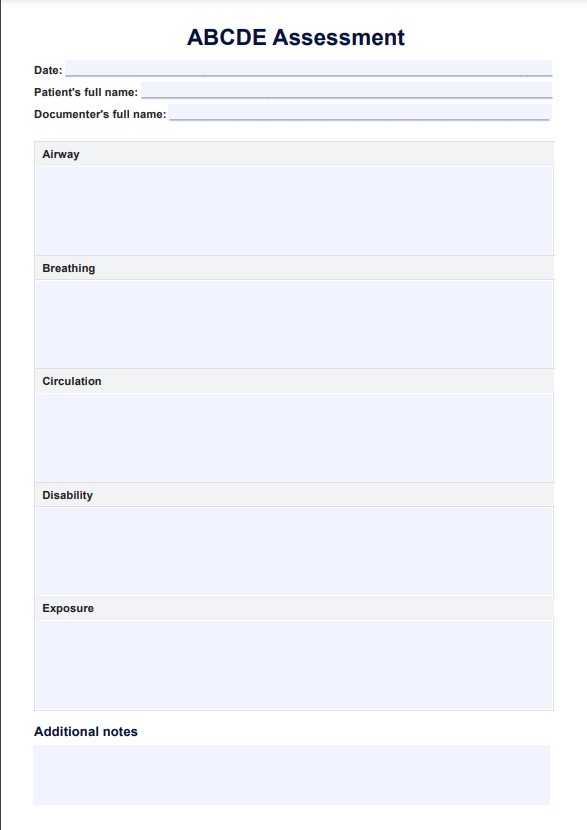
PDF Template
Download PDF TemplateExample PDF
Download Example PDFPrintable Nursing Skin Assessment Checklist
Download this Nursing Skin Assessment Checklist for skin health evaluation.
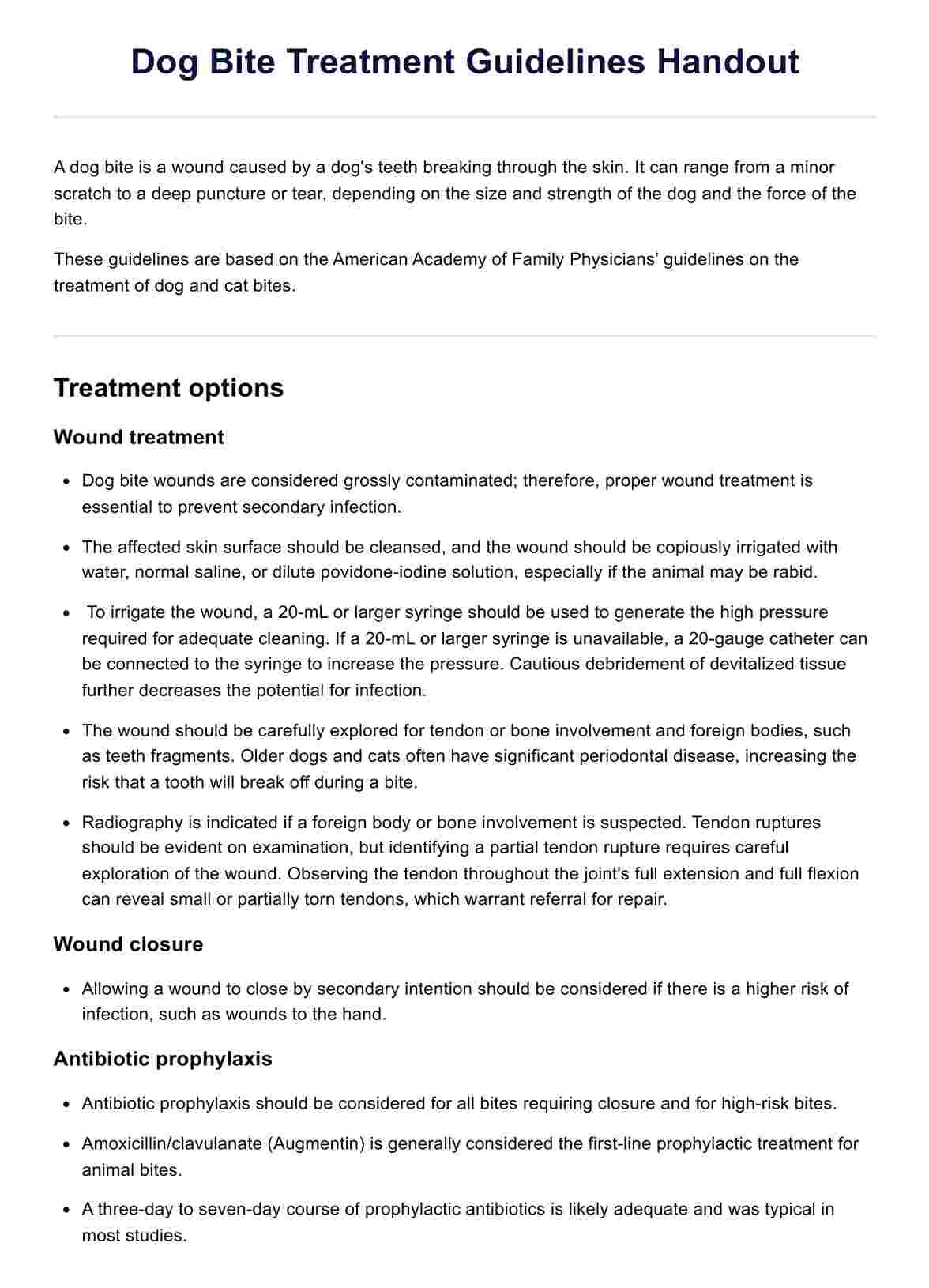
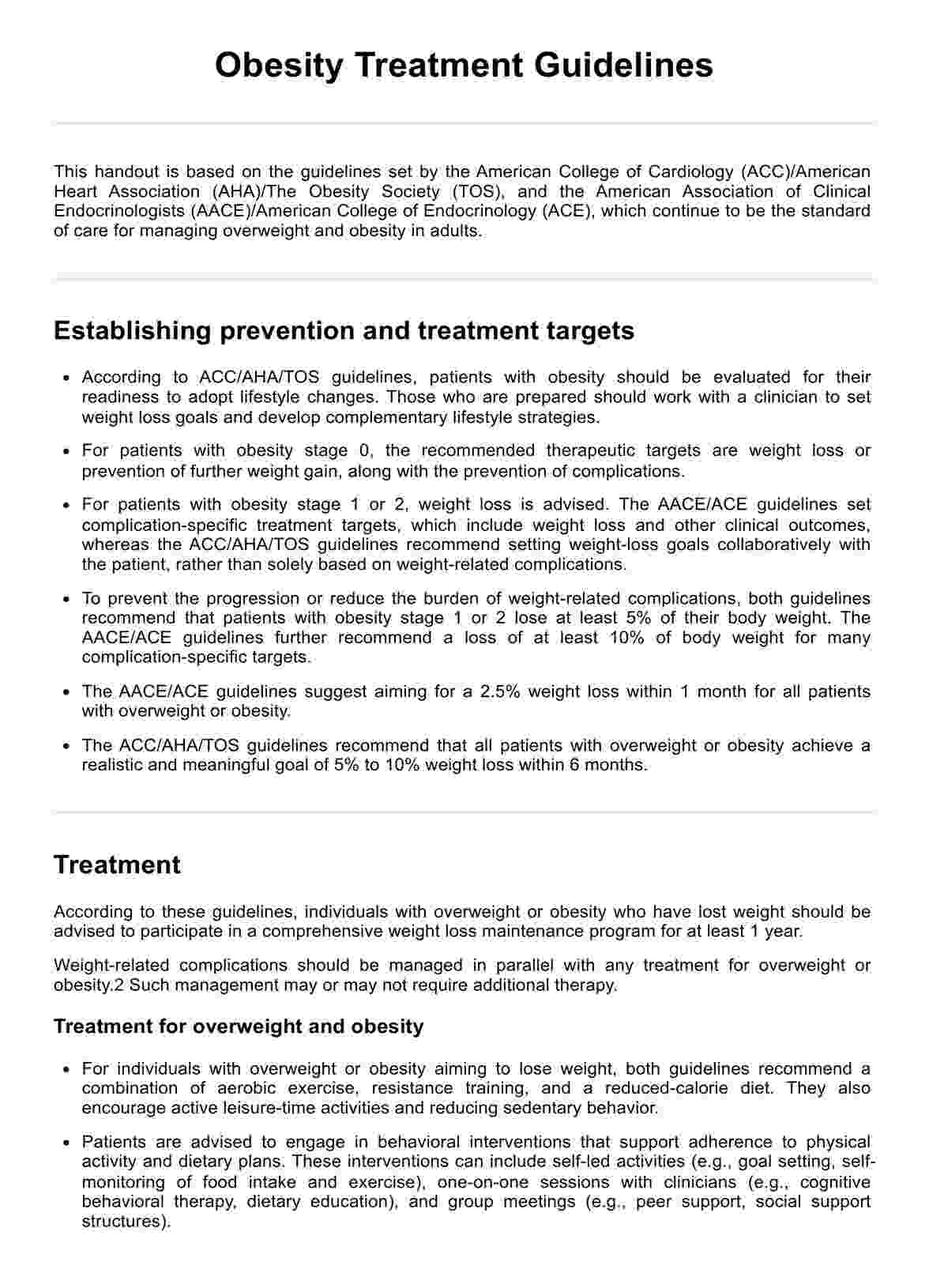
Common skin conditions
Being the largest organ of our body, the skin is susceptible to various conditions that can affect its appearance and function. Some common skin conditions include:
Acne
Acne is a skin condition when hair follicles become clogged with oil and dead skin cells, leading to whiteheads, blackheads, or pimples (National Institute of Arthritis and Musculoskeletal and Skin Diseases, n.d.). Hormonal changes, genetics, or certain medications can cause it.
Psoriasis
Psoriasis is an autoimmune disorder that causes the rapid buildup of skin cells, resulting in thick, red patches covered with silvery scales (National Institute of Arthritis and Musculoskeletal and Skin Diseases, n.d.). Stress, infections, or certain medications can trigger psoriasis.
Eczema
Eczema is a chronic skin condition characterized by dry, itchy patches of skin. It is commonly seen in people with allergies and can be triggered by irritants such as soaps, detergents, or stress.
Skin cancer
Skin cancer is the abnormal growth of skin cells, typically caused by exposure to UV radiation from the sun or tanning beds. It can manifest in different forms, such as basal cell carcinoma, squamous cell carcinoma, and melanoma.
Rosacea
Rosacea is a chronic skin condition characterized by persistent redness, flushing, and occasional development of pimples on the face (National Institute of Arthritis and Musculoskeletal and Skin Diseases, n.d.). It is a complex disorder influenced by various factors such as genetics, immune system dysfunction, and the presence of microscopic mites on the skin.
Hives
Hives are itchy, raised bumps on the skin that appear suddenly and can be triggered by allergic reactions, infections, or medications. They usually disappear within a few hours but can be recurring.
Warts
Warts are small, rough growths on the skin caused by the human papillomavirus (HPV). They can appear anywhere on the body and are often treated with topical medications or removal procedures.
Shingles
Shingles is a viral infection that causes a painful rash on one side of the face or body. The varicella-zoster virus causes it, the same virus that causes chickenpox. It is most common in older adults and people with weakened immune systems.
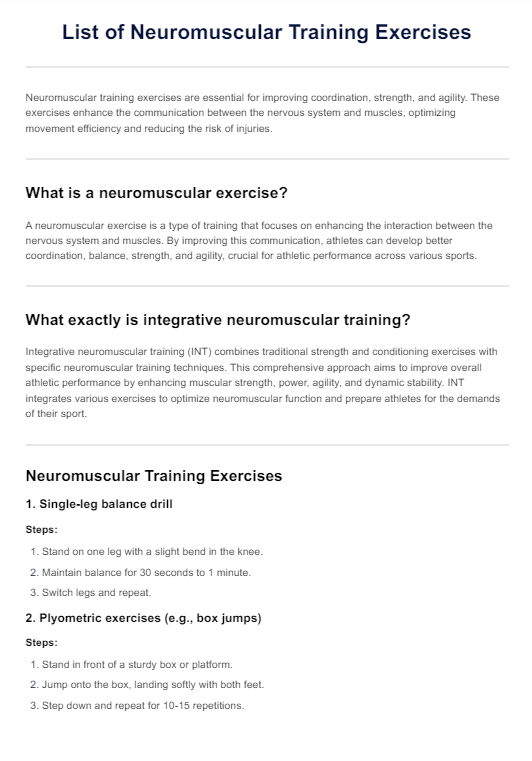
Why is a nursing skin assessment critical?
A comprehensive skin assessment lets you identify any changes or abnormalities in a patient's skin. This assessment is essential because the skin is the body's largest organ, acts as a barrier against infection, regulates body temperature, and senses touch, pain, and pressure.
Any issues with the skin can indicate underlying health problems that need to be addressed promptly. Moreover, skin assessments are crucial in detecting and preventing pressure ulcers for patients who are immobile or have limited mobility.
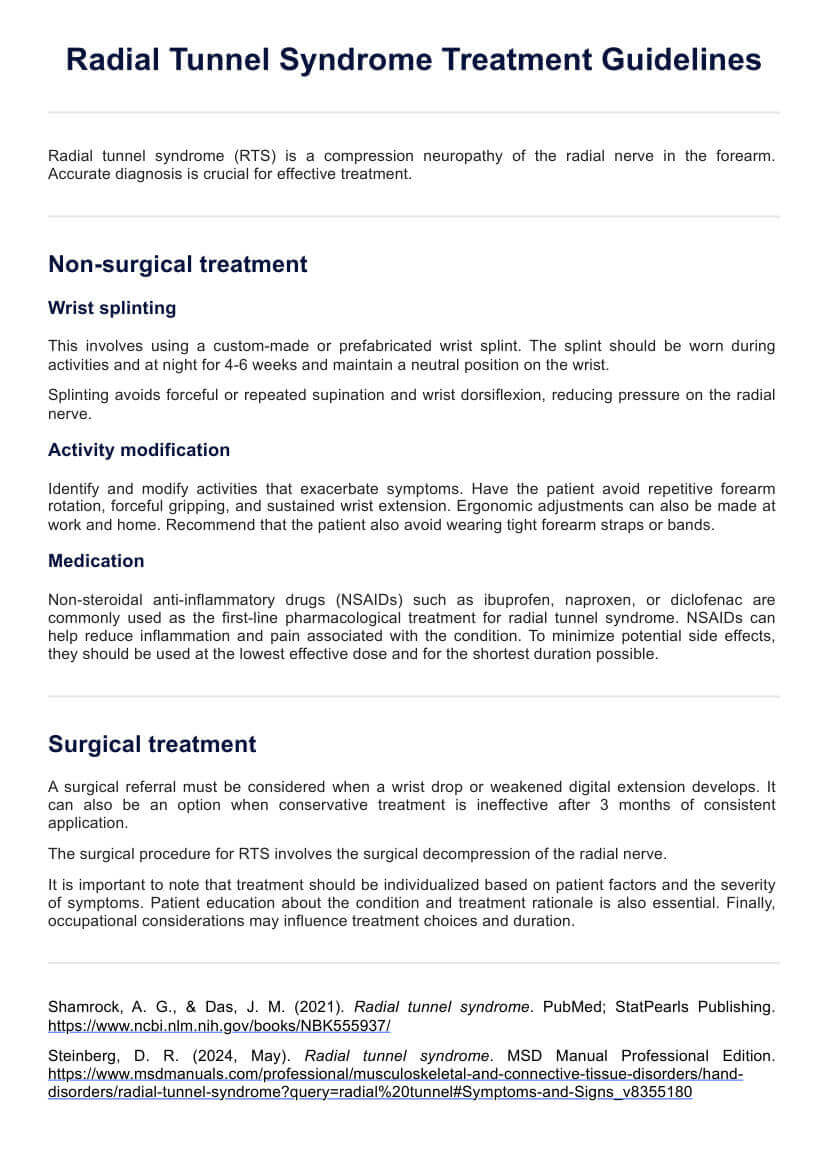
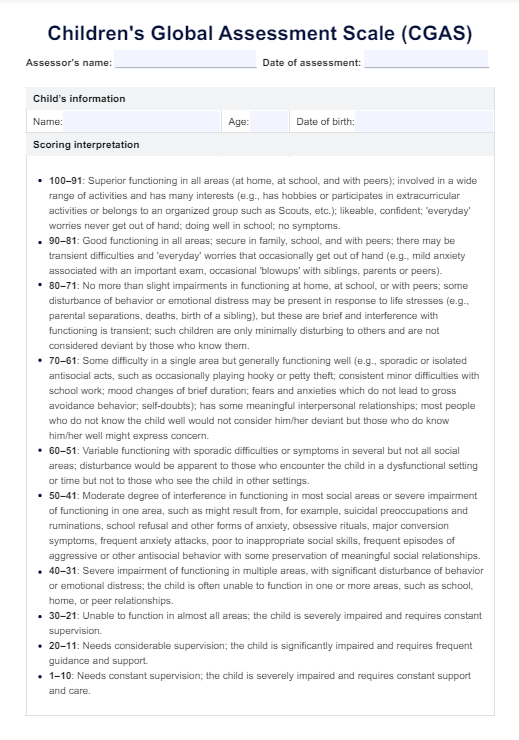
What does a Nursing Skin Assessment Checklist include?
Carepatron's free template makes it easy to ensure you are performing a comprehensive skin assessment correctly. The checklist includes the following items:
- Confirm patient identification
- Assess known skin conditions
- Evaluate skin lesions and document findings accurately
- Assess pressure points for signs of breakdown
- Palpate skin temperature accurately, noting any differences in temperature between areas.
- Check for decreased skin elasticity or skin turgor
- Evaluate skin color, noting any changes or abnormalities
- Assess for skin breakdown, including wounds and pressure ulcers
- Observe skin folds for any signs of irritation or infection
Using Carepatron's free template in your practice
Here's how to get started with Carepatron's free nursing skin assessment form:
Step 1: Download the template
Get a copy of the free template using the link on this page or via the Carepatron app. You can also download it from our resources library.
Step 2: Perform a focused integumentary assessment
A focused integumentary assessment is essential when performing a comprehensive skin assessment. This includes assessing the patient's skin for abnormalities like lesions, rashes, or discoloration.
Step 3: Check for changes in skin temperature
Skin temperature can be an indicator of circulation and overall health. While performing your skin assessment, gently grasp the skin and compare temperatures in different body areas. Be sure to note any temperature differences, which can provide valuable insights into the patient's overall health.
Step 4: Assess for safety measures
Assessing the patient's skin includes assessing their safety. This involves checking for any potential pressure points or areas of skin breakdown. Ensure that you confirm the patient's identity and any known skin conditions before proceeding with the assessment.
Step 5: Use proper techniques for assessing skin conditions
When evaluating skin lesions, ensure you are using proper physical examination techniques. This includes appropriately measuring wounds with a wound-measuring tool and gently palpating the lesion to determine its texture, size, and associated symptoms. This will help accurately document the patient's skin condition and assist in creating a care plan.
Step 6: Assess for decreased skin elasticity
The skin's elasticity decreases as we age, making it more prone to breakdowns and pressure ulcers. During your assessment, gently pinch the skin on different areas to assess its elasticity. If you notice any decreased skin elasticity, document it and take appropriate measures to prevent further breakdown.
Step 7: Monitor for changes in skin color
Skin color changes can indicate various potential health issues, including circulation problems or underlying diseases. As part of your comprehensive skin assessment, closely monitor the patient's skin color for any changes. Document and report any abnormal findings to the appropriate healthcare team members.
Step 8: Consider the patient's cues
Paying attention to your patient's cues during the skin assessment is crucial. They may express discomfort or sensitivity in certain areas, which could indicate underlying issues with their skin health.
Step 9: Discuss results with your patient
After completing the skin assessment, take the time to discuss your findings with the patient. This can help them become more aware of their skin health and any potential issues requiring further attention. You can also review proper skincare practices and provide education on maintaining healthy skin.
Nursing Skin Assessment checklist example (sample)
The Carepatron team has created a sample completed assessment form to guide you. Please note that this is just an example created for educational purposes only.
Download this free Nursing Skin Assessment Checklist example:

When would you use this form?
You can use this nursing skin assessment checklist at any point during a patient's care, including:
Upon admission to the healthcare facility or unit
Our free skin assessment checklist is a fantastic tool for admitting a patient. It helps establish a baseline for the patient's skin health upon arrival and allows continuous monitoring.
During routine check-ups or regular intervals
A comprehensive skin assessment should be performed regularly as part of routine care. This process can help identify changes in skin integrity, pressure points, or other potential issues early on.
When the patient presents with skin concerns or symptoms
In addition to regular assessments, a focused integumentary assessment should be conducted if the patient is experiencing any skin-related symptoms such as rashes, lesions, or changes in skin temperature.
During discharge planning
You can also use the template as part of the discharge process to ensure that any skin conditions or concerns are addressed before the patient leaves your care.
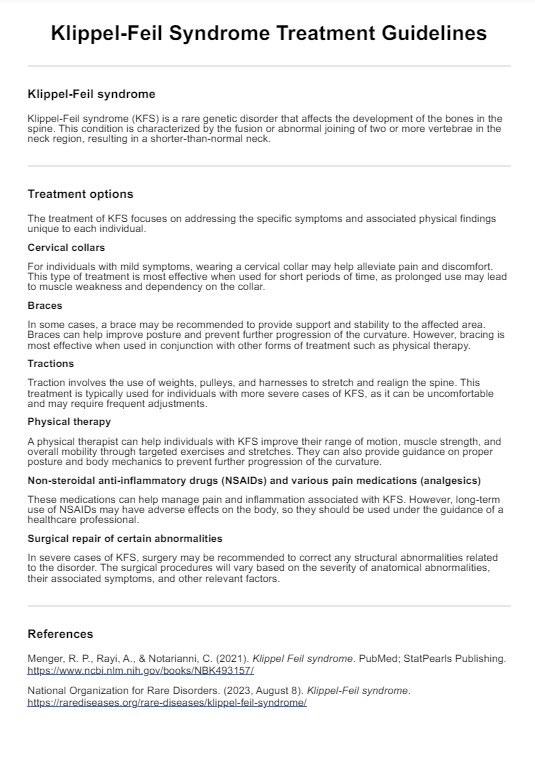
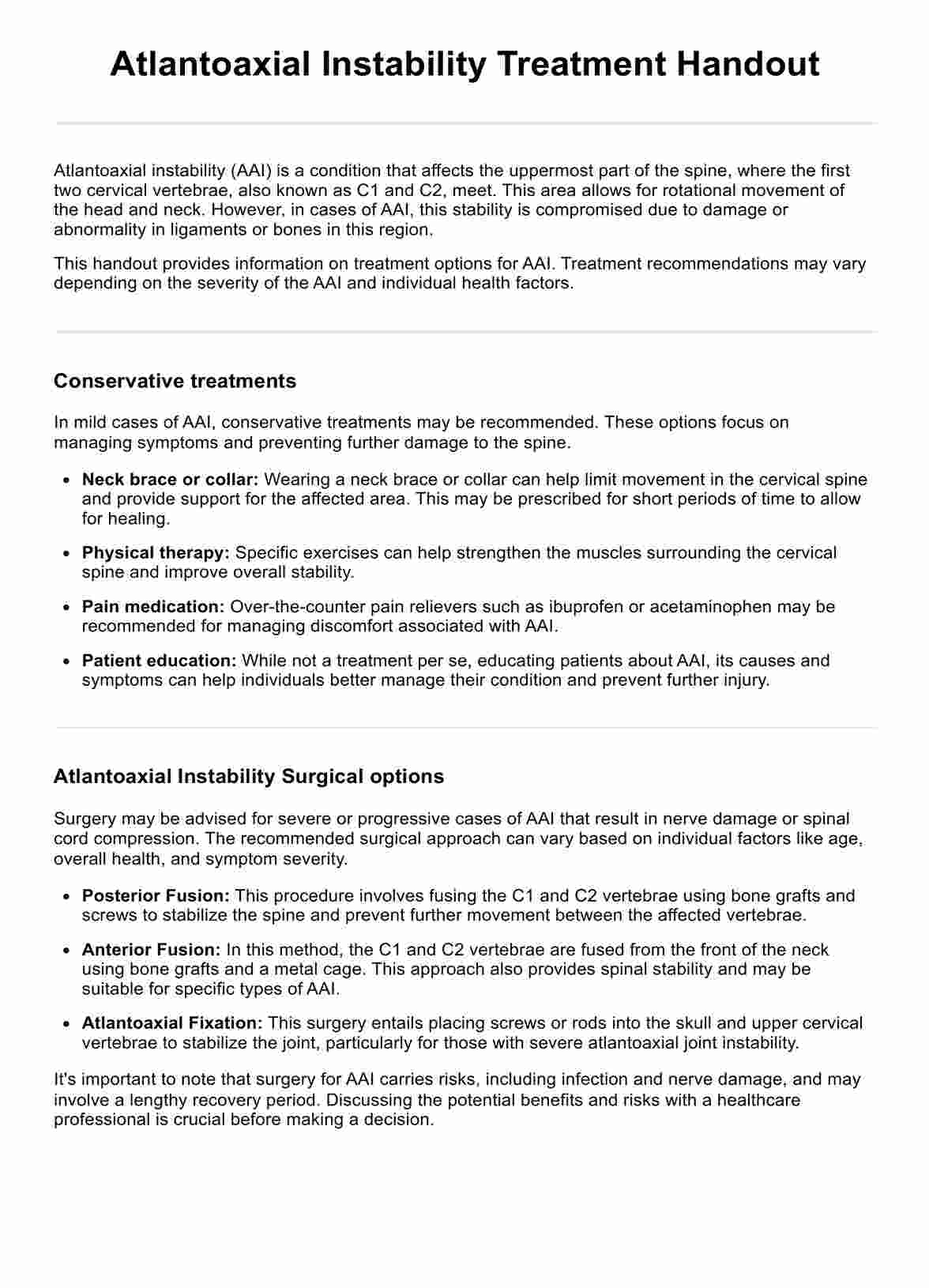
Other tests and tools for skin assessment
While this nursing skin assessment checklist provides a comprehensive overview of a patient's skin health, there are other tests and tools you may use to evaluate the condition further. These include:
Skin-fold measurement calipers
For patients with excess fatty tissue, using calipers to measure skin folds can provide insight into the patient's overall body composition and potential risk for pressure ulcers.
Braden Scale
The Braden Scale is a widely used tool for predicting pressure ulcer risk. This assessment examines six criteria: sensory perception, moisture, activity level, mobility, nutrition, and friction/shear.
Norton Scale
Like the Braden Scale, the Norton Scale is another tool used to assess a patient's risk for pressure ulcers. It evaluates five areas: mental state, physical condition, activity level, mobility, and incontinence.
Wound measuring tools
For patients with existing wounds or skin breakdowns, using wound measuring tools can help track healing progress and identify any changes in size or depth.
Waterlow Scale
This comprehensive scale assesses a patient's risk for developing pressure ulcers by considering crucial factors such as their age, weight, and overall health status.
Subcutaneous fat layer testing
This test involves gently grasping the skin in different areas of the body to measure the thickness of the subcutaneous fat layer. A thinner layer may indicate decreased skin elasticity and a higher risk of pressure ulcers.
Next steps: Keeping the skin healthy
A comprehensive skin assessment is crucial for identifying potential issues and developing a care plan. However, taking proactive steps to maintain skin health is equally important. Here are some ways you can support your patients in maintaining healthy skin:
- Encourage patients to maintain good hygiene practices, including regular bathing and keeping skin folds clean and dry.
- Promote adequate nutrition to support healthy skin. A well-balanced diet with sufficient protein intake can help improve overall skin health.
- Ensure safety measures are in place to prevent falls or injuries that could lead to skin breakdowns.
- Use pressure-relieving devices on areas prone to pressure ulcers, such as the heels or sacrum.
- Keep patients well-hydrated to support skin turgor and prevent dehydration-related skin issues.
- Educate patients on proper body positioning techniques to avoid prolonged pressure on any one area of the body.
- Use skin assessment forms to monitor for changes in skin temperature, texture, or color and evaluate new skin lesions.
Why use Carepatron as your Nursing app?
Don't let administrative tasks take away from the invaluable time you could spend on patient care.
With Carepatron, you'll have a nursing practice management app that streamlines your workflow, enhances patient management, and ensures seamless communication with your care team. By leveraging our user-friendly interface, you can prioritize what truly matters - providing high-quality patient-centered care.
From scheduling appointments to managing electronic health records, Carepatron empowers you to focus on your patients' needs while eliminating the hassle of manual paperwork.
So why wait? Take a step towards revolutionizing your nursing practice today. Join the thousands of satisfied healthcare professionals who trust Carepatron with daily operations. Start now and experience the difference firsthand.
With Carepatron, providing excellent care has never been more straightforward!
References
Cleveland Clinic. (n.d.). Skin. Cleveland Clinic. https://my.clevelandclinic.org/health/body/10978-skin
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (n.d.). Acne. NIAMS.https://www.niams.nih.gov/health-topics/skin-diseases
Yousef H, Alhajj M, Sharma S. (2022, November 14). Anatomy, Skin (Integument), Epidermis. In StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK470464/
Commonly asked questions
To record a comprehensive skin assessment, use a nursing skin assessment checklist. This tool ensures that all essential areas are thoroughly evaluated and documented accurately.
To prepare your patient for a focused integumentary assessment, confirm patient information and any known skin conditions or allergies. Also, ensure safety measures are in place before starting the evaluation.
A skin analysis can take between 5 and 15 minutes, depending on the complexity of the patient's skin condition and any additional assessments that need to be conducted.