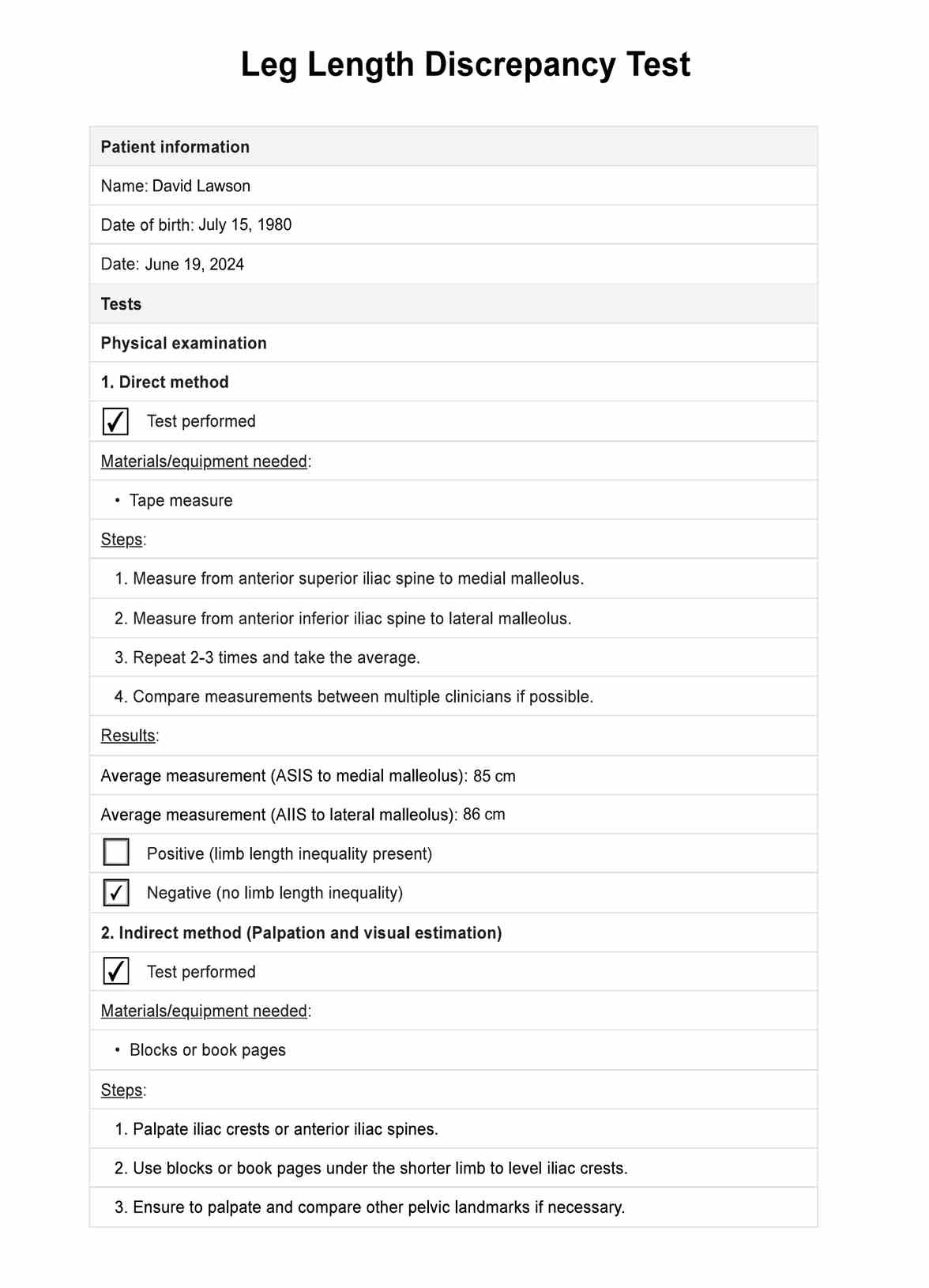
It is diagnosed through physical examinations, measurements of leg lengths from hip to ankle, and imaging tests like X-rays or MRIs to confirm the extent of the discrepancy.
Leg Length Discrepancy Test
Discover the Leg Length Discrepancy Test: Measure and address differences in leg length for better patient outcomes. Download our free PDF guide now.
Leg Length Discrepancy Test Template
Commonly asked questions
Radiographic measurements are generally considered the most precise method to assess leg length discrepancies accurately.
The best imaging modality for accurately assessing leg length discrepancy (LLD) is full-length standing anteroposterior radiography, also known as a scanogram or orthoroentgenogram. Compared to other imaging modalities like CT or MRI, scanograms provide the necessary full-length visualization of the lower limbs while minimizing radiation exposure and cost.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











