Acute Confusion Nursing Care Plan
Optimize patient care with our Acute Confusion Nursing Care Plan template to streamline assessment, intervention, and management for optimal outcomes.


What is acute confusion?
Acute confusion, also known as delirium, is a sudden onset of cognitive impairment that affects a patient's consciousness, attention, cognition, and perception. It can develop over hours to days and is often reversible once the underlying cause of medical illness is identified and treated. It is a condition frequently encountered in clinical practice, particularly among elderly patients, and requires prompt assessment and intervention to prevent complications and promote client safety.
Symptoms of acute confusion (patient report)
Patients experiencing acute confusion may report a variety of symptoms that indicate cognitive dysfunction, mood disorders, and altered mental status. These symptoms include:
- Patients may see, hear, or feel things that are not present
- A heightened sense of suspicion or fear of others
- Confusion about time, place, or identity
- Feelings of restlessness and inability to stay calm
- Difficulty remembering recent events or information
Signs of acute confusion (nurse's observations)
Health professionals, particularly nurses, identify and monitor these vital signs of acute confusion:
- Inconsistent awareness levels, ranging from alertness to drowsiness
- Physical signs of distress include fidgeting or attempting to get out of bed
- Misinterpretation of environmental stimuli, such as mistaking medical equipment for threats
- Challenges in understanding or completing tasks
- Involuntary shaking or trembling is often observed in the hands
Causes of acute confusion
Here are some probable causes of acute confusion:
- Infections, particularly urinary tract infections (UTIs) and sepsis are prevalent in elderly patients
- Sudden cessation of alcohol intake can lead to withdrawal symptoms and delirium
- Injuries to the head can disrupt cognitive function and lead to altered mental status
- Certain medications, such as anticholinergics, can induce delirium, highlighting the importance of proper medication management
- Electrolyte disturbances, hypoglycemia, and dehydration can impair cognitive function
- Postoperative confusion is common, especially in older adults
- Pre-existing conditions such as dementia, Parkinson's disease, and other mental disorders increase the risk of delirium
- Interaction of multiple medications can lead to adverse cognitive effects, necessitating careful review and adjustment of the patient's medication regimen
Understanding these underlying causative factors is essential for effective treatment and management
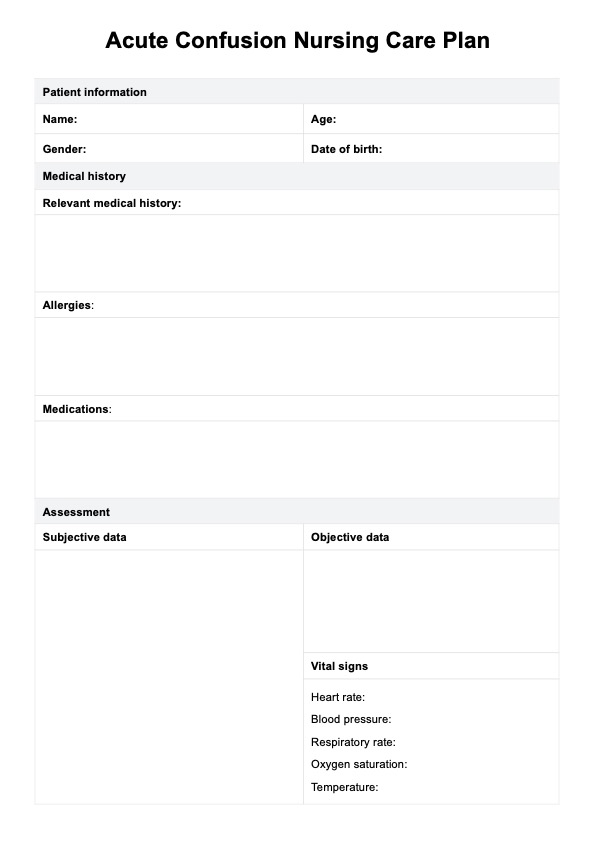
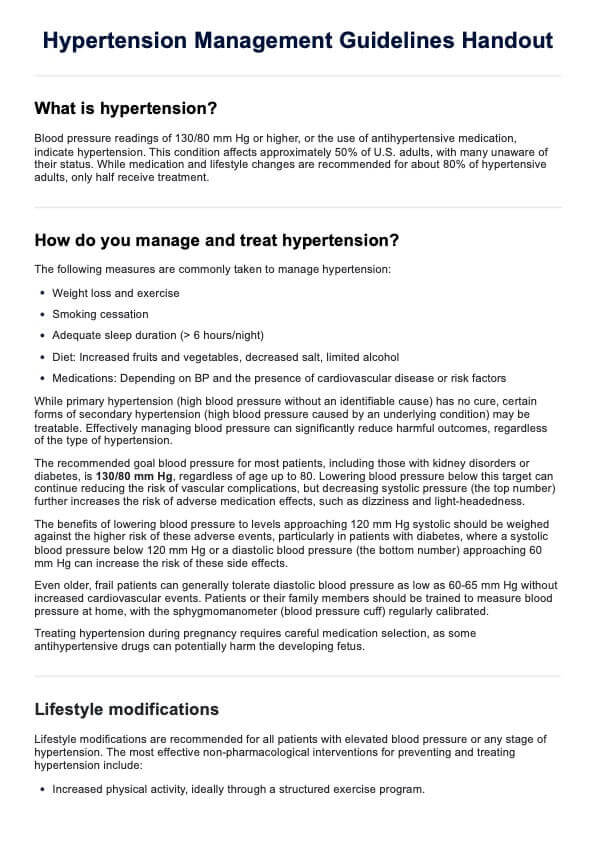
Acute Confusion Nursing Care Plan Template
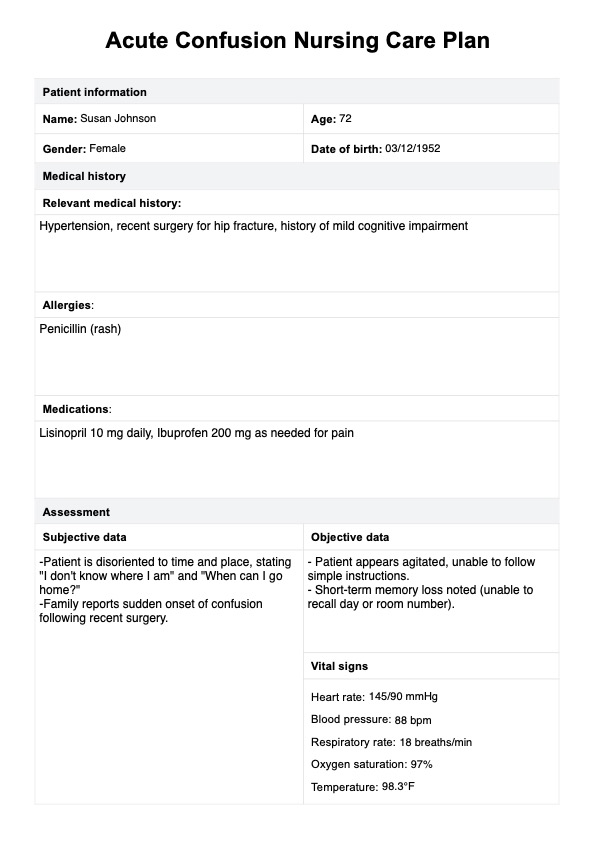
Acute Confusion Nursing Care Plan Example
What is an Acute Confusion Nursing Care Plan template?
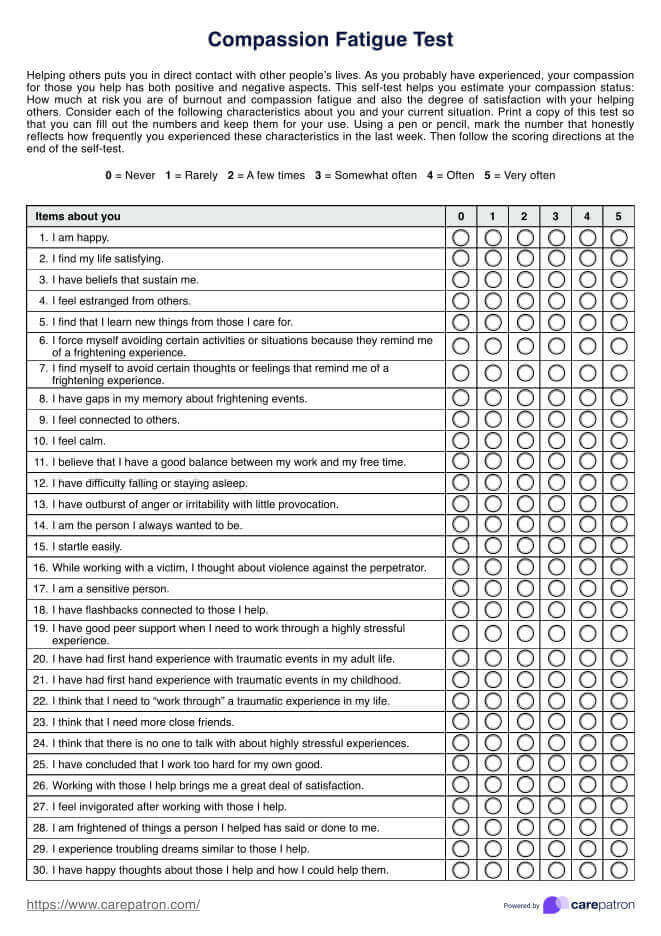
An Acute Confusion Nursing Care Plan helps healthcare providers manage acute confusion, sudden confusion, or disorientation in patients. Acute confusion can result from multiple risk factors, such as infections, medications, dehydration, trauma, or electrolyte imbalances. This care plan emphasizes a thorough confusion assessment, using tools like the Confusion Assessment Method to evaluate the patient's mental status and pinpoint contributing factors.
This nursing care plan for acute confusion guides interventions to manage and safeguard patient well-being and restore cognitive function by addressing risk factors and employing safety measures. Monitoring vital signs, adjusting medications, and utilizing hearing aids when necessary are key strategies for enhancing the patient's orientation and reducing the increased risk of disorientation.
How to use the Acute Confusion Nursing Care Plan template
Following these steps ensures healthcare professionals have a structured, effective approach to managing acute confusion and supporting patient recovery:
Step 1: Download this template
Download the Acute Confusion Nursing Care Plan template to your device or print a physical copy for easy access during assessments and care planning.
Step 2: Fill in patient information
Enter the patient’s personal information, medical history, allergies, and current medications. This information provides essential context for understanding the patient’s risk factors and potential causes of acute confusion.
Step 3: Conduct a comprehensive assessment
Record subjective data (patient’s reported symptoms) and objective data (observed symptoms), and take vital signs. Evaluate also the mental status and identify any physical factors, such as hearing aid needs, that could affect orientation.
Step 4: Develop nursing diagnosis, goals, and interventions
Formulate the primary nursing diagnosis for acute confusion and establish both short-term and long-term goals. Outline specific interventions, including safety measures and reorientation techniques, to address and experience acute confusion and ensure patient safety.
Step 5: Evaluate and update
Assessing the care plan’s effectiveness involves reviewing patient progress to see if goals are being met, identifying any obstacles, and determining if adjustments are needed. Based on the evaluation, interventions may be modified to better support the patient's needs, ensuring the care plan remains responsive and effective.
How nurses assess and diagnose acute confusion
The following can help bring clarity to the often-clouded presentation of acute confusion:
Initial patient assessment
The first step in assessing acute confusion is a thorough patient assessment. As part of the nursing process, ask about symptoms like hallucinations, paranoia, and memory issues. Observe for fluctuating cognition, agitation, inappropriate perceptions, and physical symptoms like tremors.
Review of medical history
Look for predisposing factors such as age over 60, pre-existing dementia, history of alcohol or substance abuse, recent surgery, and chronic diseases. Assess current and recent medications for potential side effects that could contribute to delirium, including interactions between drugs.
Physical examination
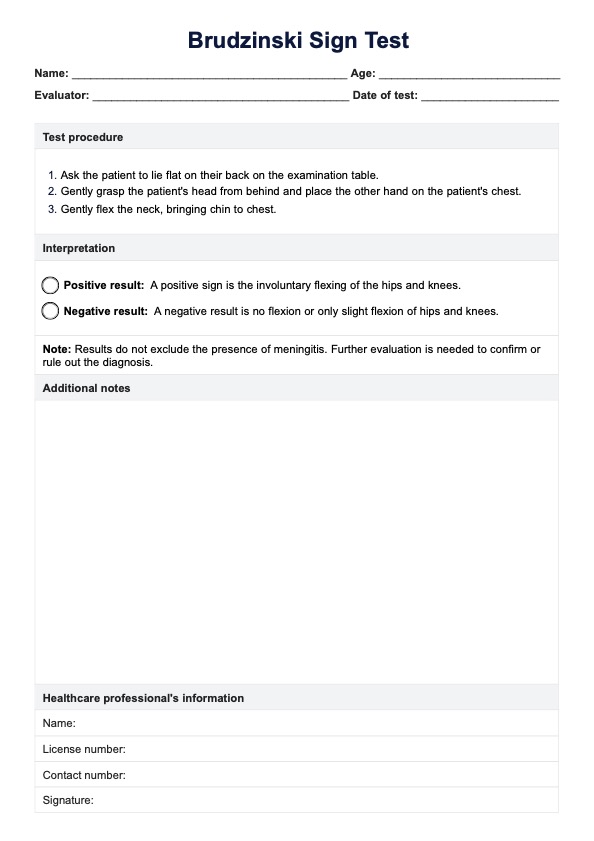
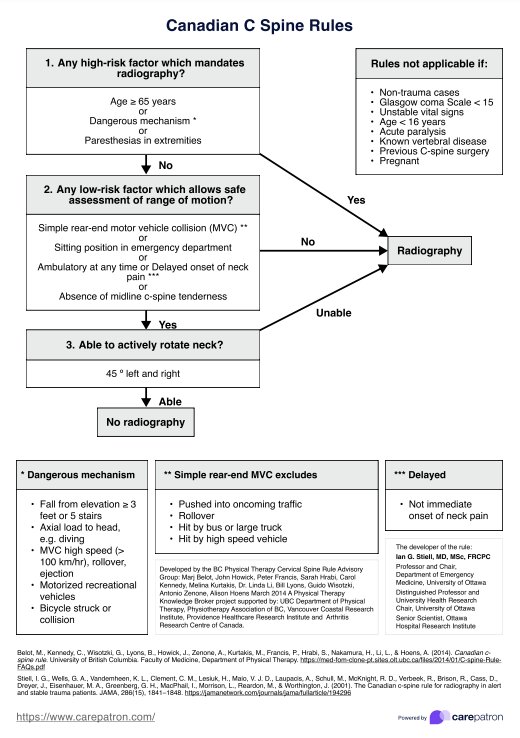
Conduct a physical exam to identify any physiological causes of acute confusion. Monitor temperature, pulse, blood pressure, respiratory rate, and oxygen saturation. Evaluate the patient's neurological and functional status throughout, including level of consciousness and cognitive function.
Use of diagnostic tools
Several standardized tools can help in the acute confusion of nursing diagnoses. Here are three of them:
- Confusion assessment method (CAM): This tool is widely used for its reliability in detecting delirium through features like acute onset, inattention, disorganized thinking, and altered level of consciousness.
- Nursing delirium screening scale (Nu-DESC): Useful for quick screening, especially in intensive care units and other clinical settings.
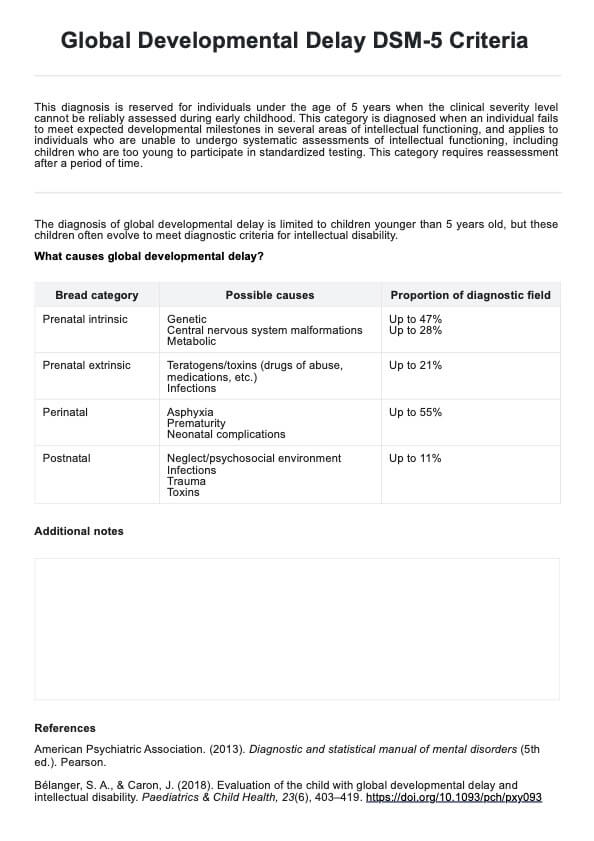
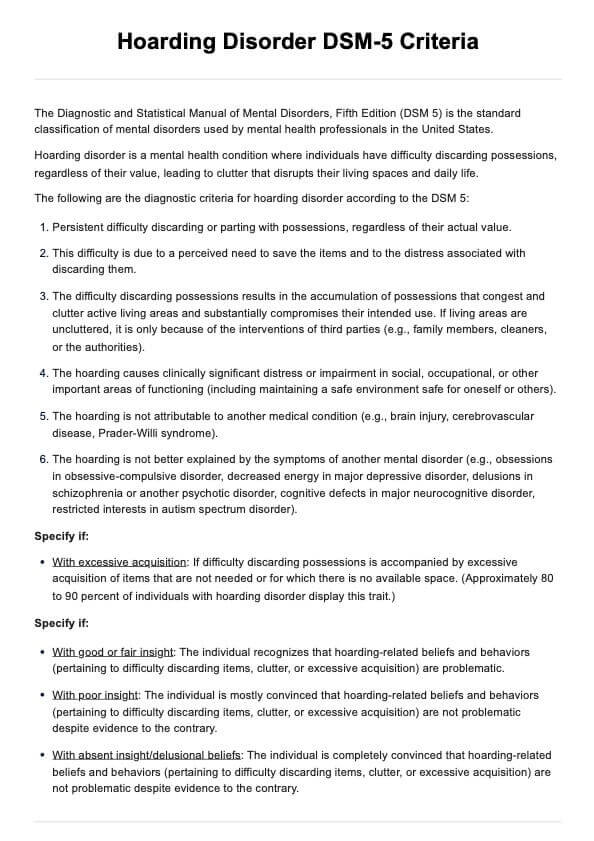
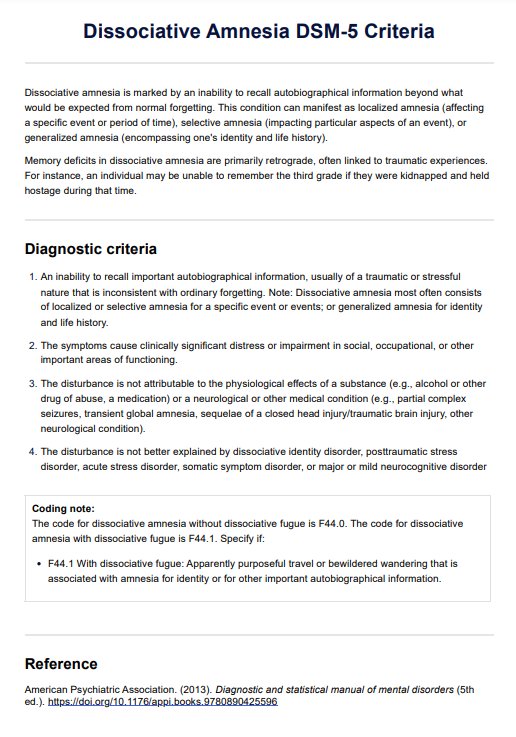
- Diagnostic and statistical manual (DSM-5) criteria: Refer to the DSM-5 criteria to differentiate delirium from other mental disorders.
Laboratory and diagnostic tests
Check for infections, metabolic imbalances, and renal function. Detect urinary tract infections and consider imaging studies if neurological brain imaging concerns exist.
Common nursing interventions for acute confusion
Here are five common nursing interventions for patients' recovery and managing acute confusion:
- Frequent orientation: It is crucial to regularly reorient the patient to time, place, and person. Use clocks, calendars, and personal items to help ground them in reality.
- Environmental modifications: Creating a calm and well-lit environment with minimal noise and distractions can significantly reduce confusion and agitation. Ensuring the patient's room is safe by removing hazards and providing clear pathways helps prevent falls and injuries.
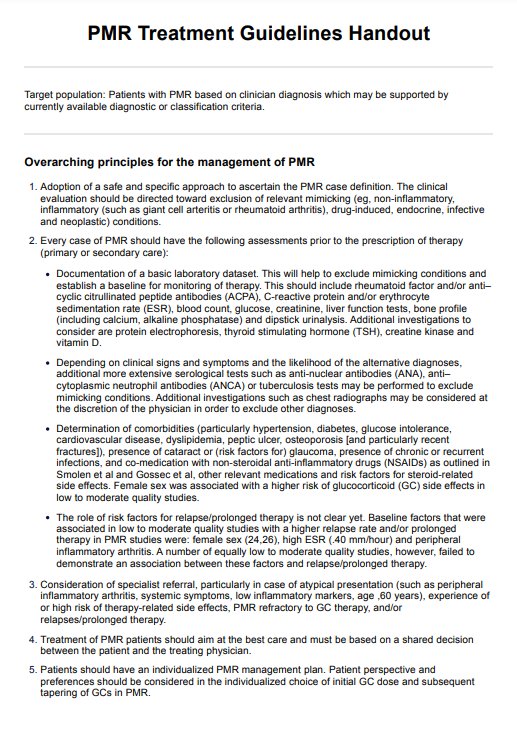
- Medication management: Reviewing and administering medications as prescribed is essential, especially avoiding those that can exacerbate confusion. Monitoring for side effects and interactions that may contribute to acute confusion is vital, and any concerns should be promptly reported to the healthcare provider.
- Promoting sleep and rest: Establishing a regular sleep routine is important. This can be achieved by encouraging daily activities and creating a restful nighttime environment.
- Hydration and nutrition: Ensuring the patient receives adequate fluids and balanced nutrition supports overall health and cognitive function.
Remember to always tailor interventions to the patient's needs.
Commonly asked questions
Acute confusion can result from a complex and interconnected process involving various factors such as head trauma, drug-induced delirium, infections, or disruptions in the central nervous system. Environmental factors, such as unfamiliar surroundings or sleep deprivation, may also contribute.
A registered nurse can create a calm environment and ensure familiar objects surround the patient to reduce disorientation. They also work closely with family members to support orientation and cognitive stimulation to reduce illogical thinking.
Family members can play a crucial role by providing comfort, bringing familiar objects, and helping to reduce confusion. Their presence can help confused patients feel more secure and reduce the stress that may worsen confusion symptoms.