During the Gaze Stabilization Test, a stable gaze is crucial for evaluating how well a patient can maintain visual focus while their head is in motion. This ability significantly correlates with physical performance and motor control, impacting daily activities and enhancing safety, especially in community-dwelling older adults. The gaze stability test is particularly important for patients with vestibular disorders as it reduces the risk of falls and improves overall mobility.
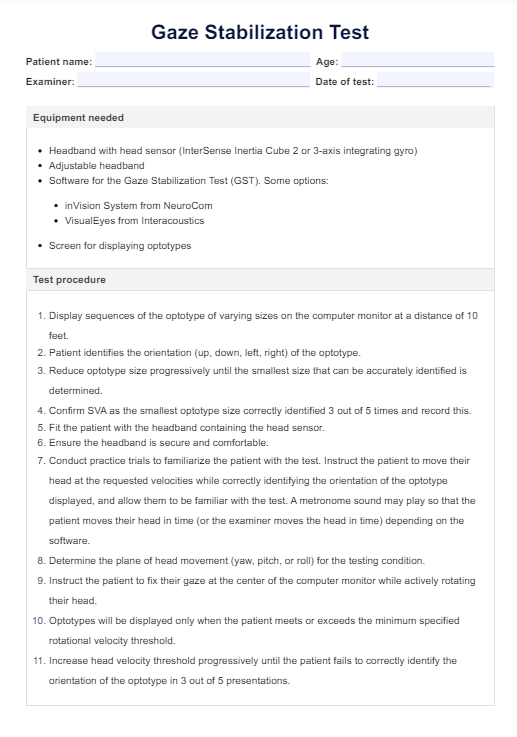
Gaze Stabilization Test
Explore our Gaze Stabilization Test guide. Learn how to assess and enhance vestibular health for better balance and mobility. Download our free PDF now!
Gaze Stabilization Test Template
Commonly asked questions
Unilateral vestibular disorders can significantly impact the results of a Gaze Stabilization Test by altering a patient's ability to maintain gaze stability, particularly when the head is turned towards the affected side. This can influence the diagnostic process and help formulate an effective treatment plan focusing on vestibular compensation and rehabilitation.
GST performance is significantly correlated with an individual’s ability to perform daily activities that require dynamic vision and balance. Tasks involving walking or navigating through crowded areas rely heavily on effective gaze stabilization to maintain orientation and stability, enhancing safe and independent living, especially among older adults. These insights are supported by studies measuring the gst velocity and functional measures related to gaze stability, which show significant correlations with everyday physical performance.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











