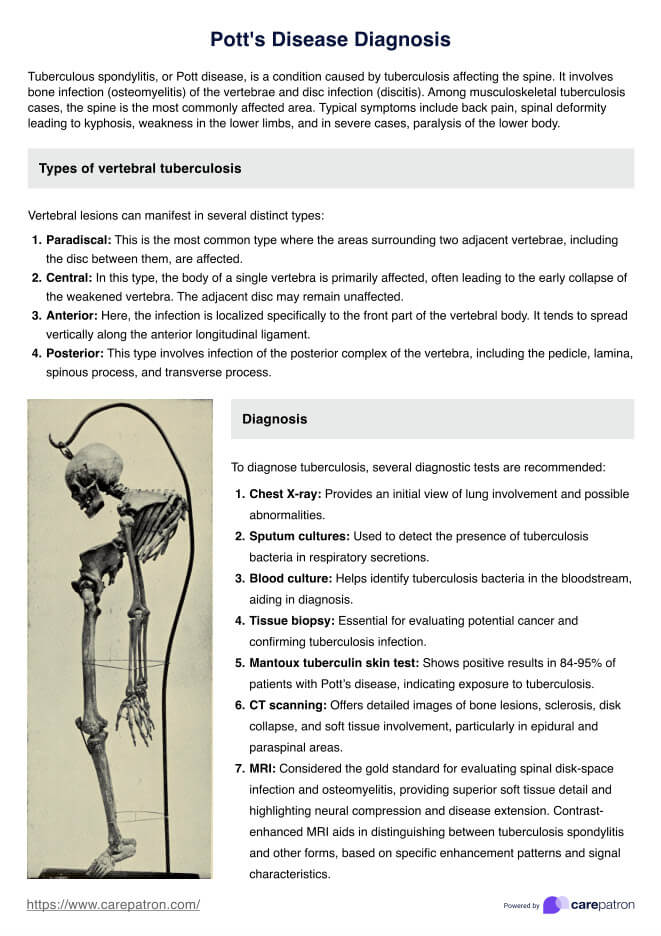
Symptoms of Pott's disease, or spinal tuberculosis, include persistent back pain, spinal deformity (kyphosis), fever, night sweats, weight loss, and sometimes neurological deficits.
Pott's Disease Diagnosis Guidelines
Learn about the guidelines and diagnosis criteria for Pott's Disease, along with an example, by downloading Carepatron's free PDF guide.
Use Template
Pott's Disease Diagnosis Guidelines Template
Commonly asked questions
Yes, Pott's disease can be cured with a combination of antitubercular medications taken for at least 6-9 months. Surgery may be necessary in severe cases.
Diagnosis involves clinical evaluation, imaging studies (X-rays, MRI, CT scans), and laboratory tests (blood tests, biopsy) to confirm the presence of Mycobacterium tuberculosis.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











