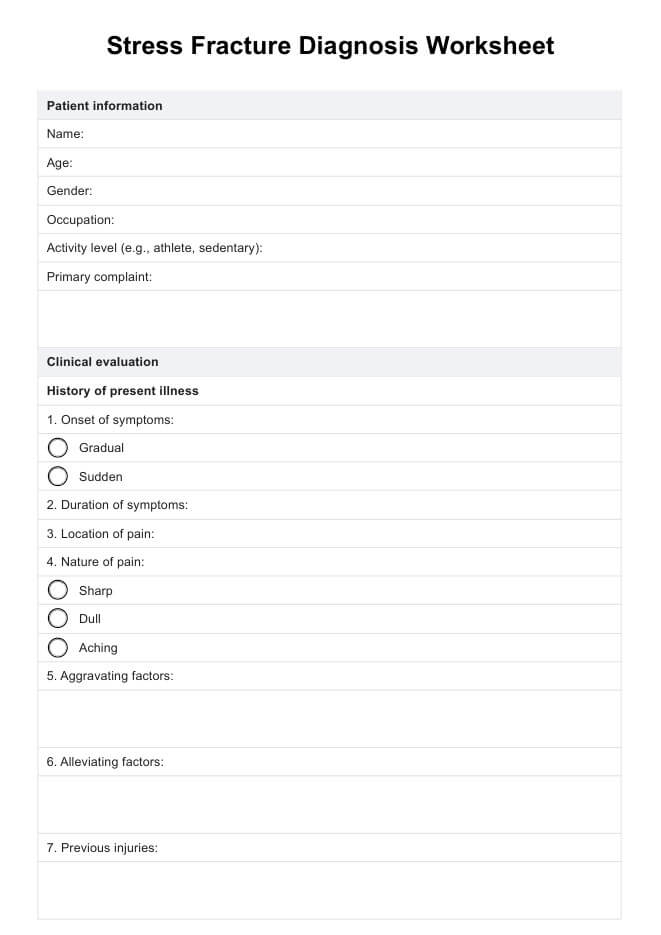
The worksheet is used to assess patients suspected of stress fractures systematically. It includes sections for patient history, physical examination findings, and imaging results to aid in diagnosis.
Stress Fracture Diagnosis Worksheet
Our Stress Fracture Diagnosis Worksheet aids healthcare professionals in thorough assessment and documentation for accurate diagnosis and treatment planning of stress fractures.
Use Template
Stress Fracture Diagnosis Worksheet Template
Commonly asked questions
Using the worksheet ensures a thorough evaluation, helping healthcare providers identify stress fractures early. It standardizes the diagnostic process, ensuring comprehensive care and accurate treatment planning.
The worksheet includes patient demographics, details of symptoms, risk factors, physical exam findings such as tenderness and swelling, and results from imaging tests like X-rays or bone scans.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











