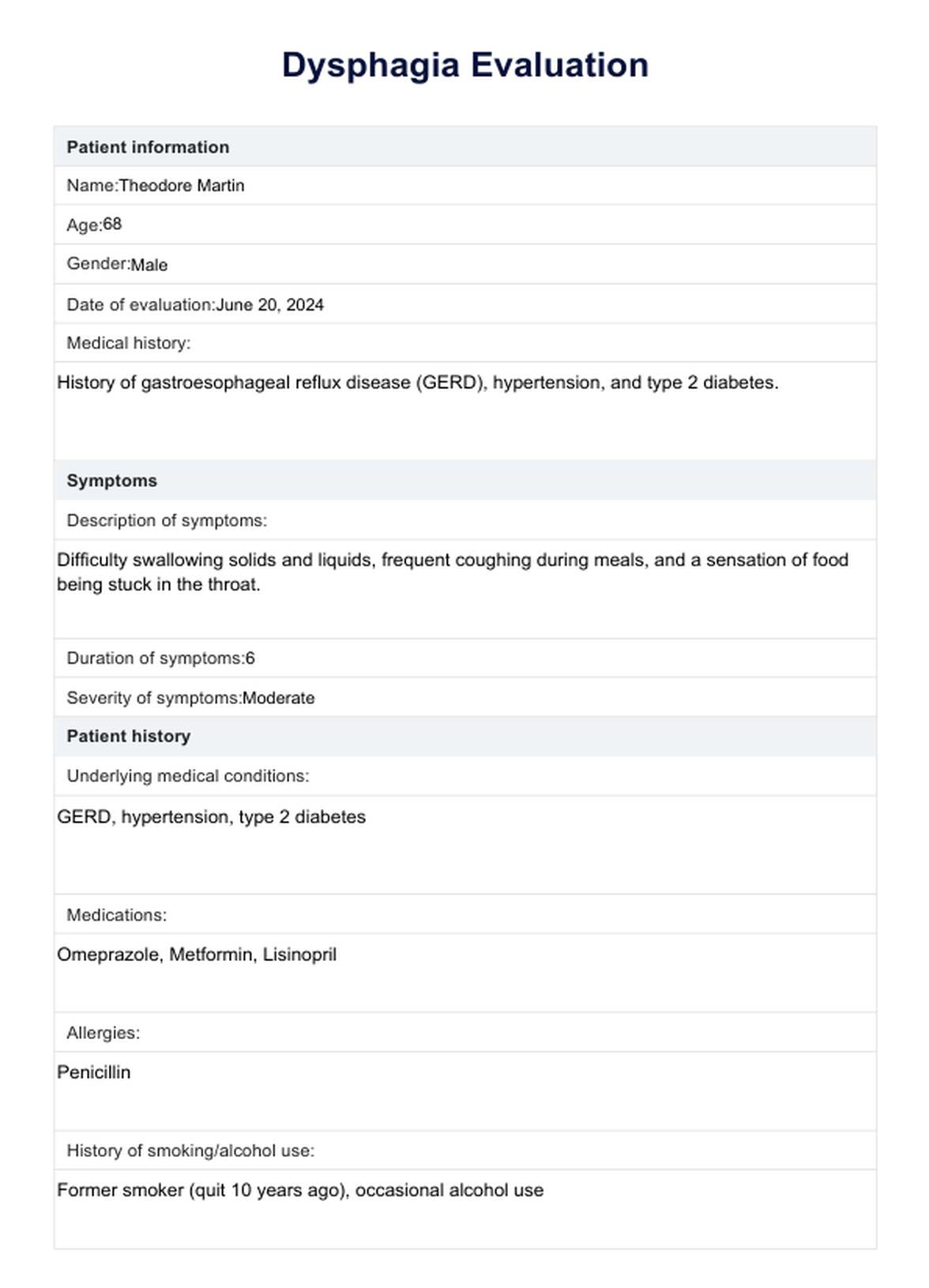
Dysphagia Evaluation
Learn about the importance of Dysphagia Evaluation and gain insights through Carepatron's free PDF download. Explore examples and tips for assessing swallowing difficulties.


What is dysphagia?
Dysphagia is a medical condition characterized by difficulty swallowing. It can affect people of all ages but is more prevalent among elderly patients. Dysphagia can result from various underlying causes, including gastroesophageal reflux disease (GERD), which often leads to esophageal inflammation and irritation.
Another cause is eosinophilic esophagitis, an allergic condition that can cause inflammation of the esophagus. Additionally, esophageal stricture, or narrowing of the esophagus, and motility disorders like diffuse esophageal spasm, which causes irregular muscle contractions, can contribute to swallowing difficulties.
Evaluating dysphagia involves a comprehensive assessment of the patient's swallowing mechanism. This swallowing evaluation is essential to identifying the specific cause of the dysphagia and developing an effective treatment plan. Common esophageal symptoms in dysphagia patients include a sensation of food being stuck, pain while swallowing, and regurgitation of food. The evaluation of dysphagia may consist of various diagnostic tests to assess the function of the upper esophageal sphincter and other parts of the esophagus.
Patients with dysphagia often require multidisciplinary care to manage their swallowing disorders effectively. Proper diagnosis and treatment are crucial to improving these patients' quality of life, especially those with severe swallowing difficulties.
Symptoms and causes of dysphagia
Symptoms of dysphagia vary widely but often include difficulty swallowing, a sensation of food being stuck in the throat or chest, pain while eating, and frequent regurgitation. Patients may also experience coughing or choking during meals, unexplained weight loss, and recurrent pneumonia due to aspiration.
The causes of dysphagia are diverse and can be classified into two main categories: oropharyngeal and esophageal. Oropharyngeal dysphagia is typically due to neurological disorders such as stroke, Parkinson's disease, or multiple sclerosis, which affect the muscles and nerves involved in swallowing. Esophageal dysphagia often results from structural abnormalities like esophageal stricture, gastroesophageal reflux disease (GERD), or motility disorders such as diffuse esophageal spasm.
Other causes include eosinophilic esophagitis, an allergic condition, and external compression from tumors or enlarged lymph nodes. Identifying the specific cause is essential for tailored treatment.
Dysphagia Evaluation Template
Dysphagia Evaluation Example
Types of dysphagia
Dysphagia can be categorized into several types, each with distinct causes and characteristics. Understanding these types is essential for accurately evaluating dysphagia and providing appropriate treatment.
Oropharyngeal dysphagia
Oropharyngeal dysphagia occurs when there is difficulty initiating the swallowing process in the oral cavity and throat. This type is often due to neurological disorders such as stroke, Parkinson's disease, or amyotrophic lateral sclerosis (ALS).
Symptoms include coughing, choking, or nasal regurgitation during swallowing. Evaluating dysphagia in these cases typically involves a thorough assessment of the muscles and nerves involved in the initial stages of swallowing.
Esophageal dysphagia
Esophageal dysphagia arises from problems within the esophagus itself. Common causes include esophageal motility disorders, such as diffuse esophageal spasm and ineffective esophageal motility, which disrupt the coordinated muscle contractions necessary for moving food down the esophagus.
Mechanical obstructions, like esophageal stricture or esophageal carcinoma, can also cause this type of dysphagia. The evaluation of dysphagia in these cases often involves endoscopic procedures and imaging studies to identify structural abnormalities.
Esophagogastric dysphagia
Esophagogastric dysphagia is characterized by difficulties at the junction between the esophagus and the stomach. This type often results from gastroesophageal reflux disease (GERD), which can cause inflammation and narrowing of this area or issues with the lower esophageal sphincter.
Symptoms include heartburn, regurgitation, and pain when swallowing. Proper Dysphagia Evaluation in these patients may involve pH monitoring and manometry to assess esophageal function and sphincter integrity.
Paraesophageal dysphagia
Paraesophageal dysphagia involves difficulty swallowing due to external pressure on the esophagus. Large hiatal hernias, tumors, or enlarged lymph nodes can cause this. Symptoms can mimic those of other types of dysphagia but often include additional chest pain and discomfort.
Evaluating dysphagia of this nature may require advanced imaging techniques like CT scans or MRI to visualize the structures exerting pressure on the esophagus.
How is a Dysphagia Evaluation conducted?
Conducting a Dysphagia Evaluation involves several key steps to accurately diagnose and address swallowing difficulties. Here are the typical steps involved:
- Patient history and interview: Gather detailed information about the patient's symptoms, medical history, and any recent changes in health or swallowing ability.
- Physical examination: Perform a thorough examination of the oral cavity, neck, and neurological function to identify any apparent abnormalities.
- Screening tests: Utilize essential screening tools, such as the water swallow test, to observe swallowing in a controlled setting.
- Videofluoroscopic swallow study (VFSS): Conduct a barium swallow study using X-rays to visualize the swallowing process and identify any structural or functional issues.
- Endoscopy: An endoscope is used to examine the esophagus and upper digestive tract directly for abnormalities such as strictures, tumors, or inflammation.
- Esophageal manometry: Measure esophageal pressure and muscle contractions to assess motility disorders.
- pH monitoring: Evaluate acid reflux and its impact on the esophagus, which can contribute to dysphagia.
- Dietary and swallowing assessments: Assess the patient's diet and swallowing capabilities to tailor dietary recommendations and therapeutic interventions.
These steps collectively help medical practitioners diagnose the cause of dysphagia and develop an effective treatment plan for patients.
Dysphagia treatments
Treating dysphagia involves a range of approaches tailored to the underlying cause and severity of the condition. Here are some common dysphagia treatments:
Dietary modifications
Dietary modifications are often the first step in managing dysphagia. This includes altering food textures and liquid consistency to make swallowing more accessible and safer. Patients might be advised to eat softer foods or use thickening agents for liquids to reduce the risk of aspiration and pulmonary complications.
Swallowing therapy
Swallowing therapy, typically conducted by a speech-language pathologist, focuses on exercises to strengthen the muscles involved in swallowing. This is particularly beneficial for patients with neurological disorders like myasthenia gravis.
Medications
Medications treat underlying conditions that contribute to dysphagia. For example, proton pump inhibitors (PPIs) can reduce acid reflux and inflammation of the esophageal mucosa in patients with gastroesophageal reflux disease (GERD).
Endoscopic procedures
Endoscopic procedures are essential for diagnosing dysphagia and treating structural issues. During endoscopy, practitioners can identify and sometimes treat conditions like mechanical obstruction or esophageal structures.
Surgical interventions
Surgical interventions may be necessary for severe cases of dysphagia caused by structural abnormalities or tumors. Surgery can correct anatomical issues, remove obstructions, or repair damage such as esophageal rupture. This approach is often considered when other treatments have failed to provide relief.
Commonly asked questions
Diagnostic tests for dysphagia may include a videofluoroscopic swallow study (VFSS), endoscopy, esophageal manometry, and pH monitoring to assess swallowing function, identify structural abnormalities, and evaluate esophageal motility and acid reflux.
The goal of dysphagia evaluation is to identify the underlying cause of swallowing difficulties, assess the severity of the condition, and develop an appropriate treatment plan to improve swallowing function and prevent complications.
The approach to diagnosing dysphagia involves a combination of patient history, physical examination, and diagnostic tests to evaluate swallowing function, identify potential causes, and guide treatment decisions based on the patient's specific needs.
Clinical indicators of dysphagia include difficulty swallowing, sensation of food sticking in the throat or chest, coughing or choking during meals, unexplained weight loss, recurrent pneumonia, and regurgitation of food or liquids. These symptoms may vary depending on the underlying cause and severity of dysphagia.